The Impact of Total Hip Arthroplasty on the Incidence of Hip Fractures in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Sources
2.2. Building the Model
- Population number (PO), for every gender (G) and age group (AG);
- Observed number of fractures (NO), for every gender (G) and age group (AG);
- Number of hip prostheses (NHP) for every gender (G) and age group (AG).
- Hip fracture rates in (BY) by sex and age group (r(BY)), as follows:r(BY) = NO/PO,
for every (G) and (AG);
- Considering the population size in the end year PO(EY) and the hip fracture rates in the baseline year (r(BY)), we calculated the expected number of hip fractures (NE) in (EY), as follows:NE(EY) = PO(EY) × (r(BY)),
for every (G) and (AG);
- We estimated the number of hip fractures requiring explanation, as the difference between the observed and expected number of hip fractures in (EY), as follows:NXestimated = NO(EY) − NE(EY),
for every (G) and (AG).
- We calculated the fracture incidence rate in a scenario without THA, as the ratio between the number of observed fractures and the population number from which we extracted 0.5 for each person living with hip prosthesis, as follows:rs = NO/(PO − 0.5 × NHP),
in (BY) and (EY), for every (G) and (AG);
- The number of hip fractures explained by the influence of hip prostheses factors is calculated as the product between the population size and the difference between the fracture incidence rate in scenario and the fracture incidence rate, as follows:NXexplained HP= PO(EY) × [(rs(EY) − r(EY)].
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xu, B.Y.; Yan, S.; Low, L.L.; Vasanwala, F.F.; Low, S.G. Predictors of poor functional outcomes and mortality in patients with hip fracture: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 568. [Google Scholar] [CrossRef]
- Giannoulis, D.; Calori, G.M.; Giannoudis, P.V. Thirty-day mortality after hip fractures: Has anything changed? Eur. J. Orthop. Surg. Traumatol. 2016, 26, 365–370. [Google Scholar] [CrossRef]
- Sing, C.W.; Lin, T.C.; Bartholomew, S.; Bell, J.S.; Bennett, C.; Beyene, K.; Bosco-Levy, P.; Bradbury, B.D.; Chan, A.H.Y.; Chandran, M.; et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J. Bone Miner. Res. 2023, 38, 1064–1075. [Google Scholar] [CrossRef]
- Kanis, J.A.; Odén, A.; McCloskey, E.V.; Johansson, H.; Wahl, D.A.; Cooper, C.; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 23, 2239–2256. [Google Scholar] [CrossRef]
- Borgström, F.; Karlsson, L.; Ortsäter, G.; Norton, N.; Halbout, P.; Cooper, C.; Lorentzon, M.; McCloskey, E.V.; Harvey, N.C.; Javaid, M.K.; et al. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 2020, 15, 59. [Google Scholar] [CrossRef]
- Veronese, N.; Maggi, S. Epidemiology and social costs of hip fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef]
- Feng, J.N.; Zhang, C.G.; Li, B.H.; Zhan, S.Y.; Wang, S.F.; Song, C.L. Global burden of hip fracture: The Global Burden of Disease Study. Osteoporos. Int. 2024, 35, 41–52. [Google Scholar] [CrossRef]
- Jing, H.; Chen, Y.; Liang, B.; Tian, Z.; Song, F.; Chen, M.; Kong, W.; Duan, Y. Risk factors for falls in older people with pre-frailty: A systematic review and meta-analysis. Geriatr. Nurs. 2025, 62 Pt A, 272–279. [Google Scholar] [CrossRef]
- Pabinger, C.; Lothaller, H.; Portner, N.; Geissler, A. Projections of hip arthroplasty in OECD countries up to 2050. Hip Int. 2018, 28, 498–506. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Valdes, K.; Pedersini, P.; Berjano, P. Osteoarthritis: A call for research on central pain mechanism and personalized prevention strategies. Clin. Rheumatol. 2019, 38, 583–584. [Google Scholar] [CrossRef]
- Iversen, M.D. Rehabilitation interventions for pain and disability in osteoarthritis. Am. J. Nurs. 2012, 112 (Suppl. 1), S32–S37. [Google Scholar] [CrossRef]
- Eethakota, V.V.S.; Vaishnav, V.; Johnston, L.; Abboud, R.; Wang, W. Comparison of revision risks and complication rates between total HIP replacement and HIP resurfacing within the similar age group. Surgeon 2018, 16, 339–349. [Google Scholar] [CrossRef]
- Național Institute of Statistics. Serii Istorice de date. Populatia Romaniei 1860–2020 (Historical Data Series. Population of Romania 1860–2020). Available online: https://insse.ro/cms/files/publicatii/Populatia-Romaniei/populatia-romaniei-1860-2020-serii-istorice-de-date.pdf (accessed on 6 June 2025).
