Abstract
Background: Septoplasty is a widely performed surgical procedure to correct nasal septal deviations and improve respiratory function. One of its most significant complications is septal perforation, which can severely impact the patient’s quality of life. This study evaluates the use of bovine pericardium grafts to enhance mucosal healing, thereby reducing the risk of postoperative septal perforation in cases with intraoperative bilateral mucosal defects. Methods: A retrospective study was conducted on patients who underwent septoplasty between January 2018 and January 2025 in whom bovine pericardium grafts were interposed due to the presence of bilateral opposing mucosal defects. Epidemiological and surgical variables were recorded, and outcomes and complications were analyzed. Results: Out of the 4151 septoplasties performed, 30 cases (0.72%) required bovine pericardium interposition. The mean patient age was 42.87 years. Postoperative absence of septal perforation was confirmed in 90% of cases, with only three postoperative perforations, all asymptomatic and approximately 2 mm in size. Complications were recorded in three patients (10%), all of which were resolved with conservative treatment and without sequelae. Conclusions: For the first time in routine surgical practice, bovine pericardium emerges as a viable option for preventing postoperative septal perforation in cases with bilateral opposing mucosal defects. With a high closure rate and a low incidence of adverse events, this material represents a promising tool in septal surgery.
1. Introduction
Septoplasty is a widely performed surgical procedure to correct nasal septal deviations and improve nasal respiratory function. It can be performed as a standalone procedure or in combination with other nasal and sinus surgeries, such as septorhinoplasty, functional endoscopic sinus surgery (FESS), or anterior skull base surgery. However, it is not without complications, with septal perforation being one of the most significant. This complication disrupts normal airflow, generating turbulence that can lead to dryness, epistaxis, crusting, and, ultimately, a considerable reduction in quality of life [1].
The incidence of septal perforation following septoplasty ranges between 1% and 6.7% [2,3,4], typically resulting from bilateral mucosal tears during surgery. Additionally, factors such as cocaine or other nasal irritant use and a history of previous septal surgery, infections, or trauma can increase the risk of this complication. Prevention relies on meticulous surgical technique, with careful elevation of the mucoperichondrial and mucoperiosteal flaps, avoiding unnecessary tears, and minimizing the resection of cartilaginous or bony tissue [5].
Once a septal perforation has developed, treatment can be either symptomatic or surgical. The choice of treatment depends primarily on the patient’s symptoms, regardless of perforation size. Asymptomatic perforations are typically managed conservatively with nasal moisturizers, whereas symptomatic perforations often require surgical correction. Various techniques have been used for repair, including sliding flaps and the interposition of fascia and cartilage [6]. More recently, there has been significant progress with endonasal flap techniques [7], particularly mucosal flaps based on the ethmoidal artery [8], the greater palatine artery [9], or combined approaches [10].
The presence of bilateral opposing mucosal dehiscence carries a high risk of postoperative septal perforation, which can increase stress and negatively impact the surgeon’s confidence, potentially worsening surgical outcomes. Therefore, it is essential to have intraoperative tools that can minimize the risk of definitive postoperative perforation. Recent research has explored the use of biomaterials such as bovine pericardium, which has shown promising results in both experimental and clinical studies [11]. Its ability to serve as a scaffold for cellular migration and promote healing suggests that it could be a viable alternative for closing mucosal flap tears, reducing the risk of reperforation and improving surgical outcomes.
Bovine pericardium has previously been used for defect closure in the head and neck [12,13], including anterior skull base surgery, and it has shown positive experimental results in septal applications [11]. Building upon these findings, our study is the first to evaluate the clinical efficacy of bovine pericardium in preventing postoperative septal perforation in patients with intraoperatively identified bilateral opposing mucosal disruptions.
