Influence of Maxillofacial Morphology on Temporomandibular Joint Degenerative Alterations and Condyle Position Assessed by CBCT in Class II Malocclusion Adult Patients—A Cross-Sectional Study
Abstract
1. Introduction
Aim of the Study
2. Materials and Methods
2.1. Study Population
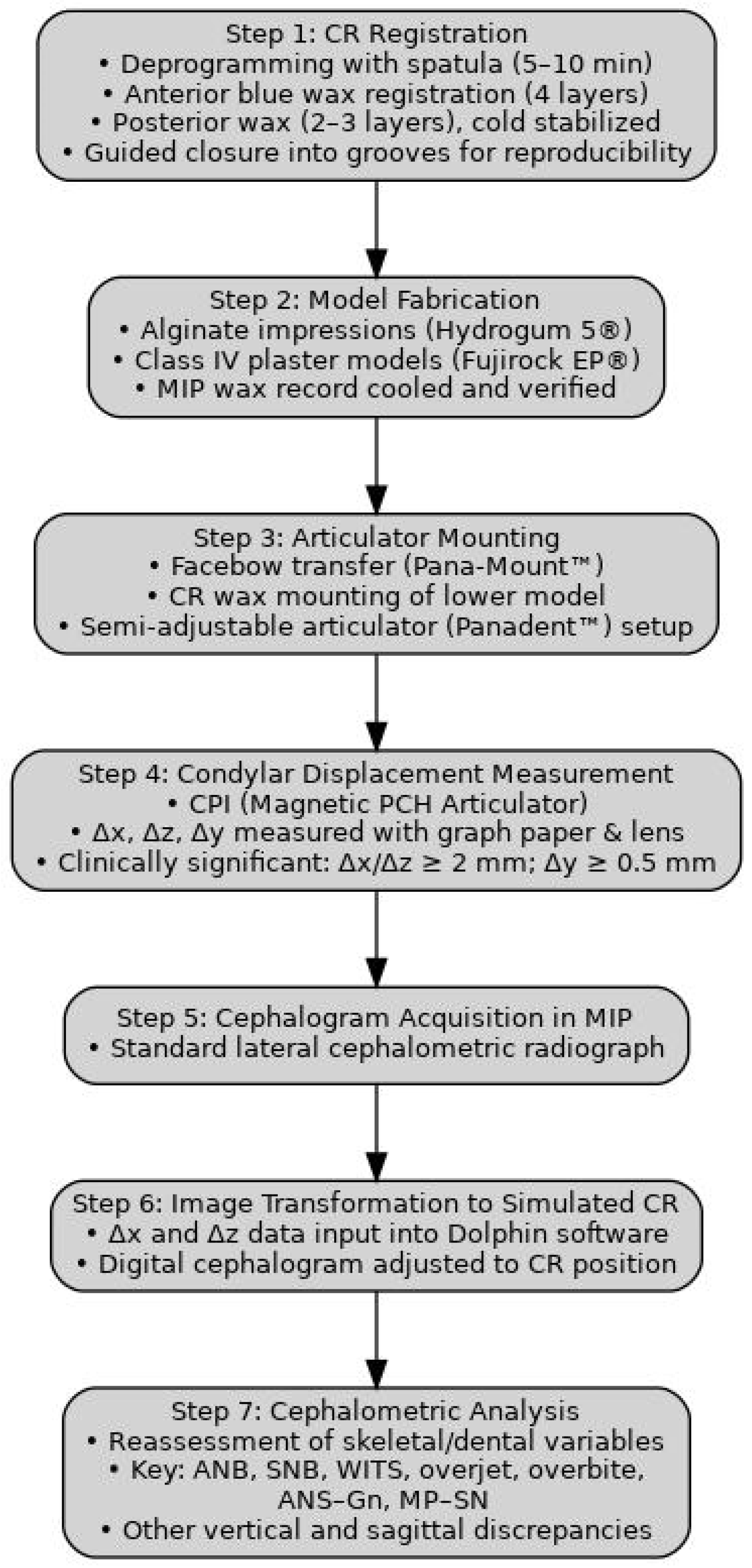
2.2. Imaging Studies
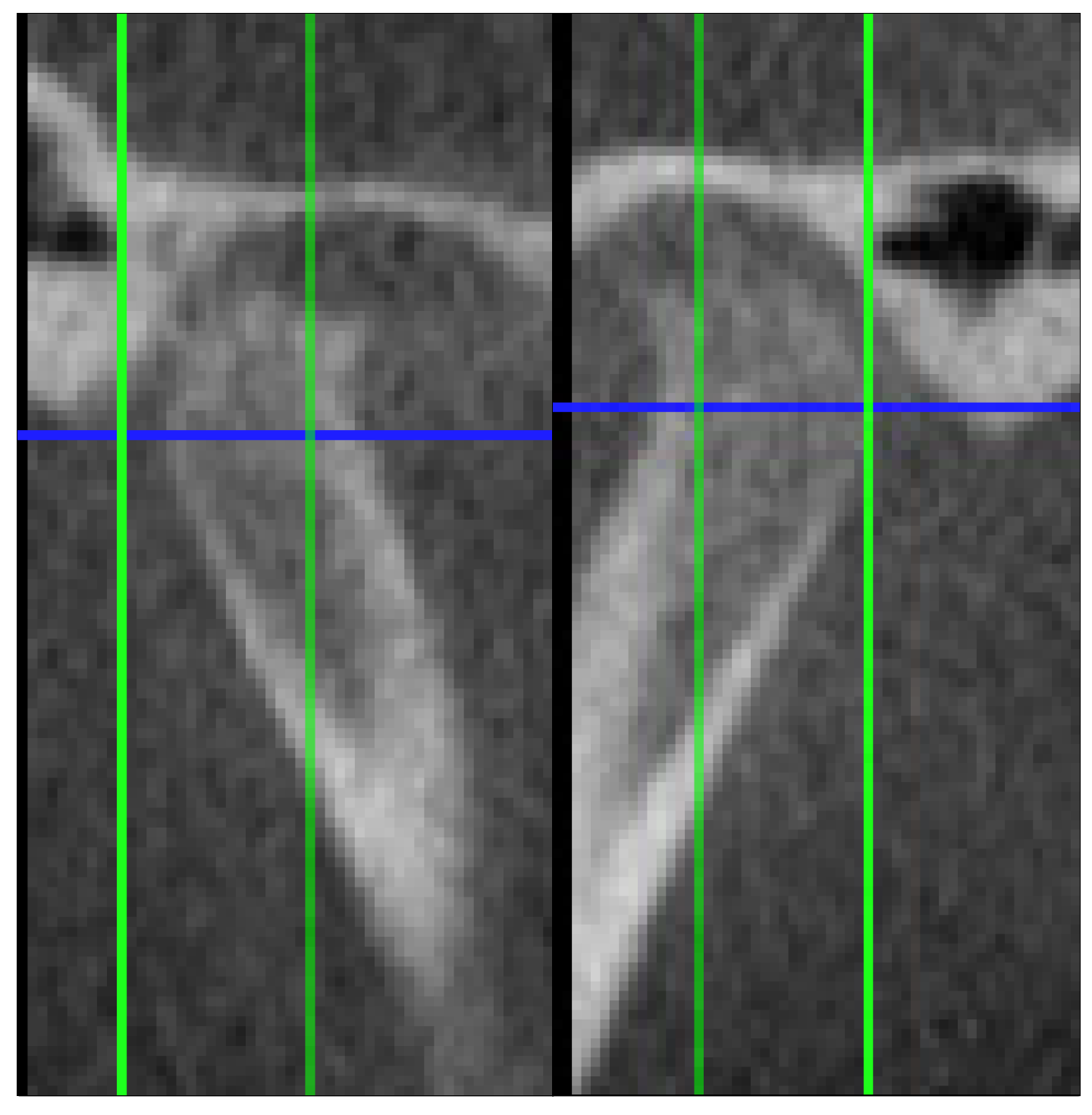
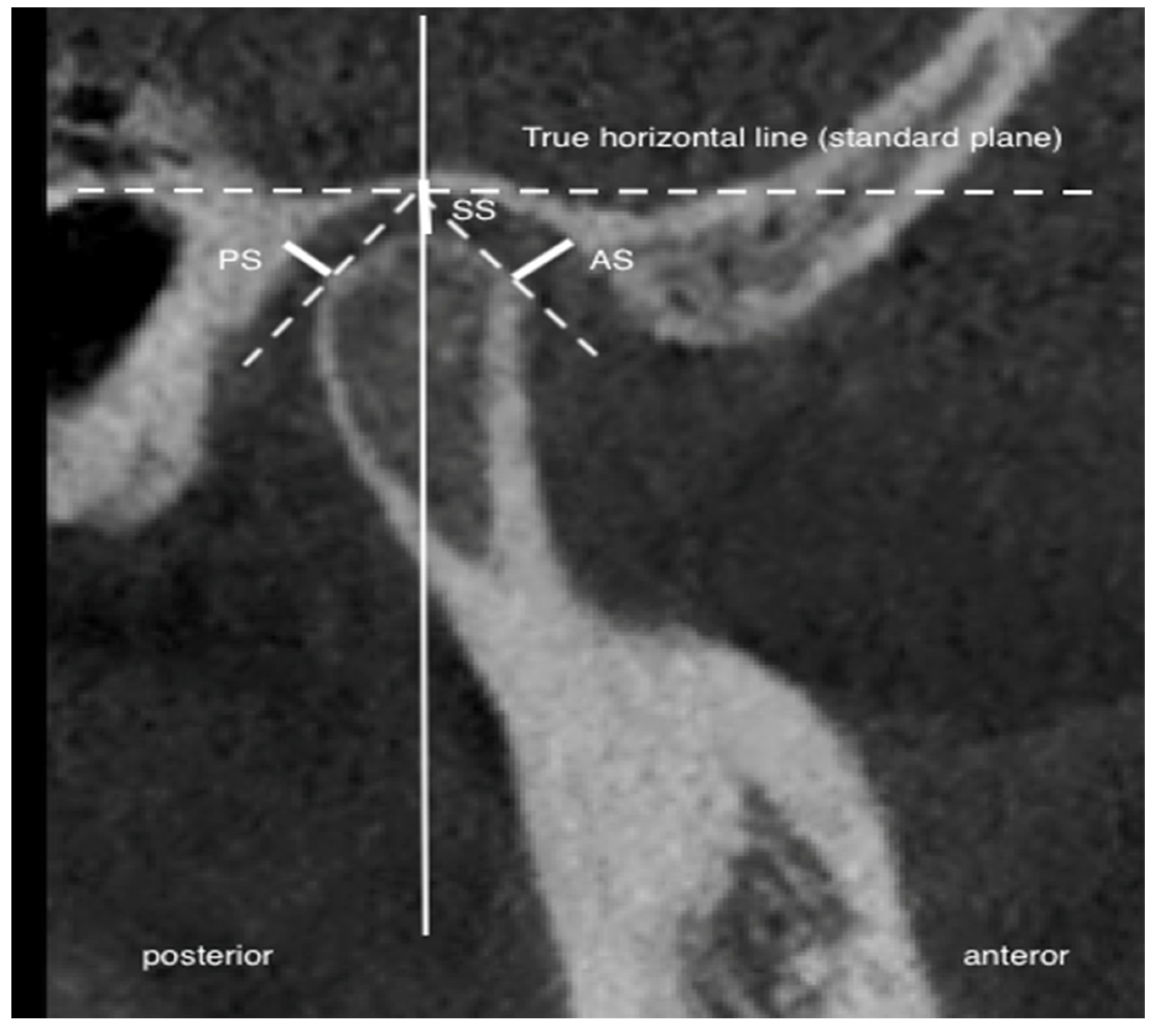
2.3. Joint Space Assessment
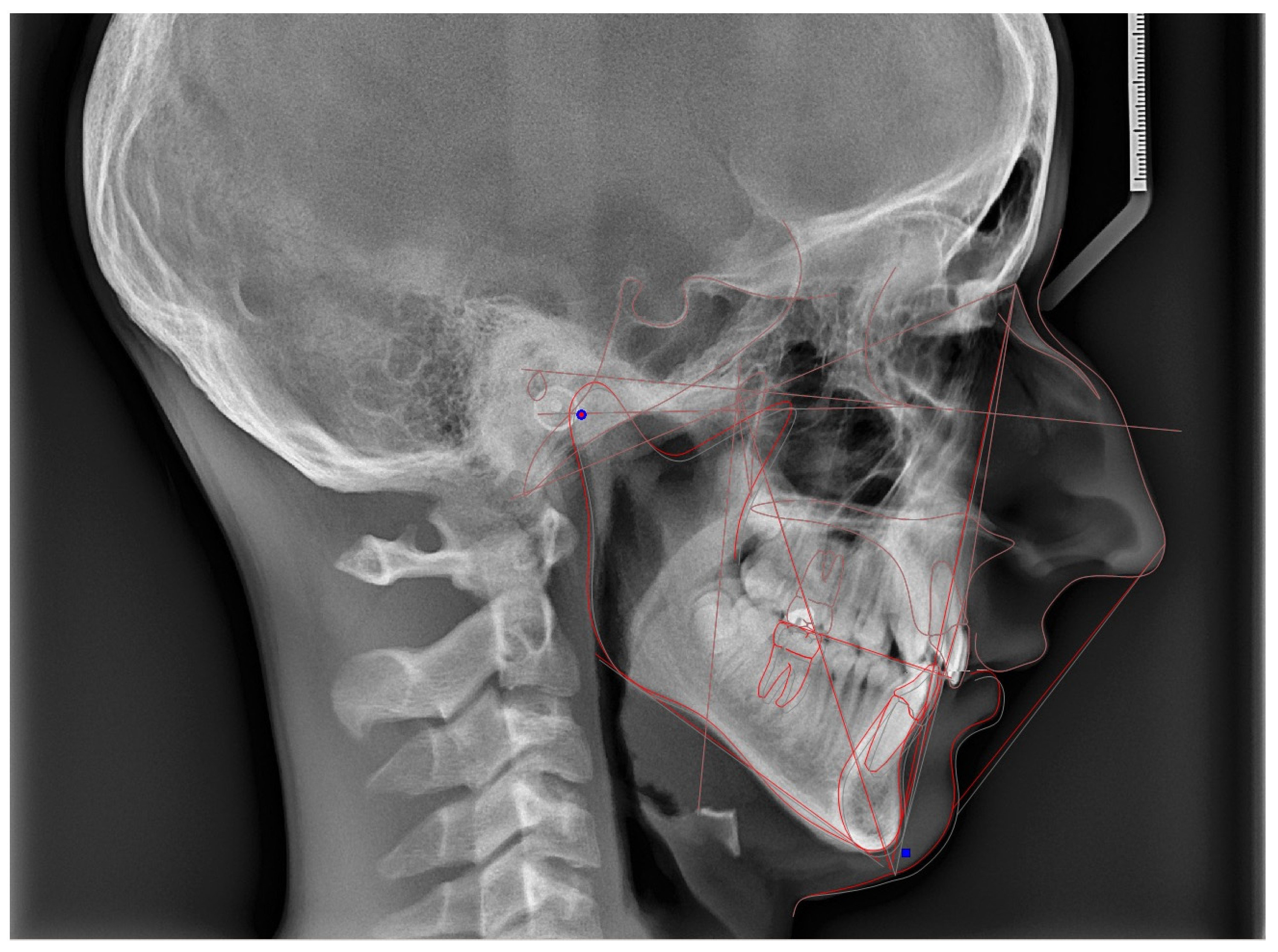
2.4. Cephalometric Analysis
2.5. MIP-CR Discrepancy Assessment
2.6. Measurement Reliability
2.7. Statistical Analysis
3. Results
3.1. Study Population and Methodological Considerations
3.1.1. Participant Characteristics
3.1.2. Reproducibility of Centric Relation Recordings
3.1.3. Structure of the Results and Analytical Framework
3.2. Intergroup Differences
3.2.1. Condylar Bone Change Prevalence
- Osteophyte formation: 22/60 cases (36.7%);
- Erosion: 18/60 cases (30.0%);
- Subcortical sclerosis: 10/60 cases (16.7%);
- Articular surface flattening: 6/60 cases (10.0%);
- Subcortical cysts: 4/60 cases (6.7%).
