Risk Factors for Common Bile Duct Stones in Patients with Previous Cholecystectomy: A Multicenter Prospective Proof-of-Concept Study
Abstract
1. Introduction
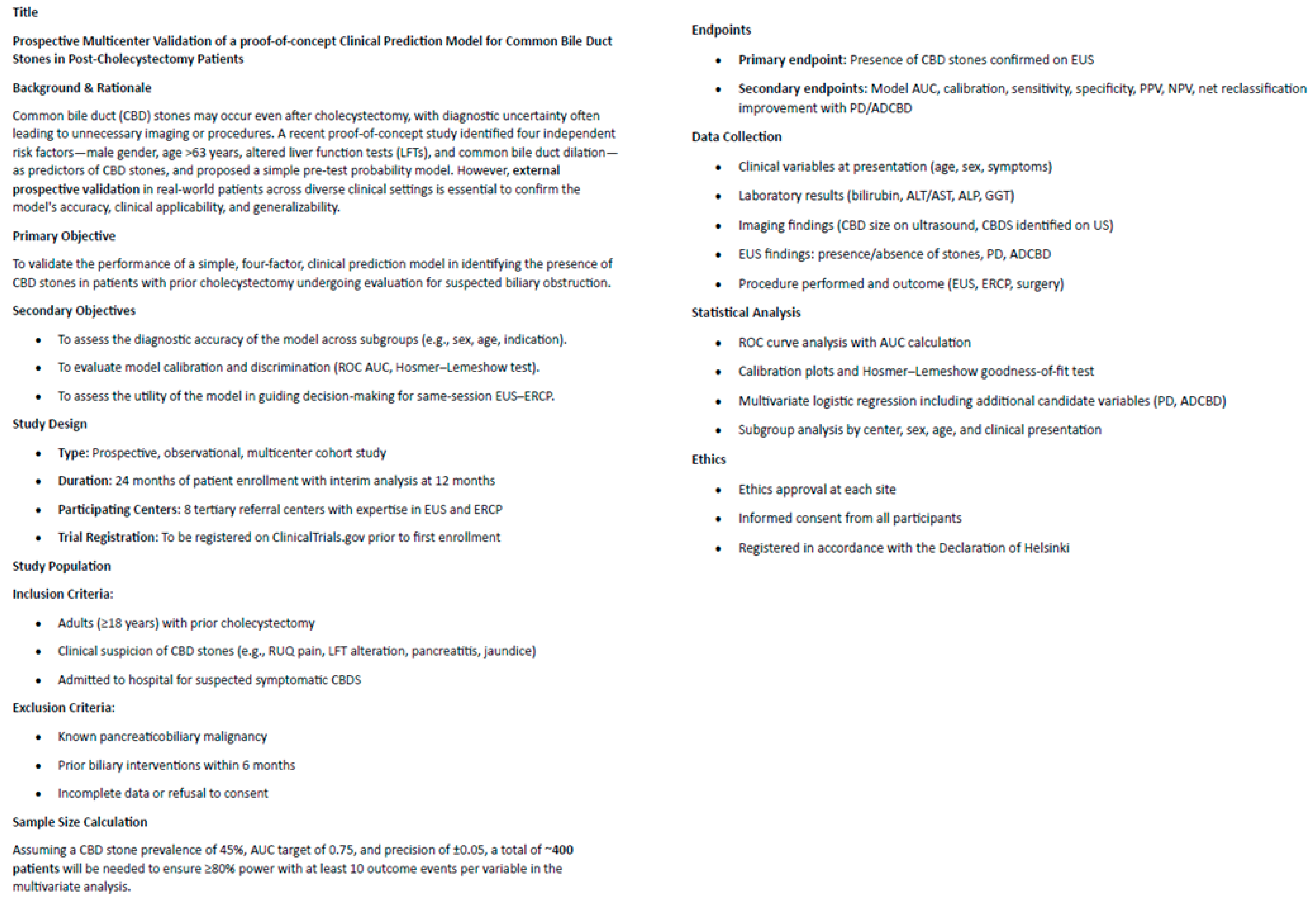
2. Materials and Methods
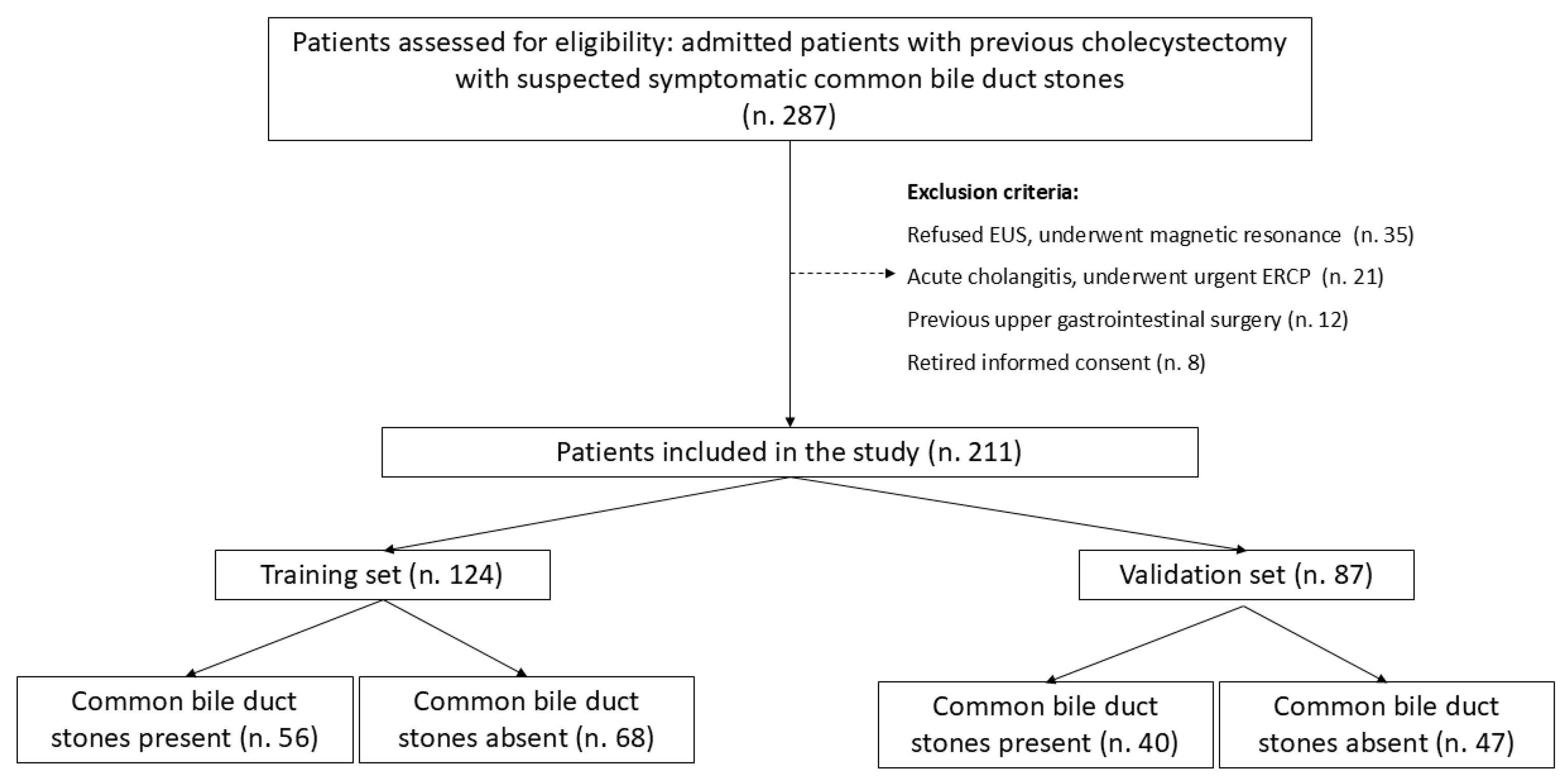
2.1. Study Design
2.2. Study Population and Eligibility Criteria
2.3. Clinical and Laboratory Assessment
2.4. Imaging Modalities and Diagnostic Approach
2.5. Definitions and Outcome Measures
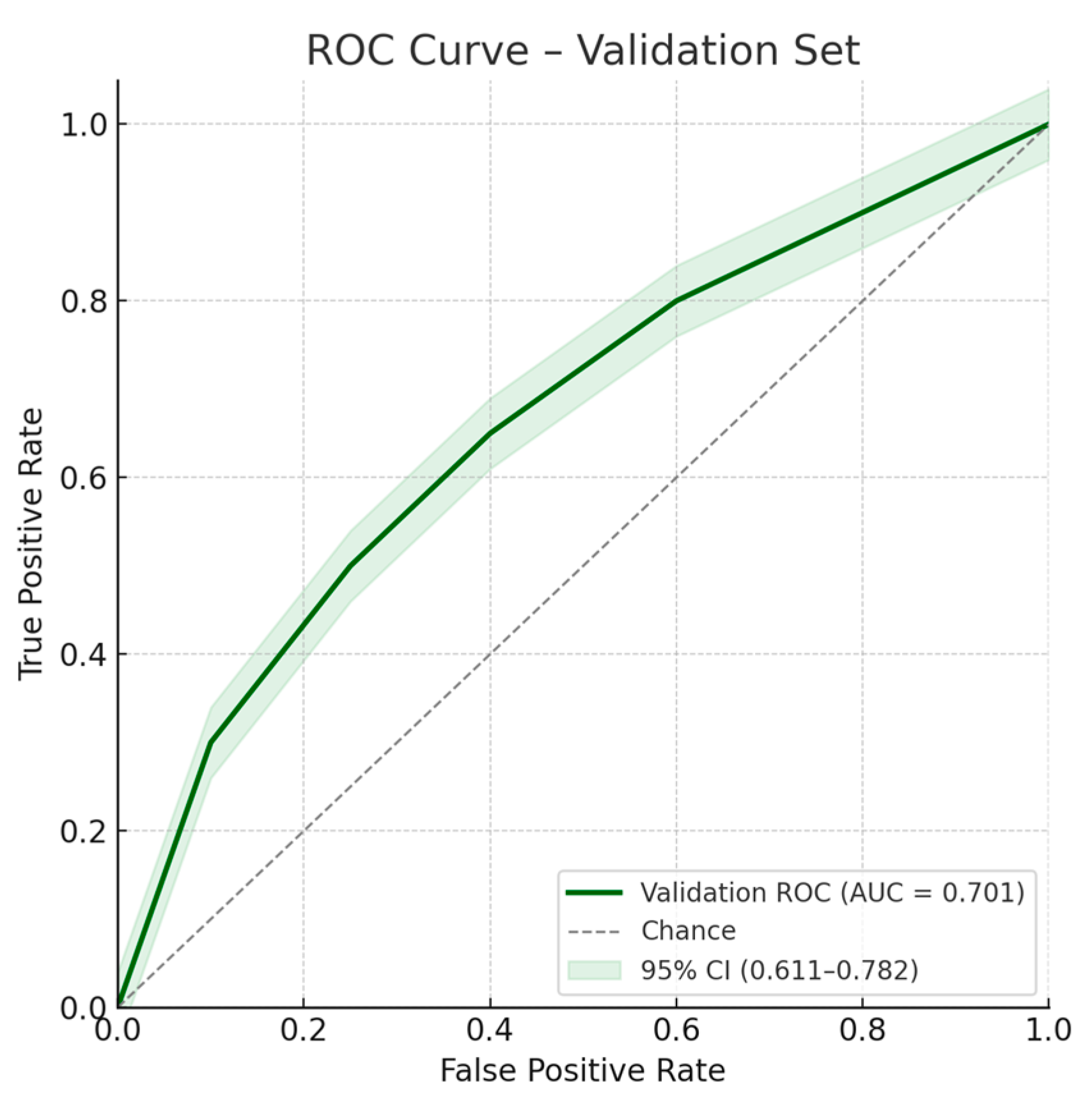
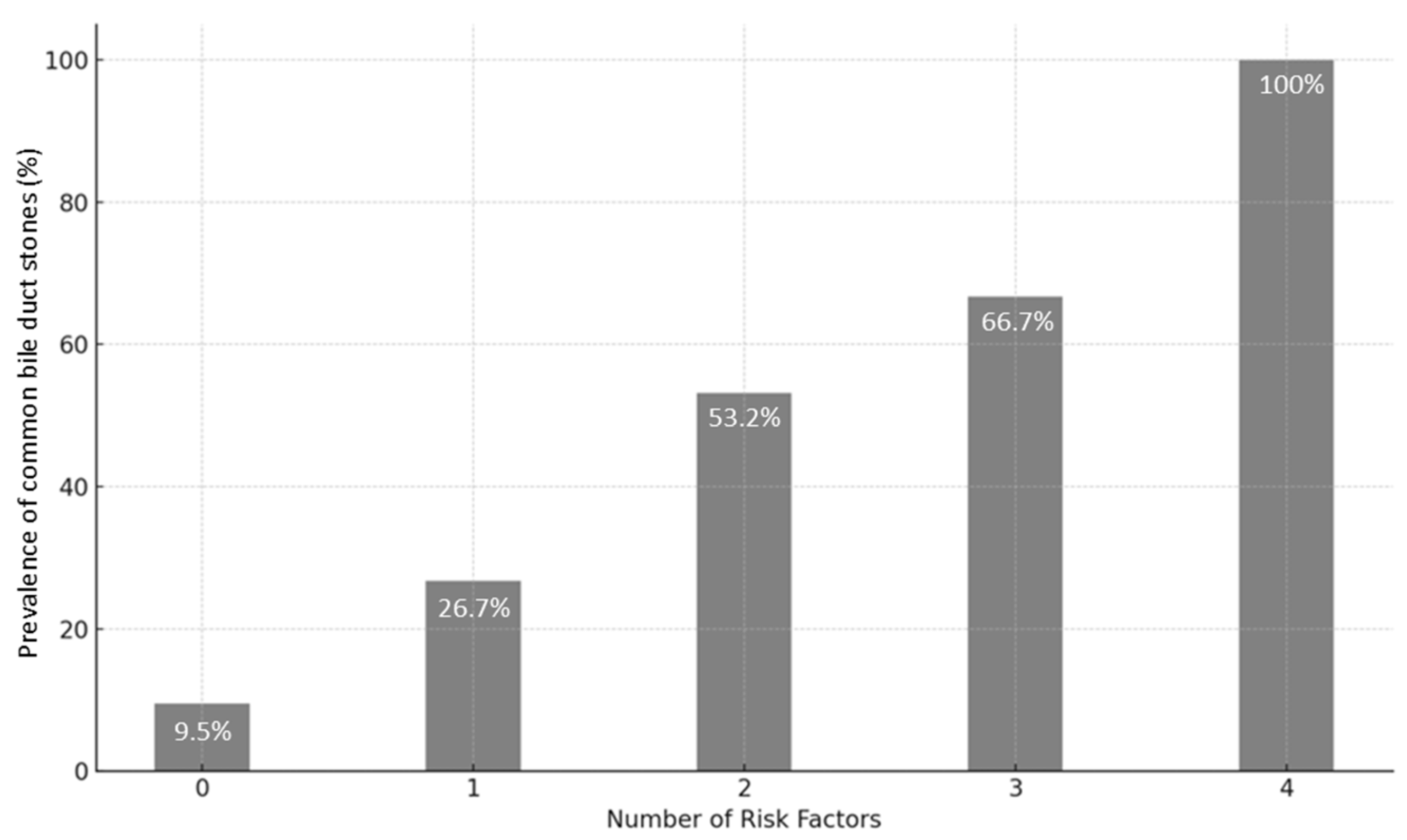
2.6. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
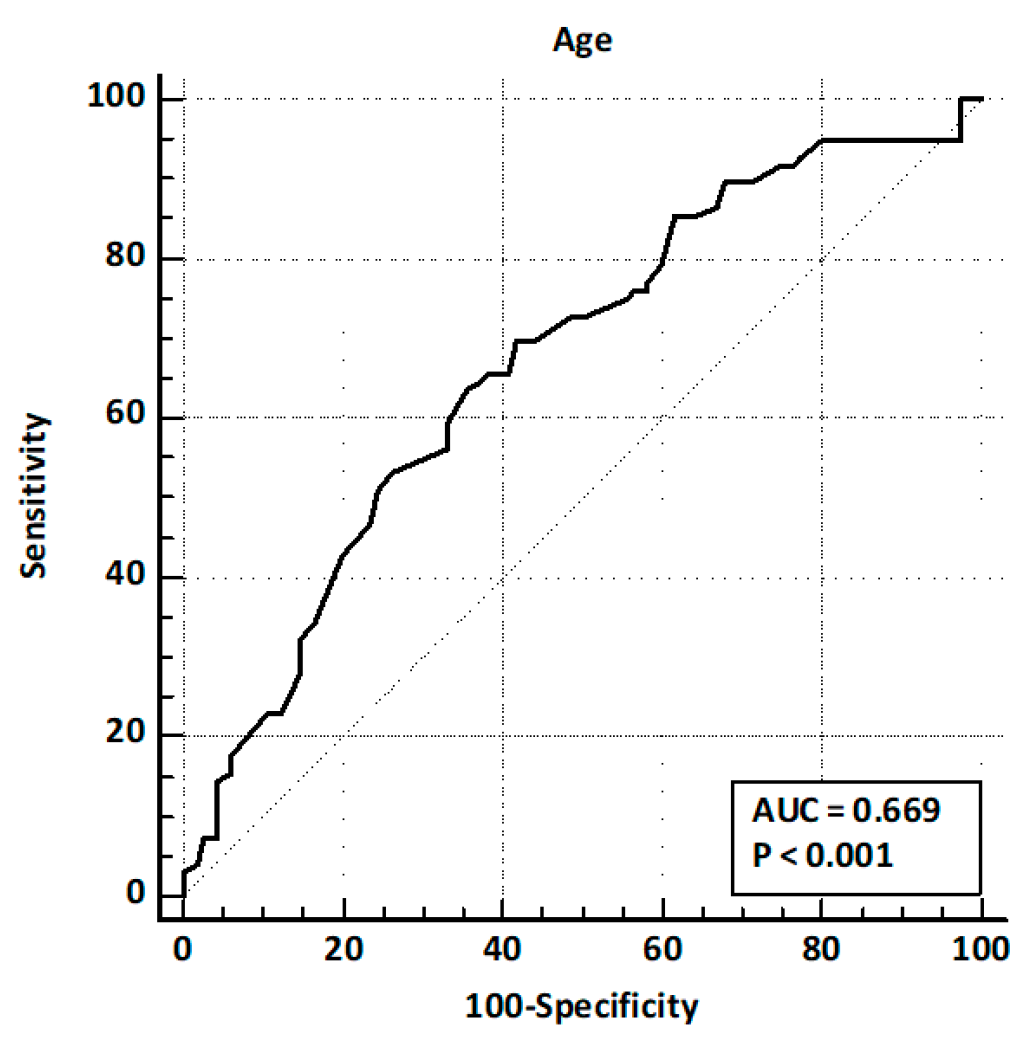
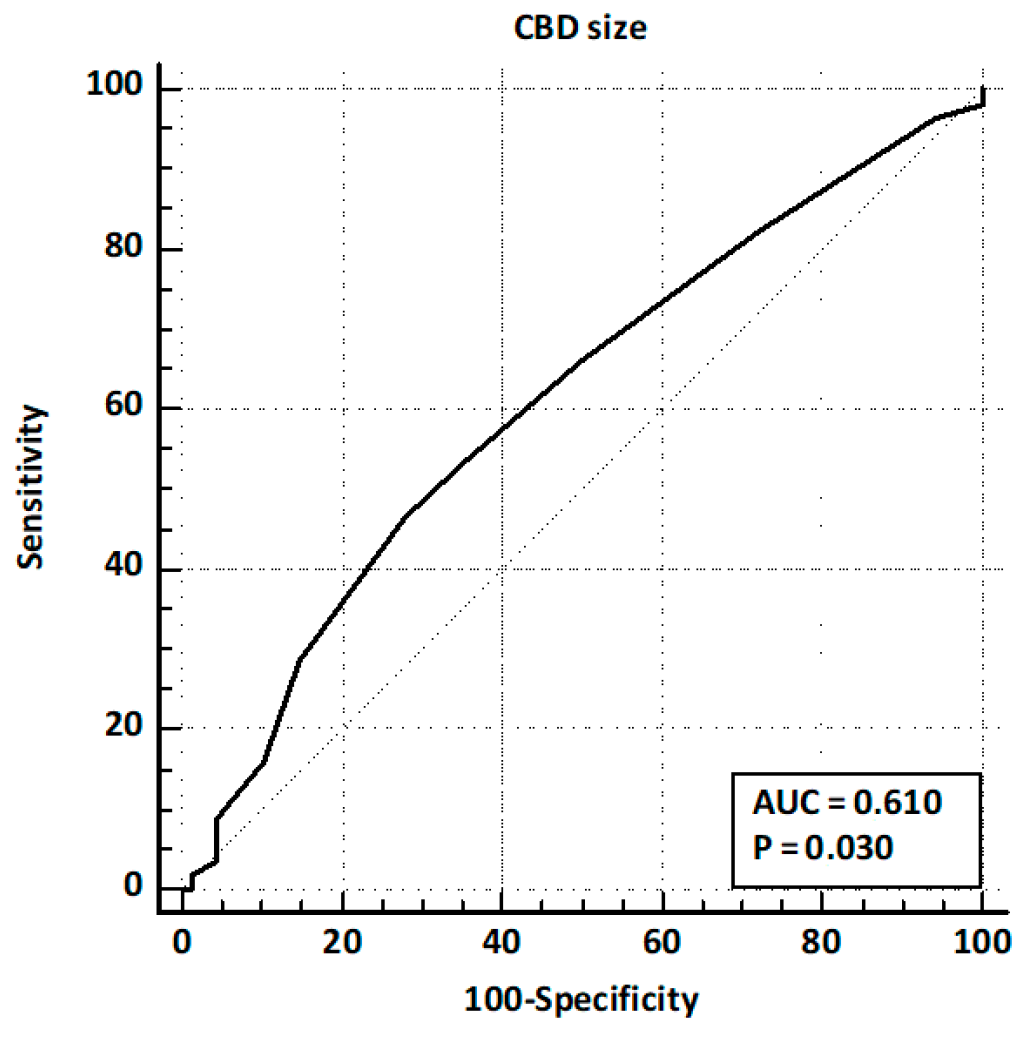
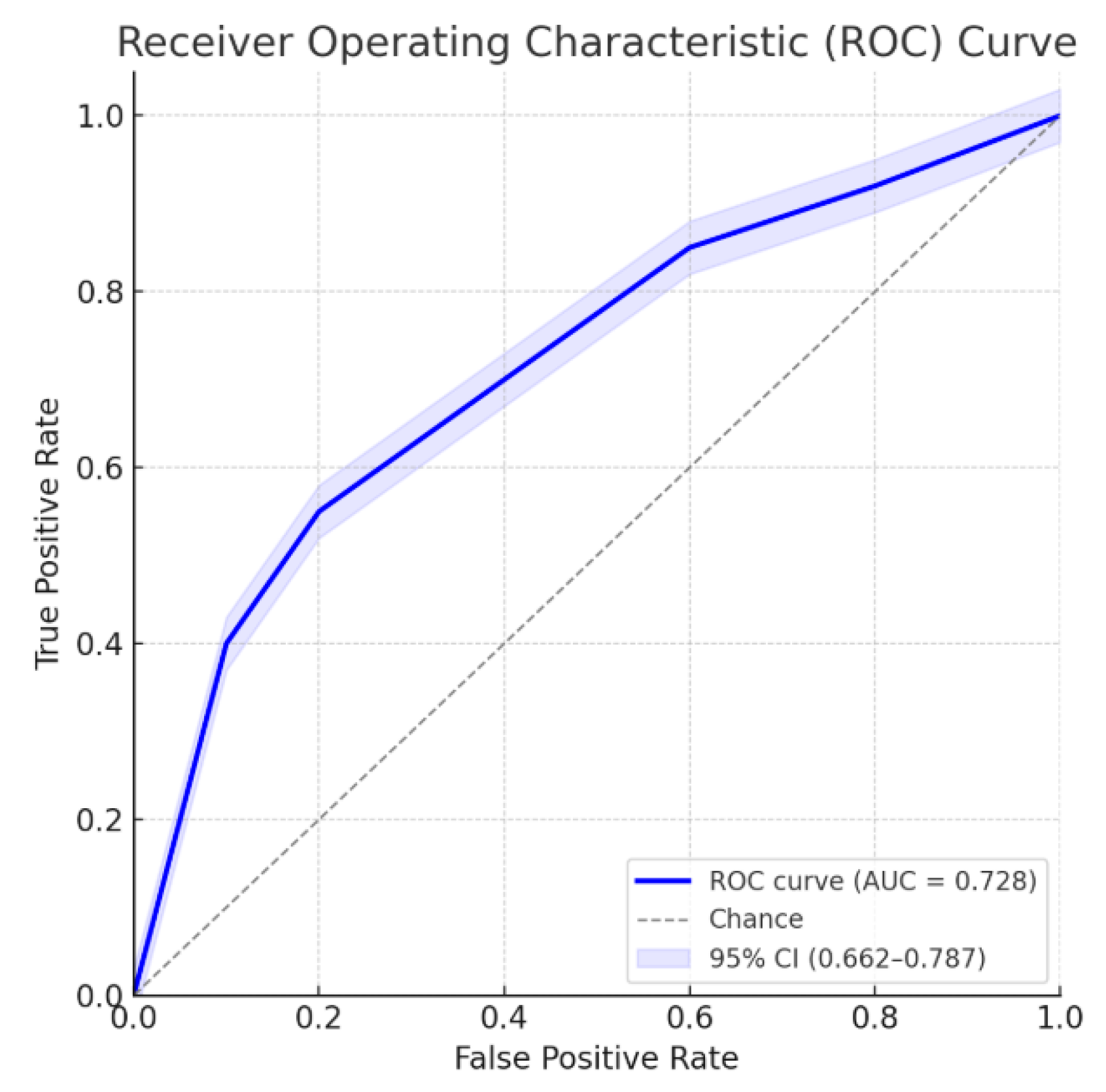
3.2. Model for Suspected CBD Stone
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBD | Common Bile Duct |
| EST | Endoscopic Biliary Sphincterotomy |
| EUS | Endoscopic Ultrasound |
| ERCP | Endoscopic Retrograde Cholangiopancreatography |
| PAD | Periampullary Diverticulum |
| LFTs | Liver Function Tests |
| OR | Odds Ratio |
| CI | Confidence Interval |
| IQR | Interquartile Range |
| TBIL | Total Bilirubin |
| WBC | White Blood Cell (count) |
| MRCP | Magnetic Resonance Cholangiopancreatography |
References
- European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J. Hepatol. 2016, 65, 146–181. [Google Scholar] [CrossRef]
- Manes, G.; Paspatis, G.; Aabakken, L.; Anderloni, A.; Arvanitakis, M.; Ah-Soune, P.; Barthet, M.; Domagk, D.; Dumonceau, J.-M.; Gigot, J.-F.; et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2019, 51, 472–491. [Google Scholar] [CrossRef]