2. Materials and Methods
A retrospective analysis was conducted on septal surgeries performed between January 2018 and January 2025 at the Hospital Universitario Fundación Jiménez Díaz and Hospital Universitario General de Villalba. Specifically, data were collected from cases in which the interposition of a heterologous graft between both mucoperichondrial flaps was deemed necessary at the surgeon’s discretion. Inclusion criteria included patients over 18 years of age who underwent septoplasty, either as a standalone procedure or in combination with turbinate and/or sinus surgeries, with a minimum follow-up period of 3 months.
Data potentially influencing surgical outcomes were collected, including epidemiological variables (sex and age) and surgical parameters (type of procedure performed, antibiotic prophylaxis, postoperative antibiotic treatment, complications, and outcome).
Septoplasties were performed using a modified Cottle technique, involving a conservative resection of deviated cartilage and bone, as required. Procedures were carried out under direct visualization with a surgical headlight or microscopic assistance.
If bilateral opposing mucosal defects were observed intraoperatively, a graft was interposed. Bilateral opposing mucosal defects measuring at least 5 mm were considered eligible for graft placement due to their higher likelihood of evolving into septal perforation. The graft was placed between both flaps, completely covering the dehiscence. When possible, the mucosal defect was sutured unilaterally or bilaterally with Polysorb® (Roquette Frères, Lestrem, France) 4-0 to reduce its size (Figure 1a). In all cases, a transfixion suture with Polysorb® 4-0 was performed throughout the nasal septum, including the heterologous graft interposed between the mucosal flaps (Figure 1b). The heterologous graft used in all cases was Tutopatch® (Tutogen Medical GmbH, Neunkirchen, Germany), a biological membrane derived from bovine pericardium, which requires no prior preparation before placement. The complete procedure video can be observed in the Supplementary Materials.
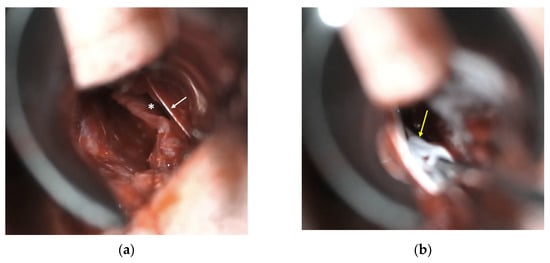
Figure 1.
Microscopic intraoperative view: (a) left nasal mucosal flap dehiscence (*) and suture of mucosal flap (arrow); (b) placement of bovine pericardium graft (arrow) between both nasal mucosal flaps.
In all cases, paraseptal silicone splints were placed and secured to the nasal septum. Each patient underwent detailed follow-up for at least 3 months, assessed via anterior rhinoscopy and nasofibroscopy.
In some cases, nasal packing was performed using an expandable sponge tampon, which was removed within 24–48 h. In other cases, no nasal packing was performed; instead, cotton pledges soaked in 2% lidocaine with epinephrine were placed and removed 30 min postoperatively. The decision to use nasal packing evolved over time based on the emerging literature discouraging its routine use in septal surgery given its lack of proven benefits in preventing bleeding, hematomas, or residual septal deviation compared to alternative techniques [14].
Statistical analysis was conducted using RStudio (version 4.0.3). Both continuous and categorical variables were analyzed considering data distributions and the nature of the variables involved. A descriptive analysis was performed on the quantitative and categorical variables in the dataset. For categorical variables—such as sex, type of intervention, use of splints, use of nasal packing, prophylactic or postoperative antibiotic use, recorded complications, and outcome—absolute frequencies and relative percentages were calculated.
To analyze the relationship between age (continuous variable) and surgical outcome (categorical variable), the Mann–Whitney U test was applied, as normality assumptions were not met. Fisher’s exact test was applied to assess the relationship between categorical variables, considering the small sample size and low frequencies in certain categories. Additionally, 95% confidence intervals were calculated for each analysis to estimate the strength of associations between categorical variables. A p-value < 0.05 was considered statistically significant for all tests.
3. Results
During the study period, a total of 4151 septal surgeries were performed at the participating hospitals, excluding cases involving septal perforation repair. These procedures included primary and revision septoplasties and primary and revision septorhinoplasties, with or without unilateral or bilateral synchronous endoscopic nasal and sinus surgery (FESS). Among these, bovine pericardium graft interposition was performed in 30 patients [0.72%]. The cohort consisted of 24 men and six women, with a mean age of 42.87 years (range: 21–68 years).