- Național Institute of Statistics. Tempo Ins. Available online: https://insse.ro/cms/ro/content/pachetul-tempo (accessed on 6 June 2025).
- Eurostat Population Structure. Age Groups. Available online: https://ec.europa.eu/eurostat/documents/12743486/14207636/RO-RO.pdf (accessed on 6 June 2025).
- Populatia Romaniei (Romania’s Population). Available online: https://populatia.ro/ (accessed on 6 June 2025).
- Grigorie, D.; Sucaliuc, A.; Ciutan, M.; Vladescu, C. Incidence and time trend of hip fractures in Romania: A nationwide studyfrom 2008 TO 2018. Acta Endocrinol. 2019, 15, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Dobre, R.; Niculescu, D.A.; Cirstoiu, C.; Popescu, G.; Poiana, C. Osteoporotic Hip Fracture Incidence Rates in the Main Urban Area of Romania. Acta Endocrinol. 2021, 17, 60–67. [Google Scholar] [CrossRef]
- Sacu, C.; Ciutan, M. Analiza episoadelor de spitalizare determinate de osteoporoză în România în perioada 2008-2020 (Analysis of hospitalization episodes due to osteoporosis in Romania in the period 2008–2020). Health Manag. 2021, 4, 18–24. [Google Scholar]
- Romanian Arthroplasty Register. Available online: https://www.rne.ro/?lang=en (accessed on 6 June 2025).
- Kjeldgaard, H.K.; Meyer, H.E.; O’Flaherty, M.; Apalset, E.M.; Dahl, C.; Emaus, N.; Fenstad, A.M.; Furnes, O.; Gjertsen, J.E.; Hoff, M.; et al. Impact of Total Hip Replacements on the Incidence of Hip Fractures in Norway During 1999–2019. A Norwegian Epidemiologic Osteoporosis Studies (NOREPOS) Study. J. Bone Miner. Res. 2022, 37, 1936–1943. [Google Scholar] [CrossRef]
- Barendregt, J.J. The effect size in uncertainty analysis. Value Health 2010, 13, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. [Google Scholar] [CrossRef]
- Ballane, G.; Cauley, J.A.; Luckey, M.M.; Fuleihan, G.H. Secular trends in hip fractures worldwide: Opposing trends east versus west. J. Bone Miner. Res. 2014, 29, 1745–1755. [Google Scholar] [CrossRef]
- Formiga, F.; Freitez Ferreira, M.D.; Montero, A. Diabetes mellitus y riesgo de fractura de cadera. Revisión sistemática [Diabetes mellitus and risk of hip fracture. A systematic review]. Rev. Esp. Geriatr. Gerontol. 2020, 55, 34–41. (In Spanish) [Google Scholar] [CrossRef]
