Intermediate-Term Clinical Outcomes After the Shortening Arthrodesis for Ankle Arthropathy with Severe Bone Defect
Abstract
1. Introduction
2. Materials and Methods
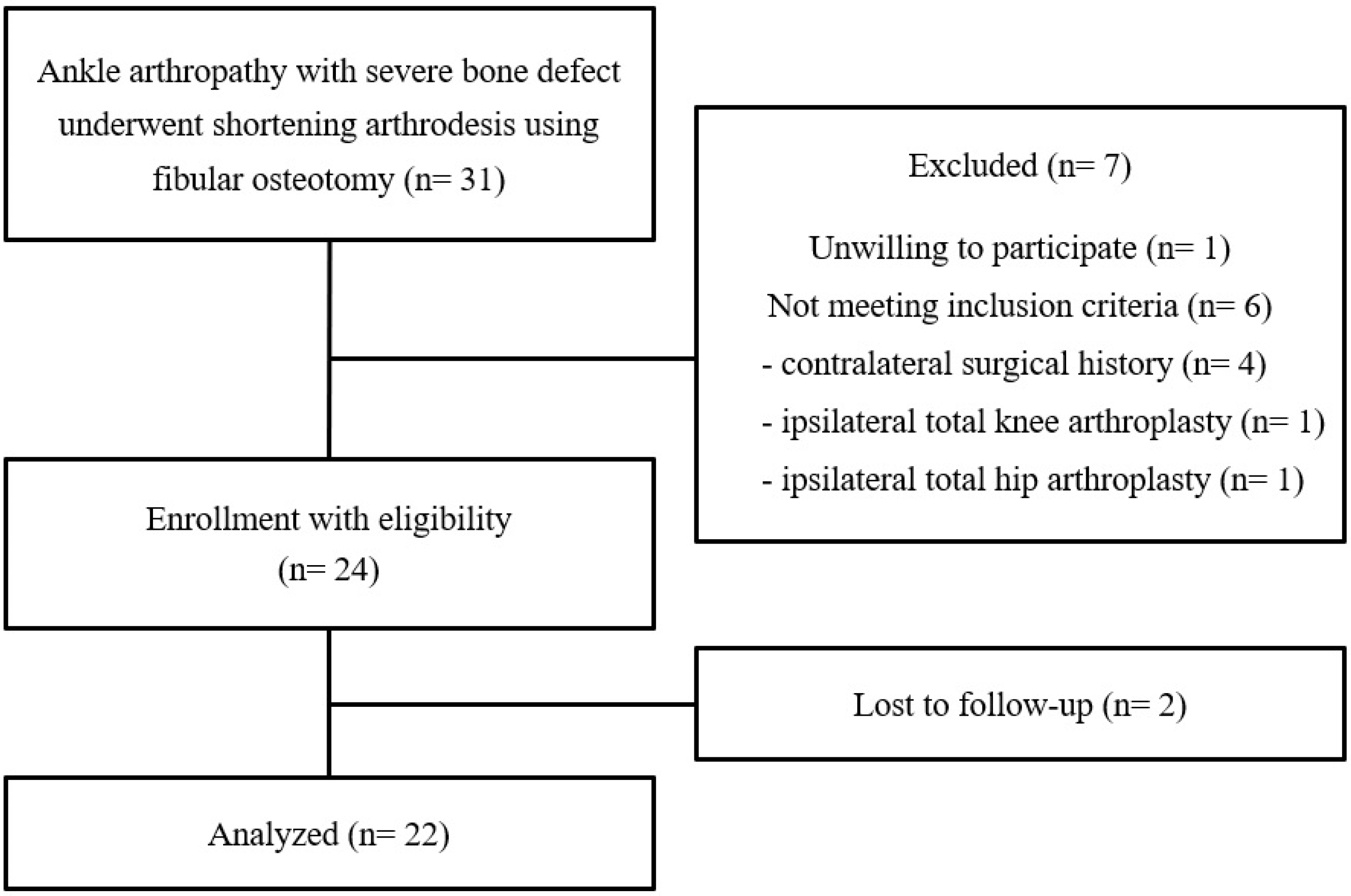
2.1. Study Subjects
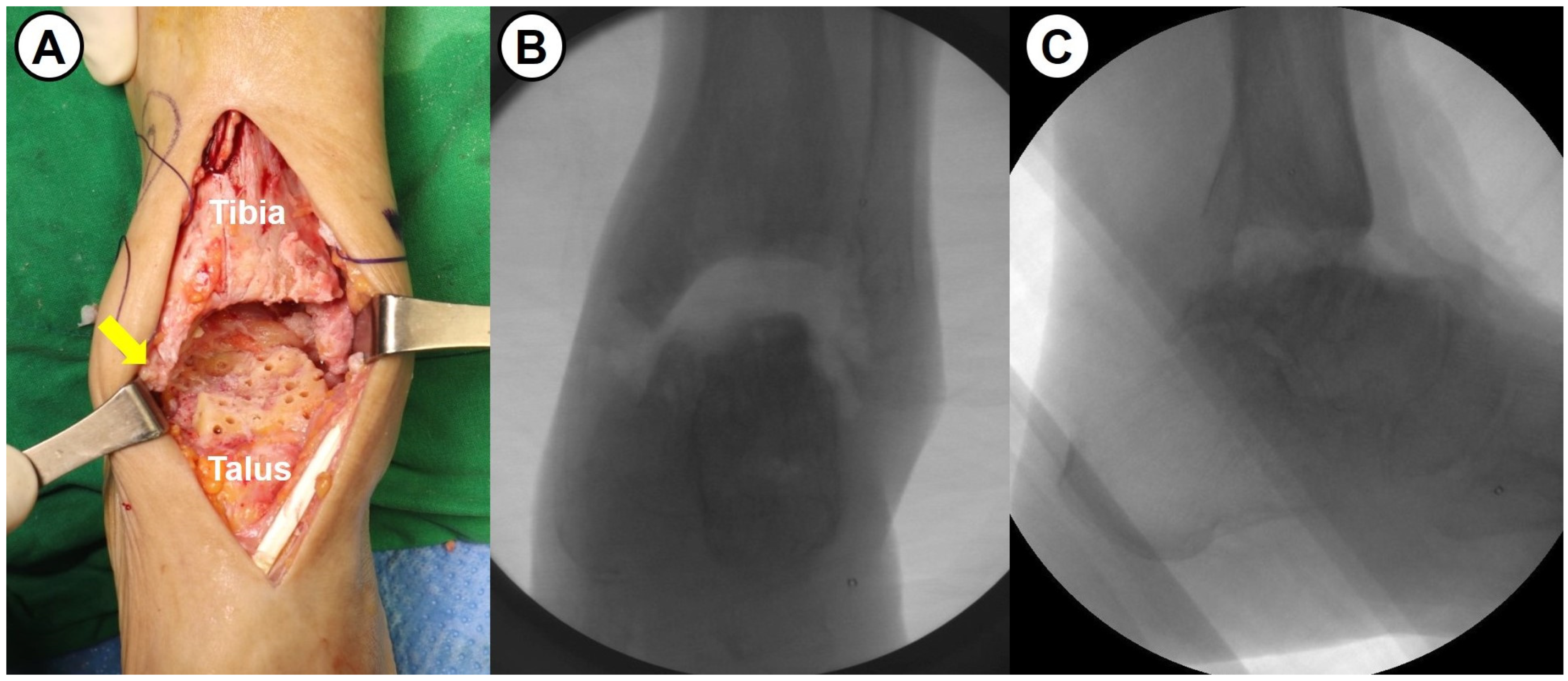
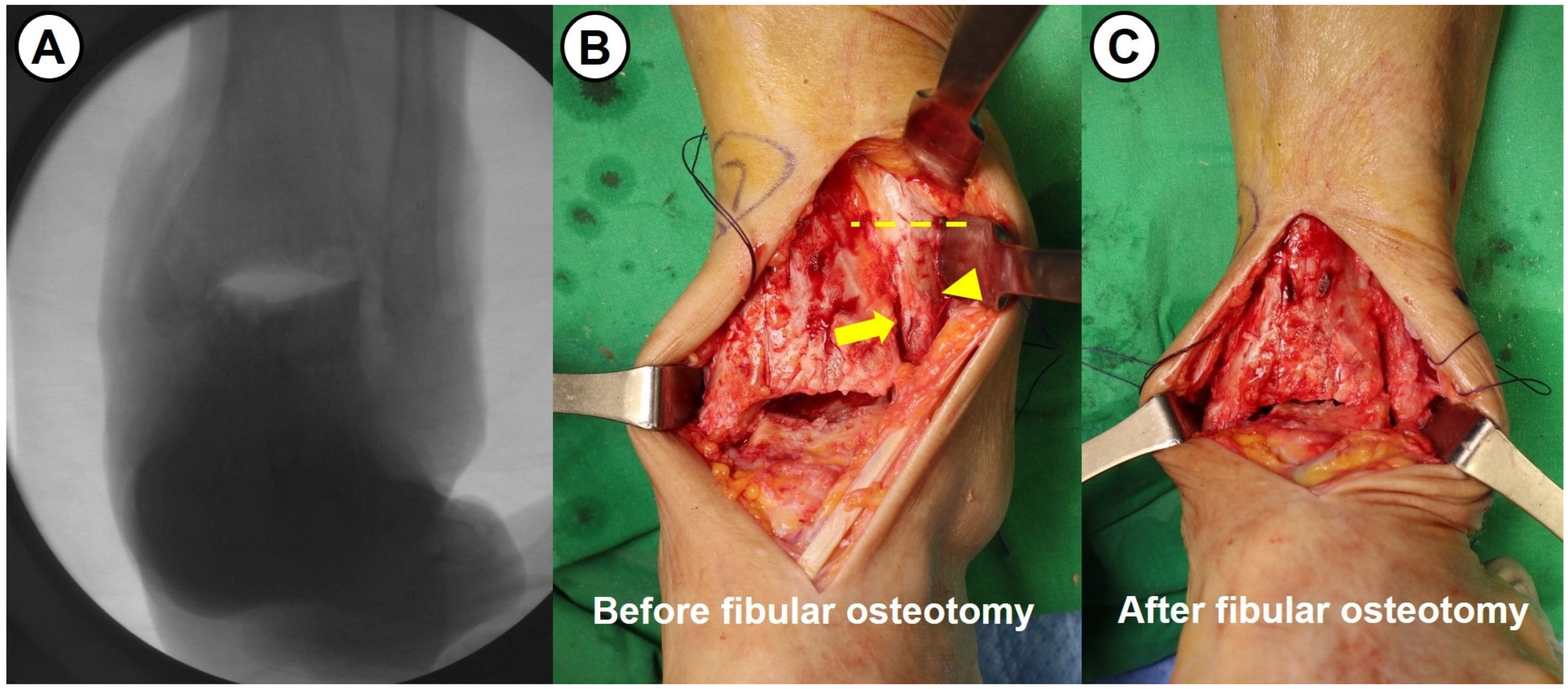
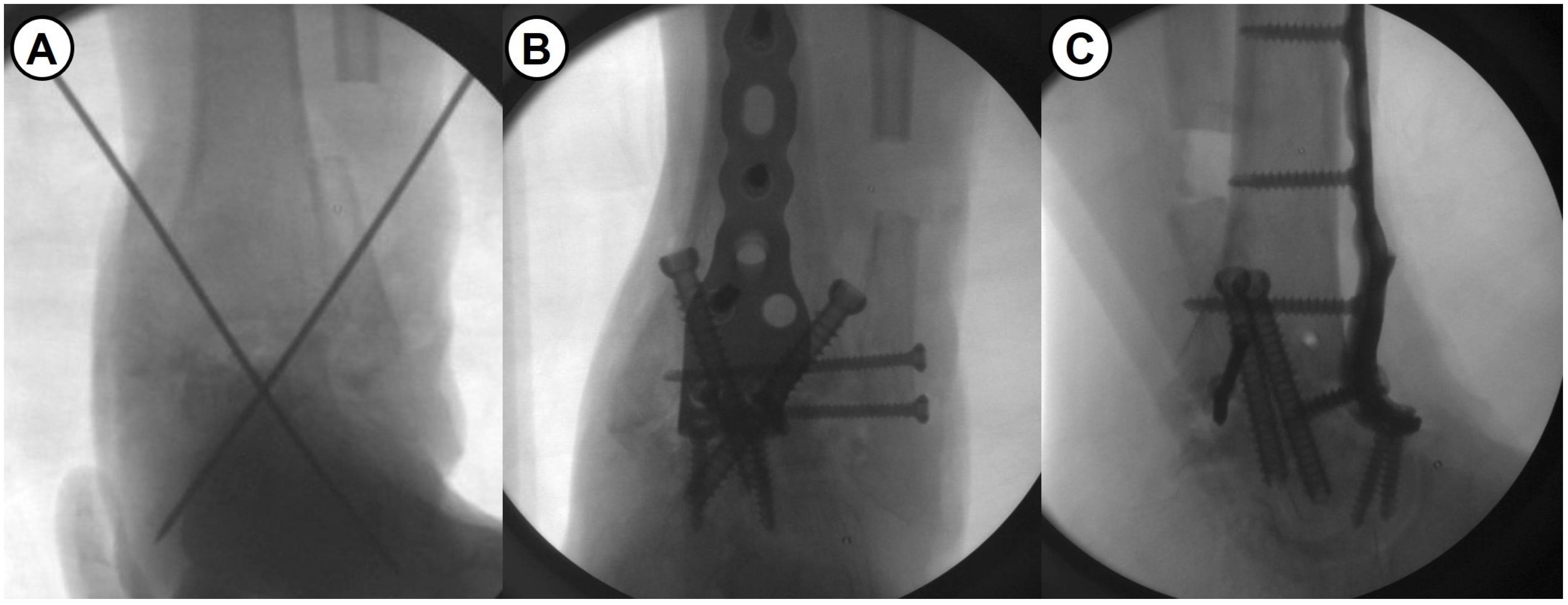
2.2. Surgical Procedure and Rehabilitation
2.3. Evaluation of the Patient-Reported Clinical Outcomes
2.4. Evaluation of Radiological Outcomes
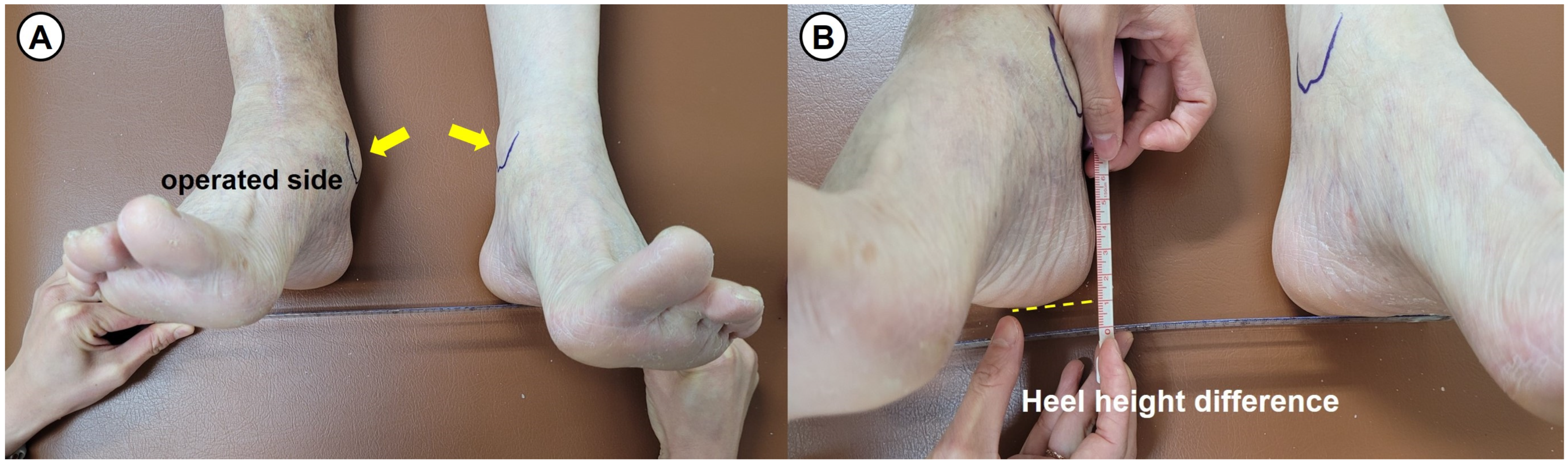
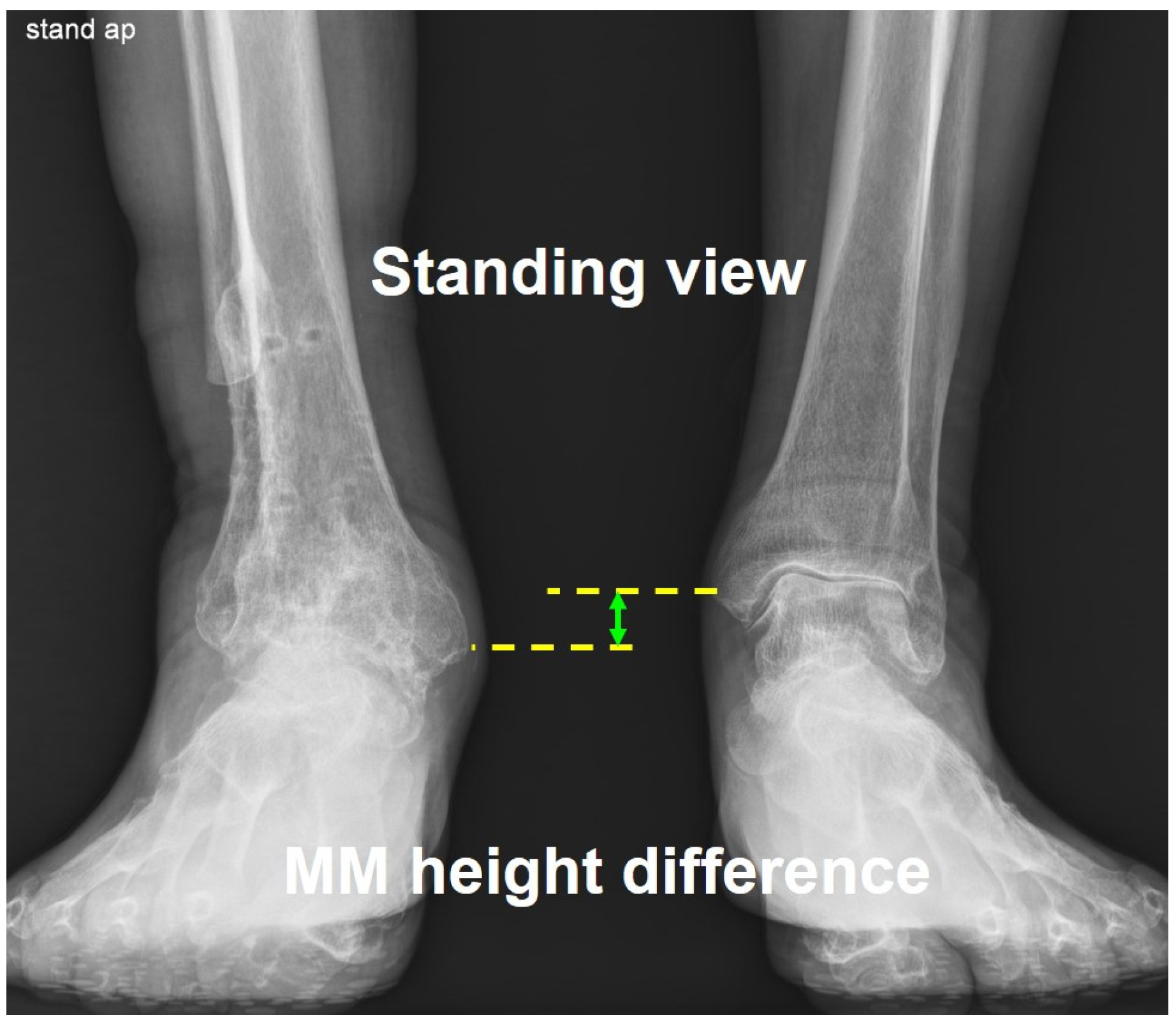
2.5. Evaluation of Leg Length Discrepancy
2.6. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Patient-Reported Clinical Outcomes
3.3. Postoperative Complications
3.4. Radiological Outcomes
3.5. The Leg Length Discrepancy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LLD | Leg length discrepancy |
| FAOS | Foot and Ankle Outcome Score |
| FAAM | Foot and Ankle Ability Measure |
| VAS | Visual analogue scale |
| TAA | Total ankle arthroplasty |
References
- Uluöz, M.; Gökmen, M.Y.; Varmiş, H.O. Arthrodesis in the treatment of ankle osteoarthritis due to neglected malleolar fractures in the elderly. Medicine 2024, 103, e40861. [Google Scholar] [CrossRef]
- Puri, A. Current concepts in ankle arthrodesis. J. Clin. Orthop. Trauma 2024, 56, 102537. [Google Scholar] [CrossRef] [PubMed]