The most common indication for surgery was primary septal deviation or persistent nasal septal deviation. In total, 80% of cases (n = 24) underwent a primary septoplasty or septorhinoplasty, while the remaining 20% were revision cases.
In all patients, paraseptal silicone splints were sutured to the nasal septum using 3-0 silk sutures. Nasal packing with polyvinyl alcohol sponges was performed in 56.67% of cases (n = 17). Notably, nasal packing was omitted in later cases due to a postoperative protocol change implemented in March 2022 based on prior recommendations [15]. The only exception was cases involving FESS, where the trend towards reducing the use of nasal packing, like septoplasties, has been increasing. In all cases, paraseptal silicone splints were removed between 10 and 21 days postoperatively (median 15 days). The variability in the timing of splint removal is attributable to the retrospective design of the study. However, in the three cases of persistent septal perforation, splint removal occurred between 14 and 17 days postoperatively, similar to the cohort median, suggesting no clear association between splint duration and reperforation.
Prophylactic antibiotics were administered prior to surgery in 50% of cases (n = 15), and postoperative antibiotics were prescribed for 40% of patients (n = 12). Complications were observed in three cases (10%), including one case of fever and rhinorrhea and two cases of significant pain and septal edema. The first case was treated with oral antibiotics (amoxicillin–clavulanate 875/125 mg every 8 h for 7 days) along with oral corticosteroids (prednisone 60 mg every 24 h for 2 days, 20 mg every 24 h for 2 days, followed by 20 mg every 24 h for another 2 days). The remaining two cases had already received postoperative antibiotics and were additionally treated with the same oral corticosteroid regimen. None of these patients developed residual septal perforation.
Across the entire series, three patients (10%) developed a residual septal perforation, which in all cases measured <2 mm and was asymptomatic. The median follow-up duration was 9 months (range: 3–24 months).
None of the analyzed variables, including age (p = 0.8102), were significantly associated with postoperative outcomes. The complete dataset is summarized in Table 1.

Table 1.
Epidemiological data related to surgical outcomes. ATB (antibiotic).
4. Discussion
Septoplasty is a fundamental procedure for nasal surgeons, with septal perforation—alongside surgical site infection—recognized as a potential complication. Intraoperatively, the risk of postoperative perforation can often be anticipated due to difficult tissue dissection, the severity of septal deviation, or, in most cases, the condition of the mucoperichondrial or mucoperiosteal flaps. When bilateral opposing mucosal dehiscence occurs, there are limited options to prevent postoperative perforation beyond direct mucosal closure or an interposition of autologous cartilage. Thus, having a salvage material available for these cases can be highly beneficial.
Septal perforations can significantly impact quality of life [16], which is measurable [17] and can be improved through reconstructive techniques [1]. A perforation impairs nasal function by altering airflow dynamics and reducing the capacity for inspired air humidification [18]. This can lead to symptoms such as nasal dryness, crusting, recurrent epistaxis, and a sensation of obstruction, even in the absence of a true mechanical blockage. The location and size of the perforation play a crucial role, as they influence the magnitude of crossflow air turbulence, causing stress to the surrounding mucosa and exacerbating irritation and nasal discomfort [18].
The use of bovine pericardium in surgery is well-established, with strong clinical outcomes reported in various fields, including cardiac [19], vascular [20], urethral stricture [21], blepharophimosis [22], and cerebrospinal fluid fistula repair [23]. This extensive experience supports its biological plausibility as a graft material in different anatomical areas, including mucosal applications such as the nasal septum.