- Mortensen, S.J.; Mohamadi, A.; Wright, C.L.; Chan, J.J.; Weaver, M.J.; von Keudell, A.; Nazarian, A. Medications as a Risk Factor for Fragility Hip Fractures: A Systematic Review and Meta-analysis. Calcif. Tissue Int. 2020, 107, 1–9. [Google Scholar] [CrossRef]
- Beeram, I.; Mortensen, S.J.; Yeritsyan, D.; Momenzadeh, K.; von Keudell, A.; Nazarian, A. Multivitamins and risk of fragility hip fracture: A systematic review and meta-analysis. Arch. Osteoporos. 2021, 16, 29. [Google Scholar] [CrossRef]
- Mortensen, S.J.; Beeram, I.; Florance, J.; Momenzadeh, K.; Mohamadi, A.; Rodriguez, E.K.; von Keudell, A.; Nazarian, A. Modifiable lifestyle factors associated with fragility hip fracture: A systematic review and meta-analysis. J. Bone Miner. Metab. 2021, 39, 893–902. [Google Scholar] [CrossRef]
- Ackerman, I.N.; Bohensky, M.A.; de Steiger, R.; Brand, C.A.; Eskelinen, A.; Fenstad, A.M.; Furnes, O.; Graves, S.E.; Haapakoski, J.; Mäkelä, K.; et al. Lifetime Risk of Primary Total Hip Replacement Surgery for Osteoarthritis From 2003 to 2013: A Multinațional Analysis Using Național Registry Data. Arthritis Care Res. 2017, 69, 1659–1667. [Google Scholar] [CrossRef]
- Moldovan, F. New Approaches and Trends in Health Care. Procedia Manuf. 2018, 22, 947–951. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. An Investigation for Future Practice of Elective Hip and Knee Arthroplasties during COVID-19 in Romania. Medicina 2023, 59, 314. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Wang, Y.; Ge, L.; Pan, F.; Winzenberg, T.; Cai, G. Association of knee and hip osteoarthritis with the risk of falls and fractures: A systematic review and meta-analysis. Arthritis Res. Ther. 2023, 25, 184. [Google Scholar] [CrossRef]
- Johnsen, M.B.; Hellevik, A.I.; Småstuen, M.C.; Langhammer, A.; Furnes, O.; Flugsrud, G.B.; Nordsletten, L.; Zwart, J.A.; Storheim, K. The mediating effect of body mass index on the relationship between smoking and hip or knee replacement due to primary osteoarthritis. A population-based cohort study (the HUNT Study). PLoS ONE 2017, 12, e0190288. [Google Scholar] [CrossRef]