- Ruland, J.R.; Sumpter, A.; McVey, E.; Novicoff, W.; Pierce, J.; Cooper, M.T.; Perumal, V.; Park, J.S. Clinical and radiographicoutcomes after hindfoot and ankle arthrodesis using cellular bone allograft augmentation: A short report. Foot Ankle Orthop. 2024, 9, 24730114241281325. [Google Scholar] [CrossRef] [PubMed]
- Roos, E.M.; Brandsson, S.; Karlsson, J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. FootAnkle Int. 2001, 22, 788–794. [Google Scholar] [CrossRef]
- Martin, R.L.; Irrgang, J.J.; Burdett, R.G.; Conti, S.F.; Van Swearingen, J.M. Evidence of validity for the foot and ankle ability measure (FAAM). Foot Ankle Int. 2005, 26, 968–983. [Google Scholar] [CrossRef] [PubMed]
- Chalayon, O.; Wang, B.; Blankenhorn, B.; Jackson, J.B., III.; Beals, T.; Nickisch, F.; Saltzman, C.L. Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int. 2015, 36, 1170–1179. [Google Scholar] [CrossRef]
- SooHoo, N.F.; Zingmond, D.S.; Ko, C.Y. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J. Bone Joint Surg. Am. 2007, 89, 2143–2149. [Google Scholar] [CrossRef]
- Mahamid, A.; Maman, D.; Sofer, S.; Pavlenko, M.; Mansour, A.; Hodruj, M.; Berkovich, Y.; Behrbalk, E. Ankle arthrodesis: Epidemiology, etiology, and complications in diabetic vs. nondiabetic patients using US nationwide inpatient sample data. Foot Ankle Orthop. 2025, 10, 24730114251315122. [Google Scholar] [CrossRef]
- Gökmen, M.Y.; Uluöz, M.; Dülgeroğlu, T.C. Anterior plate-supported cannulated screw surgery for ankle arthrodesis: Clinicaland radiologic results in patients with trauma-related end-stage ankle osteoarthritis. Med. Sci. Monit. 2024, 30, e944452. [Google Scholar] [CrossRef]