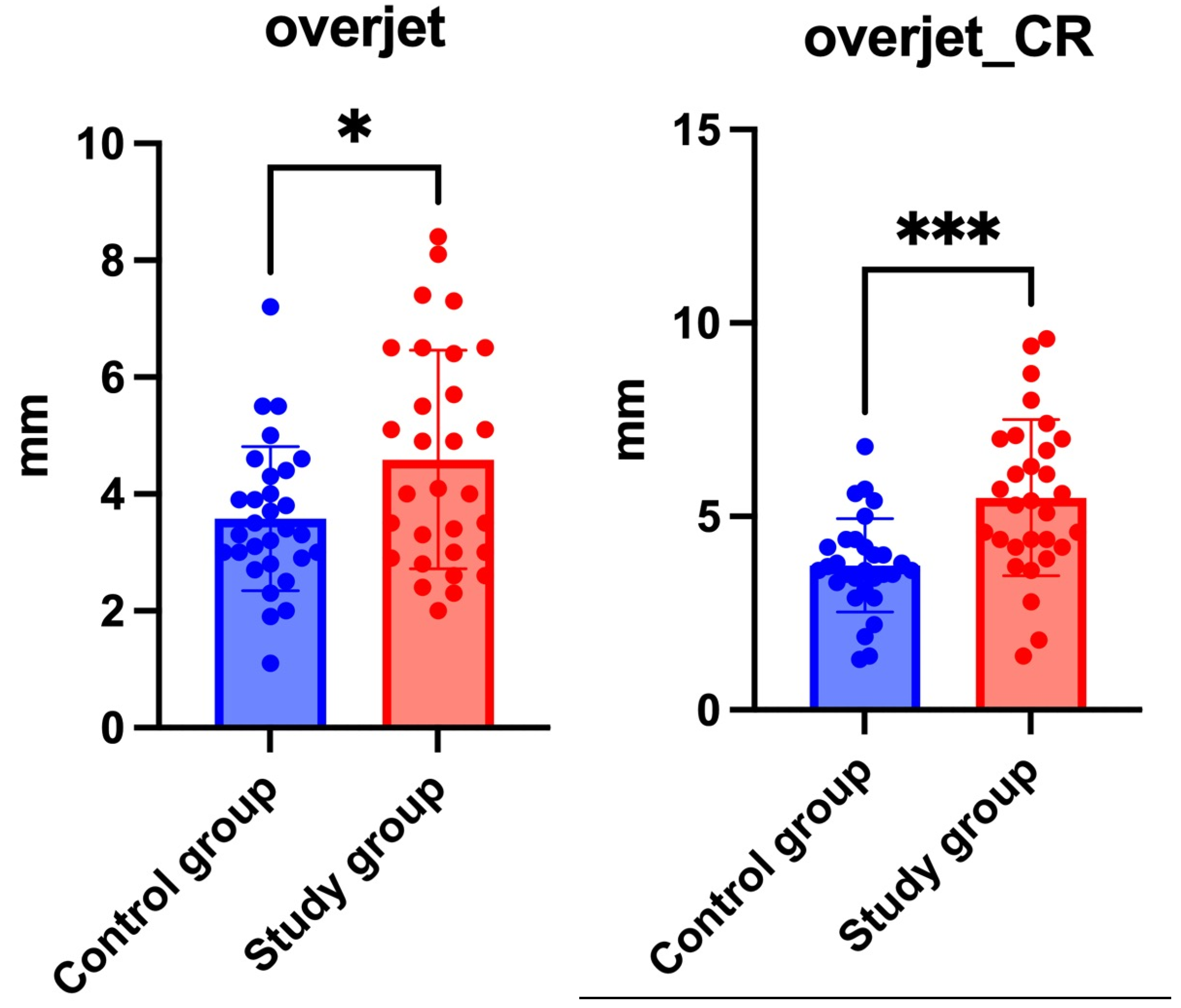
3.2.2. Cephalometric Variables
3.2.3. Joint Space
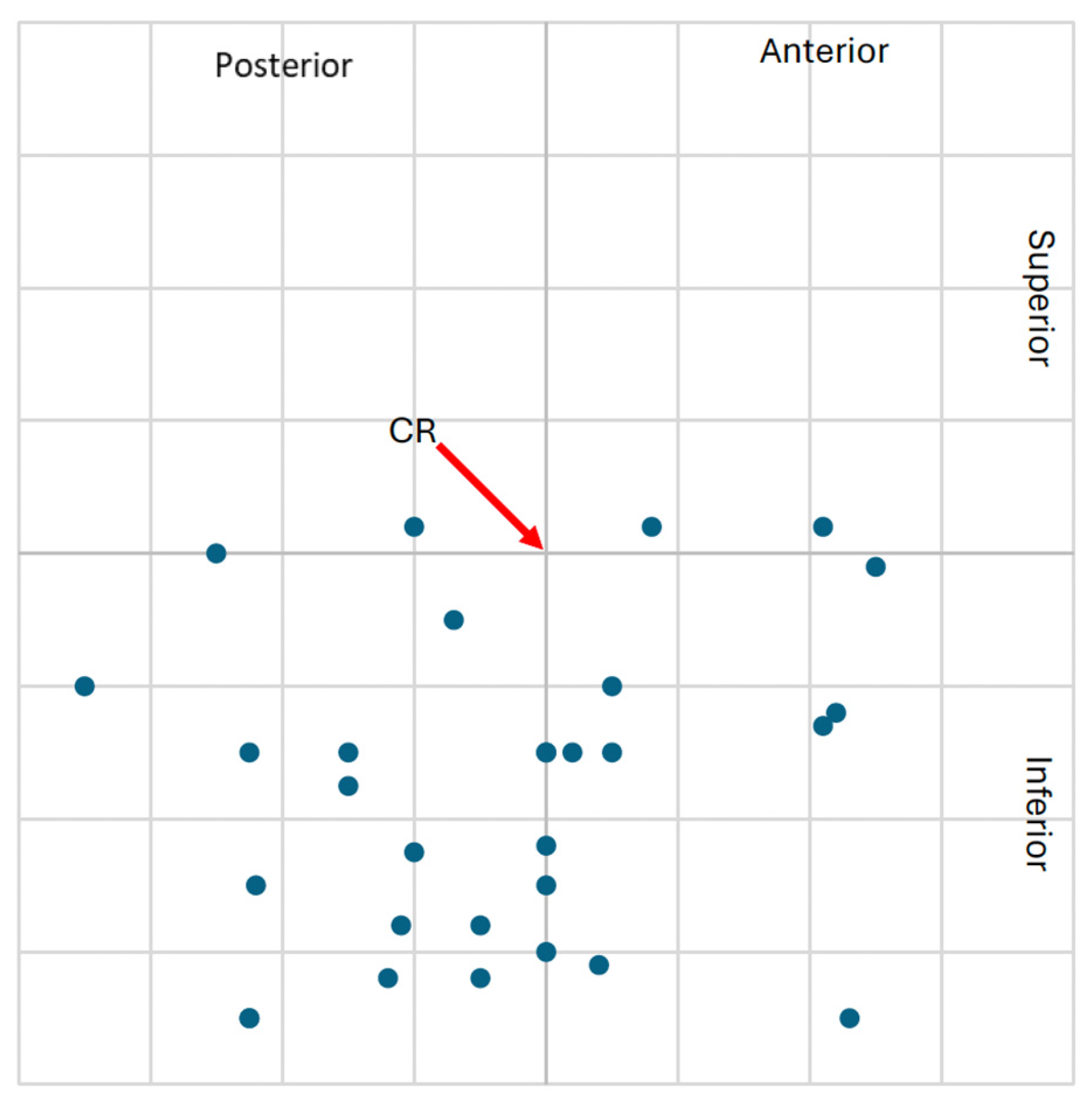
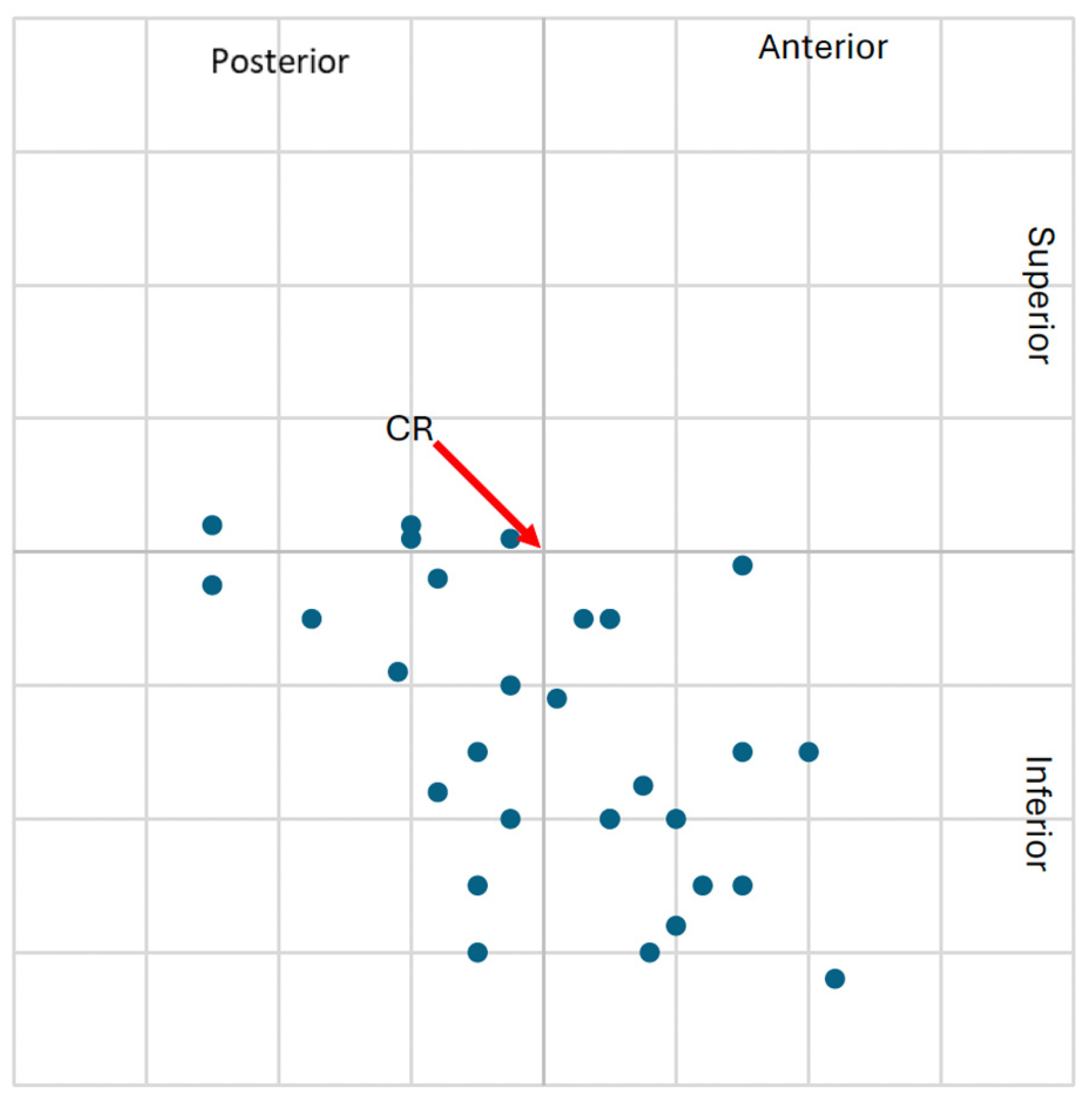
3.2.4. Condylar Displacement
- Study group: 54/120 condyles (45%);
- Control group: 29/120 condyles (24%).
- Study group: 27 condyles (22.5%);
- Control group: 19 condyles (15.8%).
- Study group: 16 patients (26.7%);
- Control group: 9 patients (15.0%).
3.3. Impact of Centric Slider Conversion on Cephalometric Variables
3.3.1. Study Group
3.3.2. Control Group
3.3.3. Study Group with CD ≥ 2 mm
- Significant differences in ANB:
- -
- Left condyle Δx ≥ 2 mm → p = 0.006;
- -
- Right condyle Δ x ≥ 2 mm → p = 0.05.
- Highly significant differences in overjet:
- -
- Both condyles Δ x ≥ 2 mm → p = 0.0002;
- -
- Δz ≥ 2 mm → p = 0.001 (left), p = 0.007 (right).
- Trend for WITS difference (left condyle Δx): p = 0.08.
- Trend in ANS-Gn distance (left condyle Δz): p = 0.08.