To date, bovine pericardium has only been used experimentally in the nasal septum, demonstrating stability, minimal antigenicity, and a high capacity for tissue integration without triggering a foreign body inflammatory response [11]. Therefore, our study is the first to evaluate the clinical use of bovine pericardium in preventing postoperative septal perforations in cases where there is an evident risk of residual perforation due to bilateral opposing mucosal dehiscence. With a 90% success rate in 30 cases, bovine pericardium has proven to be a valuable tool for preventing postoperative perforations using a straightforward surgical technique and with a 10% complication rate, none of which resulted in long-term sequelae.
Our study presents several limitations inherent to its design as a retrospective case series. The limited sample size restricts the generalizability of the findings and precludes drawing definitive conclusions. Moreover, the indication for graft placement was based on the surgeon’s intraoperative judgment, which introduces a potential selection bias and variability in case assessment. The absence of a control group without graft placement further limits the strength of the conclusions, although this was considered ethically inappropriate given the high risk of septal perforation in cases with bilateral mucosal defects.
Additionally, the study lacked long-term follow-up and did not include objective, validated patient-reported outcome measures, such as quality-of-life scales, which would have added valuable information regarding the functional impact of the intervention. The lack of comparative data from historical cohorts or other grafting techniques also limits the contextualization of our results.
Future studies should address these limitations by employing prospective, randomized, or multicenter designs with larger sample sizes, standardized selection criteria, and a systematic incorporation of long-term clinical outcomes and patient-reported measures.
5. Conclusions
The use of bovine pericardium in septoplasty has proven to be a promising strategy for preventing postoperative septal perforation in cases with bilateral opposing mucosal defects. With a 90% success rate and a low complication profile, it represents a viable and valuable surgical alternative for preserving septal integrity.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14134592/s1, Supplementary Video S1. The complete procedure video of the surgical technique and the placement of the bovine pericardium graft under microscopic visualization.
Author Contributions
Conceptualization, A.S.B. and J.M.V.A.; methodology, A.S.B., P.B.M., and J.M.V.A.; software, G.D.T., I.A.R., L.L.F., and J.M.V.A.; validation, A.S.B., P.B.M., G.D.T., I.A.R., W.A.S.-B., L.L.F., J.M.S.C., and J.M.V.A.; formal analysis, A.S.B., W.A.S.-B., and J.M.S.C.; investigation, A.S.B., P.B.M., G.D.T., I.A.R., W.A.S.-B., L.L.F., J.M.S.C., and J.M.V.A.; resources, A.S.B., P.B.M., and G.D.T.; data curation, A.S.B., P.B.M., L.L.F., J.M.S.C., and J.M.V.A.; writing—original draft preparation, A.S.B., P.B.M., G.D.T., I.A.R., W.A.S.-B., L.L.F., J.M.S.C., and J.M.V.A.; writing—review and editing, A.S.B., P.B.M., G.D.T., I.A.R., W.A.S.-B., L.L.F., J.M.S.C., and J.M.V.A.; visualization, A.S.B., G.D.T., I.A.R., and J.M.V.A.; supervision, A.S.B. and J.M.V.A.; project administration, A.S.B., J.M.S.C., and J.M.V.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The use of bovine pericardium in the nasal cavities and anterior skull base is a common practice in the sinonasal area. Given the retrospective nature of the study, every participant was thoroughly informed and provided explicit consent for the processing of their epidemiological data, in compliance with the requirements of the Clinical Research Ethics Committee at Fundación Jiménez Díaz University Hospital.
Informed Consent Statement
Informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available in the file Data.xls, which accompanies this publication.
Acknowledgments
This article is a revised and expanded version of oral communication papers entitled “Pericardio bovino como rescate en las septoplastias con riesgo de perforación septal”, which was presented at the XXIV Spring Meeting of the Commission of Rhinology, Allergy, and Anterior Skull Base of the Spanish Society of Otolaryngology and Head and Neck (SEORL-CCC); as well as in the 75th edition of the SEORL-CCC Congress [24,25].