- Flugsrud, G.B.; Nordsletten, L.; Espehaug, B.; Havelin, L.I.; Engeland, A.; Meyer, H.E. The impact of body mass index on later total hip arthroplasty for primary osteoarthritis: A cohort study in 1.2 million persons. Arthritis Rheum. 2006, 54, 802–807. [Google Scholar] [CrossRef]
- Soh, S.E.; Barker, A.L.; Morello, R.T.; Ackerman, I.N. Applying the Internațional Classification of Functioning, Disability and Health framework to determine the predictors of falls and fractures in people with osteoarthritis or at high risk of developing osteoarthritis: Data from the Osteoarthritis Initiative. BMC Musculoskelet. Disord. 2020, 21, 138. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L.; Bataga, T. Assessment of Labor Practices in Healthcare Using an Innovatory Framework for Sustainability. Medicina 2023, 59, 796. [Google Scholar] [CrossRef]
- Național Institute of Statistics. Proiectarea Populaţiei României în Profil Teritorial, la Orizontul Anului 2060 (Projection of Romania’s Population in Territorial Profile, on the Horizon of 2060). Available online: https://insse.ro/cms/sites/default/files/field/publicatii/proiectarea_populatiei_romaniei_in_profil_teritorial_la_orizontul_2060.pdf (accessed on 6 June 2025).
- Barrionuevo, P.; Kapoor, E.; Asi, N.; Alahdab, F.; Mohammed, K.; Benkhadra, K.; Almasri, J.; Farah, W.; Sarigianni, M.; Muthusamy, K.; et al. Efficacy of Pharmacological Therapies for the Prevention of Fractures in Postmenopausal Women: A Network Meta-Analysis. J. Clin. Endocrinol. Metab. 2019, 104, 1623–1630. [Google Scholar] [CrossRef]
- Mikolajczyk, T.; Moldovan, L.; Chalupczak, A.; Moldovan, F. Computer Aided Learning Process. Procedia Eng. 2017, 181, 1028–1035. [Google Scholar] [CrossRef]
- Moldovan, L.; Gligor, A.; Grif, H.-S.; Moldovan, F. Dynamic Numerical Simulation of the 6-PGK Parallel Robot Manipulator. Proc. Rom. Acad. Ser. A 2019, 20, 67–75. [Google Scholar]
- Mikolajczyk, T.; Moldovan, F.; Ciobanu, I.; Chalupczak, A.; Georgiana Marin, A. Brain Research Using Computer Test. Procedia Technol. 2016, 22, 1113–1120. [Google Scholar] [CrossRef]