- Williams, E.J.; Green, J.; Beckingham, I.; Parks, R.; Martin, D.; Lombard, M. Guidelines on the management of common bile duct stones (CBDS). Gut 2008, 57, 1004–1021. [Google Scholar] [CrossRef]
- Kama, N.A.; Atili, M.; Doganay, M.; Kologlu, M.; Reis, E.; Dolapci, M. Practical recommendations for the prediction and management of common bile duct stones in patients with gallstones. Surg. Endosc. 2001, 15, 942–945. [Google Scholar] [CrossRef]
- Tse, F.; Barkun, J.S.; Barkun, A.N. The elective evaluation of patients with suspected choledocholithiasis undergoing laparoscopic cholecystectomy. Gastrointest. Endosc. 2004, 60, 437–448. [Google Scholar] [CrossRef]
- Tse, F.; Liu, L.; Barkun, A.N.; Armstrong, D.; Moayyedi, P. EUS: A meta-analysis of test performance in suspected choledocholithiasis. Gastrointest. Endosc. 2008, 67, 235–244. [Google Scholar] [CrossRef]
- Maple, J.T.; Ben-Menachem, T.; Anderson, M.A.; Appalaneni, V.; Banerjee, S.; Cash, B.D.; Fisher, L.; Harrison, M.E.; Fanelli, R.D.; Fukami, N.; et al. for the ASGE Standards of Practice Committee. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest. Endosc. 2010, 71, 1–9. [Google Scholar] [CrossRef]
- Polkowski, M.; Regula, J.; Tilszer, A.; Butruk, E. Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: A randomized trial comparing two management strategies. Endoscopy 2007, 39, 296–303. [Google Scholar] [CrossRef]
- Chawla, S.; Trick, W.E.; Gilkey, S.; Attar, B.M. Does cholecystectomy status influence the common bile duct diameter? A matched-pair analysis. Dig. Dis. Sci. 2010, 55, 1155–1160. [Google Scholar] [CrossRef]
- Sand, J.; Pakkala, S.; Nordback, I. Twenty to thirty year follow-up after cholecystectomy. Hepatogastroenterology 1996, 43, 534–537. [Google Scholar]