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviation is used in this manuscript:
| FESS | Functional Endoscopic Sinus Surgery |
References
- Taylor, C.M.; Bansberg, S.F.; Marino, M.J. Assessing Patient Symptoms Due to Nasal Septal Perforation: Development and Validation of the NOSE-Perf Scale. Otolaryngol. Head Neck Surg. 2021, 165, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Rettinger, G.; Kirsche, H. Complications in septoplasty. Facial Plast. Surg. 2006, 22, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Bloom, J.D.; Kaplan, S.E.; Bleier, B.S.; Goldstein, S.A. Septoplasty complications: Avoidance and management. Otolaryngol. Clin. N. Am. 2009, 42, 463–481. [Google Scholar] [CrossRef]
- Daudia, A.; Alkhaddour, U.; Sithole, J.; Mortimore, S. A prospective objective study of the cosmetic sequelae of nasal septal surgery. Acta Otolaryngol. 2006, 126, 1201–1205. [Google Scholar] [CrossRef]
- Muhammad, I.A.; Rahman, N.U. Complications of the surgery for deviated nasal septum. J. Coll. Physicians Surg. Pak. 2003, 13, 565–568. [Google Scholar] [PubMed]
- Villacampa Aubá, J.M.; Sánchez Barrueco, A.; Díaz Tapia, G.; Santillán Coello, J.M.; Escobar Montatixe, D.A.; González Galán, F.; Mahillo Fernández, I.; González Márquez, R.; Cenjor Español, C. Microscopic approach for repairing nasal septal perforations using bilateral advancement flaps. Eur. Arch. Otorhinolaryngol. 2019, 276, 101–106. [Google Scholar] [CrossRef]
- Garaycochea, O.; Santamaría-Gadea, A.; Alobid, I. State-of-the-art: Septal perforation repair. Curr. Opin. Otolaryngol. Head Neck Surg. 2023, 31, 11–16. [Google Scholar] [CrossRef]
- Santamaría-Gadea, A.; Langdon, C.; Alobid, I. Extended Anterior Ethmoidal Artery Flap: Novel Endoscopic Technique for Large Septal Perforation. Laryngoscope 2022, 132, 298–300. [Google Scholar] [CrossRef]
- Santamaría-Gadea, A.; Vaca, M.; de Los Santos, G.; Alobid, I.; Mariño-Sánchez, F. Greater palatine artery pedicled flap for nasal septal perforation repair: Radiological study and case series. Eur Arch Otorhinolaryngol. 2021, 278, 2115–2121. [Google Scholar] [CrossRef]
- Alobid, I.; Santamaría-Gadea, A.; Mariño-Sánchez, F. Endoscopic “Racket-on-Donut” Technique for Large Anterior Nasoseptal Perforations. Laryngoscope 2024, 134, 143–147. [Google Scholar] [CrossRef]
- Jasso-Victoria, R.; Olmos-Zuñiga, J.R.; Gutierrez-Marcos, L.M.; Sotres-Vega, A.; Manjarrez Velazquez, J.R.; Gaxiola-Gaxiola, M.; Avila-Chavez, A.; Moreno, G.A.; Santillan-Doherty, P. Usefulness of bovine pericardium as interpositional graft in the surgical repair of nasal septal perforations (experimental study). J. Investig. Surg. Off. J. Acad. Surg. Res. 2003, 16, 209–217. [Google Scholar] [CrossRef]
- Baharuddin, A.; Go, B.T.; Firdaus, M.N.; Abdullah, J. Bovine pericardium for dural graft: Clinical results in 22 patients. Clin. Neurol. Neurosurg. 2002, 104, 342–344. [Google Scholar] [CrossRef]
- de Dorlodot, C.; De Bie, G.; Deggouj, N.; Decat, M.; Gérard, J.M. Are bovine pericardium underlay xenograft and butterfly inlay autograft efficient for transcanal tympanoplasty? Eur. Arch. Otorhinolaryngol. 2015, 272, 327–331. [Google Scholar] [CrossRef]