| Women | Men | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | Number of Hip Fractures (NO) | Population (PO) | Crude Fracture Rate per 10,000 (r) | Standardized Rate Fracture Rate per 10,000 (sr) | 95%CI | Number of Hip Fractures (NO) | Population (r) | Crude Rate Fracture Rate per 10,000 (PO) | Standardized Fracture Rate per 10,000 (sr) | 95%CI |
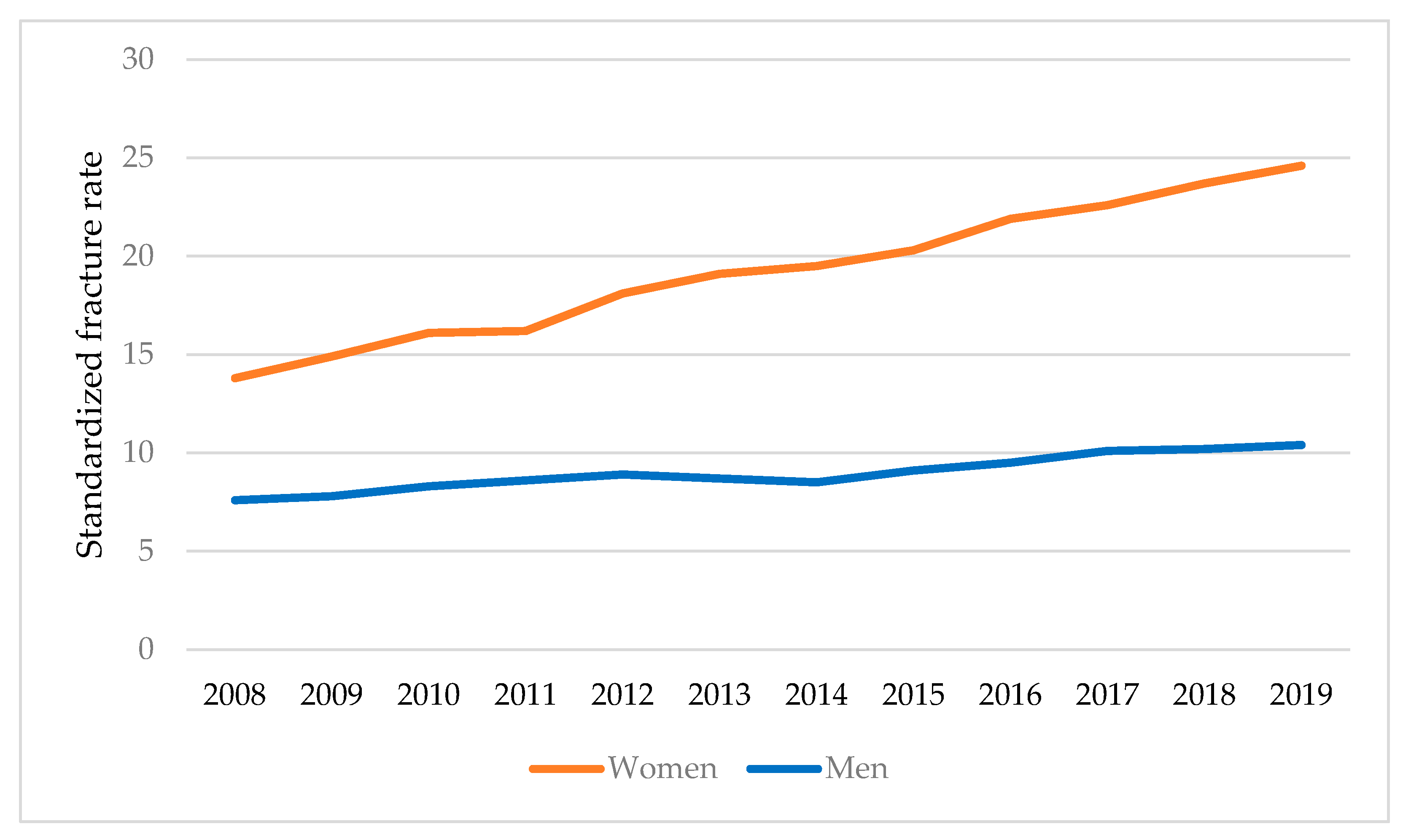
| 2008 | 7513 | 5,879,757 | 12.7 | 13.8 | 13.4–14.1 | 4266 | 5,537,747 | 7.7 | 7.6 | 7.3–7.7 |
| 2009 | 8138 | 5,830,977 | 13.9 | 14.9 | 14.4–15.2 | 4341 | 5,491,308 | 7.9 | 7.8 | 7.6–8.0 |
| 2010 | 8638 | 5,796,446 | 14.9 | 16.1 | 15.5–16.4 | 4635 | 5,548,789 | 8.3 | 8.3 | 8.1–8.5 |
| 2011 | 8653 | 5,768,005 | 15.0 | 16.2 | 15.7–16.5 | 4661 | 5,432,005 | 8.5 | 8.6 | 8.3–8.8 |
| 2012 | 9342 | 5,742,384 | 16.2 | 18.1 | 17.5–18.5 | 4781 | 5,407,876 | 8.8 | 8.9 | 8.6–9.1 |
| 2013 | 9797 | 5,721,101 | 17.1 | 19.1 | 18.5–19.5 | 4646 | 5,387,833 | 8.6 | 8.7 | 8.4–8.9 |
| 2014 | 10,004 | 5,699,711 | 17.5 | 19.5 | 18.9–19.9 | 4545 | 5,367,689 | 8.4 | 8.5 | 8.2–8.7 |
| 2015 | 10,362 | 5,672,982 | 18.2 | 20.3 | 19.6–20.7 | 4798 | 5,342,517 | 8.9 | 9.1 | 8.8–9.3 |
| 2016 | 10,784 | 5,640,532 | 19.1 | 21.9 | 21.2–22.4 | 4990 | 5,311,957 | 9.3 | 9.5 | 9.2–9.8 |
| 2017 | 11,076 | 5,608,023 | 19.7 | 22.6 | 21.8–23.1 | 5204 | 5,281,342 | 9.8 | 10.1 | 9.7–10.3 |
| 2018 | 11,512 | 5,575,173 | 20.6 | 23.7 | 22.9–24.2 | 5220 | 5,250,406 | 9.9 | 10.2 | 9.8–10.4 |
| 2019 | 11,948 | 5,544,784 | 21.5 | 24.6 | 23.8–25.2 | 5314 | 5,221,787 | 10.1 | 10.4 | 10.1–10.6 |
| 2008–2011 | 2012–2015 | 2016–2019 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Number of Hip Fractures (NO) | Population (PO) | Fracture Rate per 10,000 Inhabitants (r) | Number of Hip Fractures (NO) | Population (PO) | Fracture Rate per 10,000 Inhabitants (r) | Number of Hip Fractures (NO) | Population (PO) | Fracture Rate per 10,000 Inhabitants (r) |
| Women | |||||||||
| 40–44 years | 157 | 1,852,704 | 0.84 | 121 | 1,817,759 | 0.66 | 107 | 1,780,533 | 0.60 |
| 45–49 years | 266 | 1,713,053 | 1.55 | 273 | 1,680,742 | 1.62 | 258 | 1,646,322 | 1.56 |
| 50–54 years | 643 | 1,680,468 | 3.82 | 609 | 1,648,772 | 3.69 | 735 | 1,615,006 | 4.55 |