- Hanada, M.; Hotta, K.; Matsuyama, Y. Difficulty in bone union after arthrodesis to treat Charcot arthropathy of the foot andankle. J. Orthop. 2024, 62, 13–16. [Google Scholar] [CrossRef]
- Steginsky, B.D.; Suhling, M.L.; Vora, A.M. Ankle arthrodesis with anterior plate fixation in patients at high risk for nonunion. Foot Ankle Spec. 2020, 13, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Collman, D.R.; Kaas, M.H.; Schuberth, J.M. Arthroscopic ankle arthrodesis: Factors influencing union in 39 consecutive patients. Foot Ankle Int. 2006, 27, 1079–1085. [Google Scholar] [CrossRef] [PubMed]
- Perlman, M.H.; Thordarson, D.B. Ankle fusion in a high risk population: An assessment of nonunion risk factors. Foot AnkleInt. 1999, 20, 491–496. [Google Scholar] [CrossRef]
- Thevendran, G.; Wang, C.; Pinney, S.J.; Penner, M.J.; Wing, K.J.; Younger, A.S. Nonunion risk assessment in foot and anklesurgery: Proposing a predictive risk assessment model. Foot Ankle Int. 2015, 36, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Baker, L.; Vulcano, J.P.E.; Kaplan, J.; Aiyer, A. Risk factors for Nonunion following ankle arthrodesis: A systematicreview and meta-analysis. Foot Ankle Spec. 2023, 16, 60–77. [Google Scholar] [CrossRef]
- Greene, H.; Dodd, A.; Le, I.; LaMothe, J. Nonunion in foot and ankle arthrodesis surgery: Review of risk factors, identificationof high-risk patients, and a guide to perioperative testing and optimization. J. Am. Acad. Orthop. Surg. 2024. online ahead of print. [Google Scholar] [CrossRef]