- Fusaroli, P.; Lisotti, A.; Syguda, A.; D’eRcole, M.C.; Maimone, A.; Fabbri, C.; Cennamo, V.; Cecinato, P.; Cariani, G.; Caletti, G. Reliability of endoscopic ultrasound in predicting the number and size of common bile duct stones before endoscopic retrograde cholangiopancreatography. Dig. Liver Dis. 2016, 48, 277–282. [Google Scholar] [CrossRef]
- Hajong, R.; Medhi, B.; Rabha, P.; Baruah, A.J.; Boruah, P.; Aggarwal, S.; Devi, K.M.; Ronrang, L.; Debnath, S. A Prospective Comparative Study of Laparoscopic Common Bile Duct Exploration and Endoscopic Retrograde Cholangiopancreatography for Managing Common Bile Duct Calculi. Cureus 2025, 17, e82827. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Lovrić, M.; Jukić, M.; Perko, Z. The Laparoscopic Cholecystectomy and Common Bile Duct Exploration: A Single-Step Treatment of Pediatric Cholelithiasis and Choledocholithiasis. Children 2022, 9, 1583. [Google Scholar] [CrossRef]
- Huang, J.; Hu, W.; Liu, J.; Tang, X.; Fan, Y.; Xu, L.; Liu, T.; Xiong, H.; Li, W.; Fu, X.; et al. Laparoscopic Transcystic Common Bile Duct Exploration: 8-Year Experience at a Single Institution. J. Gastrointest. Surg. 2023, 27, 555–564. [Google Scholar] [CrossRef]
- Shabanzadeh, D.M.; Sørensen, L.T.; Jørgensen, T. A Prediction Rule for Risk Stratification of Incidentally Discovered Gallstones: Results From a Large Cohort Study. Gastroenterology 2016, 150, 156–167. [Google Scholar] [CrossRef]
- Unalp-Arida, A.; Ruhl, C.E. Increasing gallstone disease prevalence and associations with gallbladder and biliary tract mortality in the US. Hepatology 2023, 77, 1882–1895. [Google Scholar] [CrossRef]