- Titirungruang, C.K.; Charakorn, N.; Chaitusaney, B.; Hirunwiwatkul, P. Is postoperative nasal packing after septoplasty safe? A systematic review and meta-analysis of randomized controlled studies. Rhinology 2021, 59, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Del Toro López, M.D.; Arias Díaz, J.; Balibrea, J.M.; Benito, N.; Canut Blasco, A.; Esteve, E.; Horcajada, J.P.; Mesa, J.D.R.; Vázquez, A.M.; Casares, C.M. Executive summary of the Consensus Document of the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) and of the Spanish Association of Surgeons (AEC) in antibiotic prophylaxis in surgery. Enferm. Infecc. Microbiol. Clin. (Engl. Ed.). 2021, 39, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Alegre Edo, B.; Rojas-Lechuga, M.J.; Quer-Castells, M.; González-Sánchez, N.; Lopez-Chacon, M.; Hopkins, C.; Alobid, I. Quality of Life in Symptomatic Septal Perforation. Laryngoscope 2024, 134, 4480–4487. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.M.; Bansberg, S.F.; Marino, M.J. Validated Symptom Outcomes Following Septal Perforation Repair: Application of the NOSE-Perf Scale. Laryngoscope 2024, 134, 3067–3072. [Google Scholar] [CrossRef]
- Na, Y.; Kwon, K.W.; Jang, Y.J. Impact of nasal septal perforation on the airflow and air-conditioning characteristics of the nasal cavity. Sci Rep. 2024, 14, 2337. [Google Scholar] [CrossRef]
- Tiwari, N.; Kumar, A.; Ramamurthy, H.R.; Kumar, V.; Khare, A. Tissue engineered decellularized bovine pericardium as prosthetic material in paediatric cardiac surgery. Indian J. Thorac. Cardiovasc. Surg. 2025, 41, 35–40. [Google Scholar] [CrossRef]
- Ren, L.; Sun, Y.; Wang, H.; Yuan, P.; Wu, M.; Xiong, J. Mid-Term Outcomes of Common Femoral Patch Angioplasty in Iliofemoral Occlusive Diseases: Bovine Pericardial Patch Versus Great Saphenous Vein Patch. Ann. Vasc. Surg. 2025, 114, 106–115. [Google Scholar] [CrossRef]
- Avorito, L.A.; Vieiralves, R.R.; Batista, A.V.; Silva, R.P.; Hauschild, L.O.; Uneda, L.A.M.; Resende, J.A.D. Aldehyde free—Bovine Pericardium—A New Option of Graft in Urethral Stricture Treatment. Int. Braz. J. Urol. 2025, 51, e20249928. [Google Scholar] [CrossRef] [PubMed]
- Savino, G.; Mandarà, E.; Calandriello, L.; Dickmann, A.; Petroni, S. A Modified One-Stage Early Correction of Blepharophimosis Syndrome Using Tutopatch Slings. Orbit 2015, 34, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Achinger, K.G.; Williams, L.N. Trends in CSF Leakage Associated with Duraplasty in Infratentorial Procedures over the Last 20 Years: A Systematic Review. Crit. Rev. Biomed. Eng. 2023, 51, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Benavent Marín, M.P.; Sánchez Barrueco, Á.; Diaz Tapia, G.; Santillán Coello, J.M.; López Flórez, L.; Morales Domínguez, J.; Villacampa Aubá, J.M. Oral Communication: Pericardio bovino como rescate en las septoplastias con riesgo de perforación septal. In Proceedings of the XXIV Spring Meeting of the Commission of Rhinology, Allergy, and Anterior Skull Base of the Spanish Society of Otolaryngology and Head and Neck (SEORL-CCC), Madrid, Spain, 11–12 May 2024. [Google Scholar]
- Benavent Marín, M.P.; Sánchez Barrueco, Á.; Diaz Tapia, G.; Santillán Coello, J.M.; López Flórez, L.; Morales Domínguez, J.; Villacampa Aubá, J.M. Oral Communication: Pericardio bovino como rescate en las septoplastias con riesgo de perforación septal. In Proceedings of the 75th Edition of the SEORL-CCC Congress, Madrid, Spain, 23–26 October 2024. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).