- Al-Naseem, A.O.; Hayat, J.; Addar, A.; Marwan, Y. External versus internal fixation techniques for ankle arthrodesis: A systematic review and meta-analysis. J. Foot Ankle Surg. 2024, 63, 769–775. [Google Scholar] [CrossRef]
- Flint, W.W.; Hirose, C.B.; Coughlin, M.J. Ankle arthrodesis using an anterior titanium dual locked plating construct. J. Foot Ankle Surg. 2017, 56, 304–308. [Google Scholar] [CrossRef]
- Guo, C.; Yan, Z.; Barfield, W.R.; Hartsock, L.A. Ankle arthrodesis using anatomically contoured anterior plate. Foot Ankle Int. 2010, 31, 492–498. [Google Scholar] [CrossRef]
- Kusnezov, N.; Dunn, J.C.; Koehler, L.R.; Orr, J.D. Anatomically contoured anterior plating for isolated tibiotalar arthrodesis: Asystematic review. Foot Ankle Spec. 2017, 10, 352–358. [Google Scholar] [CrossRef]
- Lindsey, B.B.; Hundal, R.; Bakshi, N.K.; Holmes, J.R.; Talusan, P.G.; Walton, D.M. Ankle arthrodesis through an anterior approach. J. Orthop. Trauma 2020, 34, S42–S43. [Google Scholar] [CrossRef]
- Mitchell, P.M.; Douleh, D.G.; Thomson, A.B. Comparison of ankle fusion rates with and without anterior plate augmentation. Foot Ankle Int. 2017, 38, 419–423. [Google Scholar] [CrossRef]
- Schoenhaus, H.D.; Lam, S.; Treaster, A.; Troiano, M. Use of a small bilateral external fixator for ankle fusion. J. Foot Ankle Surg. 2009, 48, 89–92. [Google Scholar] [CrossRef]