- Stender, S.; Nordestgaard, B.G.; Tybjaerg-Hansen, A. Elevated body mass index as a causal risk factor for symptomatic gallstone disease: A Mendelian randomization study. Hepatology 2013, 58, 2133–2141. [Google Scholar] [CrossRef]
- Gerbasi, L.; Gunsberger, T.; Santarelli, A.; Ashurst, J. Comparing the Sensitivity and Specificity of Computed Tomography and Ultrasound in the Diagnosis of Acute Cholecystitis in a Rural Setting. Cureus 2025, 17, e80316. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, H.; Bai, Z.; Xie, X.; Feng, Y. Current status of artificial intelligence analysis for the diagnosis of gallbladder diseases using ultrasonography: A scoping review. Transl. Gastroenterol. Hepatol. 2024, 10, 12. [Google Scholar] [CrossRef]
- Wu, X.; Li, K.; Kou, S.; Wu, X.; Zhang, Z. The Accuracy of Point-of-Care Ultrasound in the Detection of Gallbladder Disease: A Meta-analysis. Acad. Radiol. 2024, 31, 1336–1343. [Google Scholar] [CrossRef]
- Fusaroli, P.; Lisotti, A. EUS and ERCP in the Same Session for Biliary Stones: From Risk Stratification to Treatment Strategy in Different Clinical Conditions. Medicina 2021, 57, 1019. [Google Scholar] [CrossRef] [PubMed]
- Neves, J.A.C.; de Santiago, E.R.; Pohl, H.; Lorenzo-Zúñiga, V.; Cunha, M.F.; Voiosu, A.M.; Römmele, C.; Penman, D.G.; Albéniz, E.; Siau, K.; et al. Perspectives and awareness of endoscopy healthcare professionals on sustainable practices in gastrointestinal endoscopy: Results of the LEAFGREEN survey. Endoscopy 2024, 56, 355–363. [Google Scholar] [CrossRef]