3.4. Correlations of Variables
3.4.1. Condylar Displacement and Cephalometric Variables
3.4.2. Joint Space and Cephalometric Variables
4. Discussion
4.1. Methodological Reliability and Centric Relation Reproducibility
4.2. Prevalence and Patterns of Condylar Bone Alterations
4.3. Differences in Cephalometric Variables
4.4. Temporomandibular Joint Space Variation
4.5. Condylar Displacement Due to Centric Slide Between Groups
4.6. Impact of MIP-CR Conversion on Cephalometric Variables
4.6.1. Group Comparison
4.6.2. Study Group with CD ≥ 2
4.7. Correlations of Variables
4.7.1. Condylar Displacement and Cephalometric Variables
4.7.2. Joint Space and Cephalometric Variables
4.8. Strengths and Limitations
4.9. Future Directions
- Incorporate longitudinal designs to evaluate TMJ remodeling over time;
- Investigate the prognostic value of MIP-CR discrepancies in detecting TMJ dysfunction;
- Establish standardized CBCT and CR recording protocols for routine orthodontic screening in high-risk populations.
5. Conclusions
- Adult patients with skeletal class II malocclusion demonstrated a higher prevalence of CBCT-confirmed temporomandibular joint degeneration.
- Greater condylar displacements between CR and MIP were observed in the DJD group, particularly in the anteroposterior (Δx) and vertical (Δz) dimensions.
- Cephalometric differences, including increased ANB, reduced SNB, and higher WITS values, indicated more pronounced sagittal discrepancies in the study group.
- Posterior and superior joint space reductions may reflect condylar remodeling or altered joint loading in the degenerative group.
- These findings suggest that CR-based assessment and condylar position analysis may enhance the understanding of skeletal and joint-related discrepancies in selected adult cases. However, clinical implementation should be approached cautiously and supported by further prospective validation.