- Zwipp, H.; Rammelt, S.; Endres, T.; Heineck, J. High union rates and function scores at midterm follow-up with ankle arthrodesis using a four screw technique. Clin. Orthop. Relat. Res. 2010, 468, 958–968. [Google Scholar] [CrossRef]
- Betz, M.M.; Benninger, E.E.; Favre, P.P.; Wieser, K.K.; Vich, M.M.; Espinosa, N. Primary stability and stiffness in ankle arthrodes-crossed screws versus anterior plating. Foot Ankle Surg. 2013, 19, 168–172. [Google Scholar] [CrossRef]
- Clifford, C.; Berg, S.; McCann, K.; Hutchinson, B. A biomechanical comparison of internal fixation techniques for ankle arthrodesis. J. Foot Ankle Surg. 2015, 54, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Kestner, C.J.; Glisson, R.R.; DeOrio, J.K.; Nunley, J.A., II. A biomechanical analysis of two anterior ankle arthrodesis systems. Foot Ankle Int. 2013, 34, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Tarkin, I.S.; Mormino, M.A.; Clare, M.P.; Haider, H.; Walling, A.K.; Sanders, R.W. Anterior plate supplementation increasesankle arthrodesis construct rigidity. Foot Ankle Int. 2007, 28, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Choi, S.M.; Kim, M.B.; Cho, B.K. The effects of tibialis anterior tenotomy on wound complications and functionaloutcomes after anterior fusion plating for severe ankle arthritis. J. Foot Ankle Surg. 2023, 62, 237–243. [Google Scholar] [CrossRef]
- Cifaldi, A.; Thompson, M.; Abicht, B. Tibiotalocalcaneal arthrodesis with structural allograft for management of large osseousdefects of the hindfoot and ankle: A systematic review and meta-analysis. J. Foot Ankle Surg. 2022, 61, 900–906. [Google Scholar] [CrossRef]