- McCarty, T.R.; Hathorn, K.E.; Creighton, D.W.; AlSamman, M.A.; Thompson, C.C. Safety and sedation-associated adverse event reporting among patients undergoing endoscopic cholangiopancreatography: A comparative systematic review and meta-analysis. Surg. Endosc. 2021, 35, 6977–6989. [Google Scholar] [CrossRef] [PubMed]
- Masciangelo, G.; Cecinato, P.; Bacchilega, I.; Masetti, M.; Ferrari, R.; Zagari, R.M.; Napoleon, B.; Sassatelli, R.; Fusaroli, P.; Lisotti, A. Urgent ERCP performed with single-use duodenoscope (SUD) in patients with moderate-to-severe cholangitis: Single-center prospective study. Endosc. Int. Open 2024, 12, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Sha, Y.; Wang, Z.; Tang, R.; Wang, K.; Xu, C.; Chen, G. Modern Management of Common Bile Duct Stones: Breakthroughs, Challenges, and Future Perspectives. Cureus 2024, 16, e75246. [Google Scholar] [CrossRef]
- Gornals, J.B.; Moreno, R.; Castellote, J.; Loras, C.; Barranco, R.; Catala, I.; Xiol, X.; Fabregat, J.; Corbella, X. Single-session endosonography and endoscopic retrograde cholangiopancreatography for biliopancreatic diseases is feasible, effective and cost beneficial. Dig. Liver Dis. 2013, 45, 578–583. [Google Scholar] [CrossRef]
- Sbeit, W.; Kadah, A.; Shahin, A.; Khoury, T. Same day endoscopic retrograde cholangio-pancreatography immediately after endoscopic ultrasound for choledocholithiasis is feasible, safe and cost-effective. Scand. J. Gastroenterol. 2021, 56, 1243–1247. [Google Scholar] [CrossRef]
- Umefune, G.; Kogure, H.; Hamada, T.; Isayama, H.; Ishigaki, K.; Takagi, K.; Akiyama, D.; Watanabe, T.; Takahara, N.; Mizuno, S.; et al. Procalcitonin is a useful biomarker to predict severe acute cholangitis: A single-center prospective study. J. Gastroenterol. 2017, 52, 734–745. [Google Scholar] [CrossRef]