| 55–59 years | 1321 | 1,587,367 | 8.32 | 1293 | 1,557,427 | 8.30 | 1202 | 1,525,532 | 7.87 |
| 60–64 years | 2599 | 1,510,074 | 17.21 | 2481 | 1,541,442 | 16.09 | 2464 | 1,509,874 | 16.32 |
| 65–69 years | 4824 | 1,524,524 | 31.64 | 5062 | 1,484,351 | 34.10 | 4972 | 1,465,137 | 33.93 |
| 70–74 years | 9388 | 1,047,383 | 89.63 | 9627 | 1,027,628 | 93.68 | 10,465 | 1,006,583 | 103.96 |
| 75–79 years | 17,457 | 907,732 | 192.31 | 19,072 | 890,610 | 214.14 | 19,896 | 872,371 | 228.07 |
| 80–84 years | 28,203 | 698,255 | 403.90 | 32,600 | 685,085 | 475.91 | 35,132 | 671,055 | 523.57 |
| 84+ years | 40,215 | 349,127 | 1151.87 | 47,771 | 342,542 | 1394.60 | 54,006 | 335,527 | 1609.58 |
| Men | |||||||||
| 40–44 years | 539 | 1,751,983 | 3.07 | 371 | 1,711,870 | 2.16 | 352 | 1,676,813 | 2.10 |
| 45–49 years | 1055 | 1,619,924 | 6.51 | 921 | 1,582,835 | 5.81 | 839 | 1,550,420 | 5.41 |
| 50–54 years | 1568 | 1,589,111 | 9.86 | 1232 | 1,552,727 | 7.93 | 1440 | 1,520,928 | 9.46 |
| 55–59 years | 2268 | 1,501,071 | 15.11 | 2045 | 1,466,703 | 13.94 | 2048 | 1,436,666 | 14.35 |
| 60–64 years | 3418 | 1,485,664 | 23.01 | 3132 | 1,451,649 | 21.57 | 3200 | 1,421,920 | 22.50 |
| 65–69 years | 4759 | 1,441,645 | 33.01 | 4748 | 1,408,637 | 33.70 | 5209 | 1,379,783 | 37.75 |
| 70–74 years | 7032 | 990,443 | 70.99 | 6868 | 967,766 | 70.96 | 12,808 | 947,947 | 135.11 |
| 75–79 years | 10,549 | 858,384 | 122.89 | 10,914 | 838,730 | 130.12 | 11,234 | 821,554 | 136.74 |
| 80–84 years | 15,959 | 660,029 | 241.79 | 17,373 | 645,177 | 269.27 | 17,999 | 631,964 | 284.81 |
| 84+ years | 24,167 | 336,147 | 718.94 | 26,968 | 322,588 | 835.98 | 28,991 | 315,982 | 917.48 |
| Age | Number of Hip Fractures a (NO) | Number of Hip Prostheses b (NHP) | Population (PO) | Observed Fracture Rate per 10,000 Thousand Inhabitants (r) | Calculated Fracture Rate in Scenario per 10,000 Thousand Inhabitants c (rs) |
|---|---|---|---|---|---|
| Women 2008 | |||||
| 40–59 years | 495 | 11,735 | 1,726,296 | 2.86 | 2.87 |
| 60–79 years | 3952 | 27,825 | 1,277,671 | 30.93 | 31.27 |
| 80+ years | 3066 | 1645 | 264,589 | 115.87 | 136.43 |
| Women 2019 | |||||