- Escudero, M.I.; Poggio, D.; Alvarez, F.; Barahona, M.; Vivar, D.; Fernandez, A. Tibiotalocalcaneal arthrodesis with distal tibialallograft for massive bone deficits in the ankle. Foot Ankle Surg. 2019, 25, 390–397. [Google Scholar] [CrossRef]
- Miller, C.P.; Chiodo, C.P. Autologous bone graft in foot and ankle surgery. Foot Ankle Clin. 2016, 21, 825–837. [Google Scholar] [CrossRef] [PubMed]
- Clough, T.; Jamjoom, B.; Jagani, N.; Quarcoopome, J.; Kakwani, R.; Townshend, D.; Cullen, N.; Patel, S.; Malhotra, K.; Welck, M. Morselized femoral head impaction bone grafting of large defects in ankle and hindfoot fusions. Foot Ankle Int. 2025, 46, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Jeng, C.L.; Campbell, J.T.; Tang, E.Y.; Cerrato, R.A.; Myerson, M.S. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int. 2013, 34, 1256–1266. [Google Scholar] [CrossRef]
- Kakarala, G.; Rajan, D.T. Comparative study of ankle arthrodesis using cross screw fixation versus anterior contoured plate plus cross screw fixation. Acta. Orthop. Belg. 2006, 72, 716–721. [Google Scholar] [PubMed]
- Tenenbaum, S.; Coleman, S.C.; Brodsky, J.W. Improvement in gait following combined ankle and subtalar arthrodesis. J. Bone Joint Surg. Am. 2014, 96, 1863–1869. [Google Scholar] [CrossRef]
- Brodsky, J.W.; Kane, J.M.; Coleman, S.; Bariteau, J.; Tenenbaum, S. Abnormalities of gait caused by ankle arthritis are improved by ankle arthrodesis. Bone Joint J. 2016, 98, 1369–1375. [Google Scholar] [CrossRef]