- Doğan, Ü.B.; Gümürdülü, Y.; Gölge, N.; Kara, B. Relationship of CA 19-9 with choledocholithiasis and cholangitis. Turk. J. Gastroenterol. 2011, 22, 171–177. [Google Scholar] [CrossRef]
- Burckhardt, O.; Peisl, S.; Rouiller, B.; Colinet, E.; Egger, B. Length of the Remnant Cystic Duct and Bile Duct Stone Recurrence: A Case–Control Study. J. Gastrointest. Surg. 2023, 27, 1122–1129. [Google Scholar] [CrossRef]
- Wen, N.; Wang, Y.; Cai, Y.; Nie, G.; Yang, S.; Wang, S.; Xiong, X.; Li, B.; Lu, J.; Cheng, N. Risk factors for recurrent common bile duct stones: A systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2023, 17, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Shi, L.; Wang, J.; Guo, S.; Zhu, S. The value of endoscopic duodenal papilloplasty with titanium clip in improving post-operative complications of choledocholithiasis. Cir. Cir. 2024, 92, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yang, T. The effect of pre-operative biliary drainage in resectable periampullary lesions: A systematic review and meta-analysis. Cir. Cir. 2024, 92, 338–346. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total (No. 211) | Training Set (No. 124) | Validation Set (No. 87) | p Value ‡ |
|---|---|---|---|---|
| Demographics | ||||
| Gender (male), No. (%) | 54 (25.6%) | 33 (26.6%) | 21 (24.1%) | 0.75 a |
| Age (years), median [IQR] | 66 [49–75] | 65.5 [49–75] | 68 [49.25–76] | 0.78 b |
| Time from cholecystectomy (months) | 32 [5–60] | 20 [6–55] | 36 [9–60] | 0.29 b |
| Clinical presentation | ||||
| Abdominal pain, No. (%) | 164 (77.7%) | 96 (77.4%) | 68 (78.2%) | 1.00 a |
| Acute pancreatitis, No. (%) | 56 (26.5%) | 28 (22.6%) | 28 (32.2%) | 0.15 a |