| 40–59 years | 417 | 26,173 | 1,627,948 | 2.56 | 2.58 |
| 60–79 years | 4940 | 62,056 | 1,204,881 | 40.99 | 42.08 |
| 80+ years | 6357 | 3669 | 225,553 | 254.77 | 256.66 |
| Men 2008 | |||||
| 40–59 years | 1004 | 10,415 | 1,625,882 | 6.17 | 6.18 |
| 60–79 years | 2286 | 14,722 | 1,203,352 | 18.99 | 19.11 |
| 80+ years | 976 | 637 | 249,198 | 39.16 | 39.21 |
| Men 2019 | |||||
| 40–59 years | 853 | 25,199 | 1,533,116 | 5.56 | 5.6 |
| 60–79 years | 2607 | 35,621 | 1,134,694 | 22.97 | 23.00 |
| 80+ years | 1758 | 1541 | 234,980 | 74.81 | 75.06 |
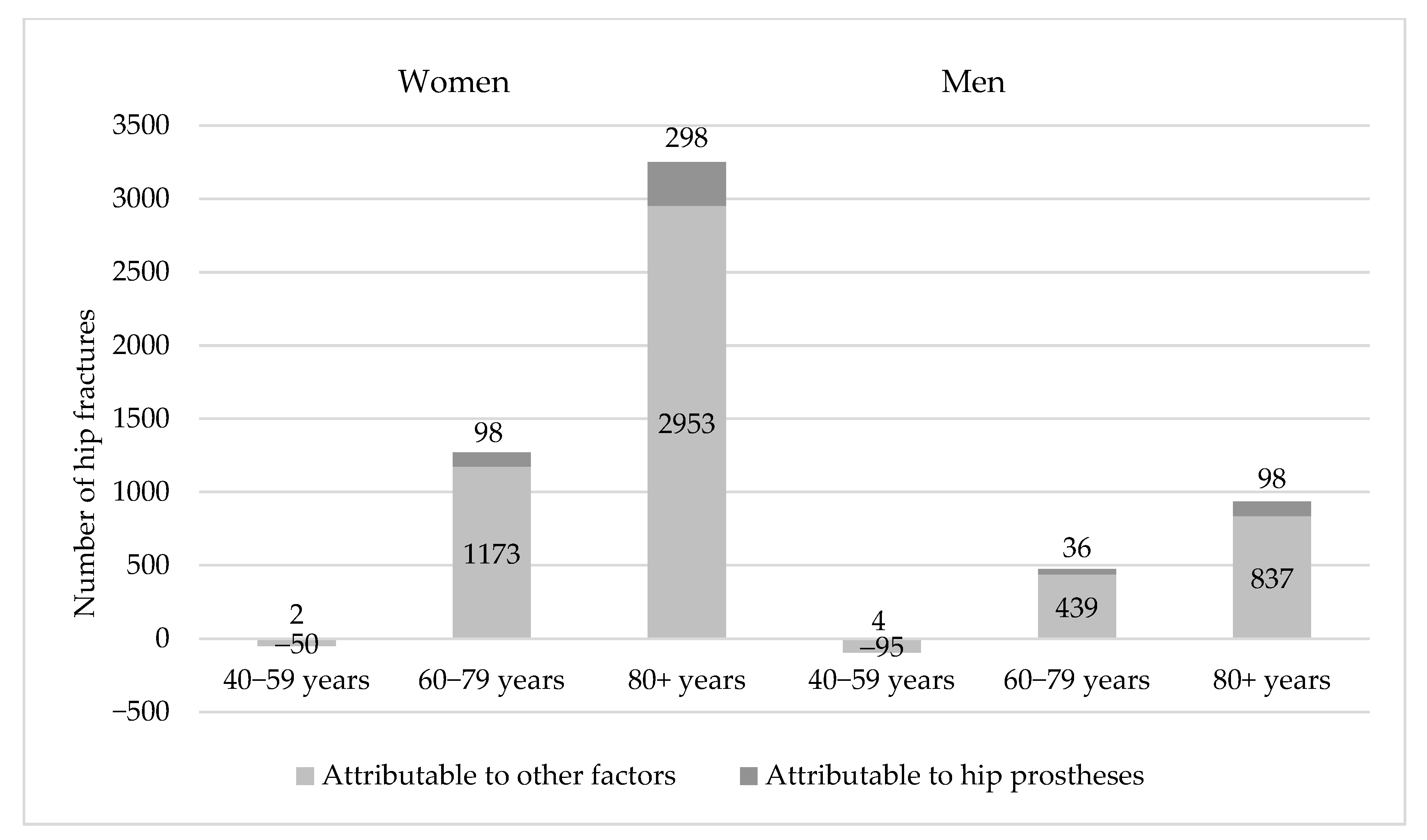
| Gender | Age | Population in 2019 (PO) | Observed Number of Hip Fractures in 2019 (NO) | Fracture Incidence in Scenario 2008 (rs) | Expected Number of Hip Fractures in 2019 (NX) | Difference Between Observed and Expected Fractures in 2019 (NO)-(NX) | Number of Fractures Attributable to the Hip Protheses (NXexplained HP) |
|---|---|---|---|---|---|---|---|
| Women | 40–59 | 1,627,948 | 417 | 2.87 | 467 | −50 | 2 |
| 60–79 | 1,204,881 | 4940 | 31.27 | 3767 | 1173 | 98 | |
| 80+ | 225,553 | 6357 | 136.43 | 3404 | 2953 | 298 | |
| Men | 40–59 | 1,533,116 | 853 | 6.18 | 948 | −95 | 4 |
| 60–79 | 1,134,694 | 2607 | 19.11 | 2168 | 439 | 36 | |
| 80+ | 234,980 | 1758 | 39.21 | 921 | 837 | 98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, F.; Moldovan, L. The Impact of Total Hip Arthroplasty on the Incidence of Hip Fractures in Romania. J. Clin. Med. 2025, 14, 4636. https://doi.org/10.3390/jcm14134636
Moldovan F, Moldovan L. The Impact of Total Hip Arthroplasty on the Incidence of Hip Fractures in Romania. Journal of Clinical Medicine. 2025; 14(13):4636. https://doi.org/10.3390/jcm14134636
Chicago/Turabian StyleMoldovan, Flaviu, and Liviu Moldovan. 2025. "The Impact of Total Hip Arthroplasty on the Incidence of Hip Fractures in Romania" Journal of Clinical Medicine 14, no. 13: 4636. https://doi.org/10.3390/jcm14134636
APA StyleMoldovan, F., & Moldovan, L. (2025). The Impact of Total Hip Arthroplasty on the Incidence of Hip Fractures in Romania. Journal of Clinical Medicine, 14(13), 4636. https://doi.org/10.3390/jcm14134636