- Ciobanu, I.; Stanculescu, D.I.; Iliescu, A.; Popescu, A.M.; Seiciu, P.L.; Mikolajczyk, T.; Moldovan, F.; Berteanu, M. The usability pilot study of a mechatronic system for gait rehabilitation. Procedia Manuf. 2018, 22, 864–871. [Google Scholar] [CrossRef]

| Variables | Intraclass Correlation Coefficient (95% CI *) | |
|---|---|---|
| Heel Height Difference | Medial Malleolar Height Difference | |
| Intraobserver reproducibility | ||
| Researcher 1 | 0.91 | 0.95 |
| Researcher 2 | 0.82 | 0.92 |
| Researcher 3 | 0.85 | 0.9 |
| Interobserver agreement | ||
| Researcher 1–2 | 0.85 | 0.88 |
| Researcher 2–3 | 0.89 | 0.91 |
| Researcher 3–1 | 0.79 | 0.82 |
| Scheme 6 | Preoperative | PO 6 Months | PO 1 Year | Final F/U | p-Value † |
|---|---|---|---|---|---|
| FAOS * | |||||
| Pain | 14.3 ± 8.1 | 73.9 ± 18.6 | 83.1 ± 13.2 | 86.2 ± 11.4 | <0.001 |
| Symptoms | 31.9 ± 15.3 | 70.8 ± 17.5 | 79.5 ± 15.3 | 83.4 ± 14.2 | <0.001 |
| Activity of daily living | 30.2 ± 12.9 | 73.1 ± 15.9 | 84.2 ± 11.7 | 89.5 ± 9.6 | <0.001 |
| Sports | 11.8 ± 6.5 | 44.5 ± 16.7 | 62.4 ± 17.5 | 69.3 ± 16.1 | <0.001 |
| Quality of life | 20.8 ± 11.2 | 70.4 ± 16.8 | 80.2 ± 14.9 | 82.6 ± 15.2 | <0.001 |
| Total FAOS | 21.8 ± 9.8 | 66.5 ± 13.6 | 77.9 ± 11.4 | 82.2 ± 13.5 | <0.001 |
| FAAM * | |||||
| Daily activity | 34.5 ± 14.4 | 71.3 ± 15.4 | 83.8 ± 11.5 | 92.5 ± 7.4 | <0.001 |
| Sports activity | 12.6 ± 6.8 | 55.9 ± 17.1 | 68.5 ± 16.6 | 74.3 ± 15.8 | <0.001 |