| Hyperbilirubinemia, No. (%) | 64 (30.3%) | 27 (21.8%) | 37 (42.5%) | 0.001 a |
| Biochemistry | ||||
| Liver function test alteration, No. (%) | 129 (61.1%) | 66 (53.2%) | 63 (72.4%) | 0.01 a |
| Imaging findings on US | ||||
| Common bile duct dilation, No. (%) | 79 (37.4%) | 45 (36.3%) | 34 (39.1%) | 0.77 a |
| Common bile duct stones, No. (%) | 12 (5.7%) | 8 (6.5%) | 4 (4.6%) | 0.88 a |
| EUS results | ||||
| Common bile duct stones, No. (%) | 96 (45.5%) | 56 (45.2%) | 40 (46.0%) | 1.00 a |
| Periampullary diverticulum, No. (%) | 15 (7.1%) | 10 (8.1%) | 5 (5.7%) | 0.86 a |
| Odds Ratio [95% C.I.] | p Value | Odds Ratio [95% C.I.] | p Value | Odds Ratio [95% C.I.] | p Value | |
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis (stepwise) | Multivariate analysis (Enter) | ||||
| Gender (male) | 1.91 [1.02–3.57] | 0.04 | 2.54 [1.26–5.09] | 0.009 | 2.53 [1.26–5.09] | 0.009 |
| Age (>63 years) | 3.22 [1.82–5.71] | <0.001 | 3.06 [1.63–5.72] | <0.001 | 3.04 [1.62–5.70] | 0.0005 |
| Time from cholecystectomy | 1.02 [0.97–1.12] | 0.32 | --- | --- | --- | --- |
| Recent cholecystectomy | 0.62 [0.21–3.28] | 0.64 | --- | --- | --- | --- |
| Abdominal pain | 0.93 [0.49–1.79] | 0.84 | --- | --- | --- | --- |
| Acute pancreatitis | 0.95 [0.52–1.76] | 0.88 | --- | --- | --- | --- |
| Hyperbilirubinemia | 1.86 [1.03–3.37] | 0.04 | NS * | NS * | 1.54 [0.77–3.10] | 0.22 |
| Alkaline phosphatase > 125 U/L | 1.78 [0.94–3.22] | 0.11 | --- | --- | --- | --- |
| AST > 1.5 upper limit normal | 1.45 [0.60–2.45] | 0.54 | --- | --- | --- | --- |
| ALT > 1.5 upper limit normal | 1.56 [0.55–2.02] | 0.24 | --- | --- | --- | --- |