| Total FAAM score | 23.5 ± 10.9 | 63.6 ± 16.9 | 76.2 ± 13.4 | 83.4 ± 12.7 | <0.001 |
| Number (%) | |
|---|---|
| Superficial wound infection | 2 (9.1%) |
| Delayed wound healing (≥3 weeks) | 3 (13.6%) |
| Superficial peroneal nerve injury | 2 (9.1%) |
| Metal irritation symptom | 2 (9.1%) |
| Implant removal | 6 (27.3%) |
| Delayed union (≥6 months) | 1 (4.5%) |
| Nonunion (failed fusion) | 0 |
| Progressive arthritis in the adjacent joints | 2 (9.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, J.-H.; Kim, S.-H.; Cho, B.-K. Intermediate-Term Clinical Outcomes After the Shortening Arthrodesis for Ankle Arthropathy with Severe Bone Defect. J. Clin. Med. 2025, 14, 4605. https://doi.org/10.3390/jcm14134605
Song J-H, Kim S-H, Cho B-K. Intermediate-Term Clinical Outcomes After the Shortening Arthrodesis for Ankle Arthropathy with Severe Bone Defect. Journal of Clinical Medicine. 2025; 14(13):4605. https://doi.org/10.3390/jcm14134605
Chicago/Turabian StyleSong, Jae-Hwang, Sung-Hoo Kim, and Byung-Ki Cho. 2025. "Intermediate-Term Clinical Outcomes After the Shortening Arthrodesis for Ankle Arthropathy with Severe Bone Defect" Journal of Clinical Medicine 14, no. 13: 4605. https://doi.org/10.3390/jcm14134605
APA StyleSong, J.-H., Kim, S.-H., & Cho, B.-K. (2025). Intermediate-Term Clinical Outcomes After the Shortening Arthrodesis for Ankle Arthropathy with Severe Bone Defect. Journal of Clinical Medicine, 14(13), 4605. https://doi.org/10.3390/jcm14134605