| LFTs alteration | 2.15 [1.21–3.81] | <0.001 | 2.62 [1.40–4.91] | 0.003 | 2.26 [1.15–4.42] | 0.002 |
| CBD dilation on US | 2.71 [1.53–4.81] | <0.001 | 2.46 [1.31–4.65] | 0.005 | 2.53 [1.34–4.81] | 0.005 |
| CBD stones on US | 18.2 [0.21–126.3] | 0.66 | --- | --- | --- | --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lisotti, A.; Togliani, T.; Masciangelo, G.; Bruni, A.; Rakichevikj, E.; Vilmann, P.; Mirante, V.G.; Fusaroli, P. Risk Factors for Common Bile Duct Stones in Patients with Previous Cholecystectomy: A Multicenter Prospective Proof-of-Concept Study. J. Clin. Med. 2025, 14, 4532. https://doi.org/10.3390/jcm14134532
Lisotti A, Togliani T, Masciangelo G, Bruni A, Rakichevikj E, Vilmann P, Mirante VG, Fusaroli P. Risk Factors for Common Bile Duct Stones in Patients with Previous Cholecystectomy: A Multicenter Prospective Proof-of-Concept Study. Journal of Clinical Medicine. 2025; 14(13):4532. https://doi.org/10.3390/jcm14134532
Chicago/Turabian StyleLisotti, Andrea, Thomas Togliani, Graziella Masciangelo, Angelo Bruni, Emilija Rakichevikj, Peter Vilmann, Vincenzo Giorgio Mirante, and Pietro Fusaroli. 2025. "Risk Factors for Common Bile Duct Stones in Patients with Previous Cholecystectomy: A Multicenter Prospective Proof-of-Concept Study" Journal of Clinical Medicine 14, no. 13: 4532. https://doi.org/10.3390/jcm14134532
APA StyleLisotti, A., Togliani, T., Masciangelo, G., Bruni, A., Rakichevikj, E., Vilmann, P., Mirante, V. G., & Fusaroli, P. (2025). Risk Factors for Common Bile Duct Stones in Patients with Previous Cholecystectomy: A Multicenter Prospective Proof-of-Concept Study. Journal of Clinical Medicine, 14(13), 4532. https://doi.org/10.3390/jcm14134532