- Due to the cross-sectional design and moderate sample size, these observations should be interpreted cautiously. Longitudinal studies are warranted to confirm these associations and determine their diagnostic and prognostic value.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TMJ | temporomandibular joint |
| CBCT | cone beam computed tomography |
| CPI | condylar position index |
| SS | superior joint space |
| AS | anterior joint space |
| PS | posterior joint space |
| DJD | degenerative joint disease |
| AAOP | American Academy of Orofacial Pain |
| CR | centric relation |
| MIP | maximal intercuspation, habitual occlusion |
| CD | condylar displacement |
Appendix A
Appendix A.1. Imaging Studies
Appendix A.2. CO-CR Discrepancy Assessment
References
- Wood, D.P.; Elliott, R.W. Reproducibility of the centric relation bite registration technique. Angle Orthod. 1994, 64, 211–220. [Google Scholar] [PubMed]
- Utt, T.W.; Meyers, C.E., Jr.; Wierzba, T.F.; Hondrum, S.O. A three-dimensional comparison of condylar position changes between centric relation and centric occlusion using the mandibular position indicator. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Hidaka, O.; Adachi, S.; Takada, K. The difference in condylar position between centric relation and centric occlusion in pretreatment Japanese orthodontic patients. Angle Orthod. 2002, 72, 295–301. [Google Scholar]
- Tanaka, E.; Detamore, M.S.; Mercuri, L.G. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef]
- Radej, I.; Szarmach, I. The Role of Maxillofacial Structure on Condylar Displacement in Maximum Intercuspation and Centric Relation. BioMed Res. Int. 2022, 2022, 1439203. [Google Scholar] [CrossRef]
- Barrera-Mora, J.M.; Espinar Escalona, E.; Abalos Labruzzi, C.; Llamas Carrera, J.M.; Ballesteros, E.J.; Solano Reina, E.; Rocabado, M. The relationship between malocclusion, benign joint hypermobility syndrome, condylar position and TMD symptoms. Cranio 2012, 30, 121–130. [Google Scholar] [CrossRef]
- Krisjane, Z.; Urtane, I.; Krumina, G.; Neimane, L.; Ragovska, I. The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: A cone-beam CT study. Int. J. Oral Maxillofac. Surg. 2012, 41, 690–695. [Google Scholar] [CrossRef]
- dos Anjos Pontual, M.L.; Freire, J.S.; Barbosa, J.M.; Frazão, M.A.; dos Anjos Pontual, A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac. Radiol. 2012, 41, 24–29. [Google Scholar] [CrossRef]
- Almăşan, O.C.; Băciuţ, M.; Almăşan, H.A.; Bran, S.; Lascu, L.; Iancu, M.; Băciuţ, G. Skeletal pattern in subjects with temporomandibular joint disorders. Arch. Med. Sci. 2013, 9, 118–126. [Google Scholar] [CrossRef]
- Okeson, J. Management of Temporomandibular Disorder and Occlusion, 7th ed.; Elsevier: St Louis, MO, USA, 2014. [Google Scholar]
- Chen, S.; Lei, J.; Fu, K.Y.; Wang, X.; Yi, B. Cephalometric Analysis of the Facial Skeletal Morphology of Female Patients Exhibiting Skeletal Class II Deformity with and without Temporomandibular Joint Osteoarthrosis. PLoS ONE 2015, 10, e0139743. [Google Scholar] [CrossRef]
- Paknahad, M.; Shahidi, S.; Abbaszade, H. Correlation between condylar position and different sagittal skeletal facial types. J. Orofac. Orthop. 2016, 77, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Shu, C.; Xiong, X.; Huang, L.; Liu, Y. The relation of cephalometric features to internal derangements of the temporomandibular joint: A systematic review and meta-analysis of observational studies. Orthod. Craniofac. Res. 2021, 24, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Pascu, L.; Haiduc, R.-S.; Almășan, O.; Leucuța, D.-C. Occlusion and Temporomandibular Disorders: A Scoping Review. Medicina 2025, 61, 791. [Google Scholar] [CrossRef]
- Zheng, J.; Zhang, Y.; Wu, Q.; Xiao, H.; Li, F. Three-dimensional spatial analysis of the temporomandibular joint in adult patients with Class II division 2 malocclusion before and after orthodontic treatment: A retrospective study. BMC Oral Health 2023, 23, 477. [Google Scholar] [CrossRef]
- Shi, Q.; Gu, Z.; Lai, D.; Dai, Q.; Yu, F. Three-dimensional evaluation of condylar morphology after orthodontic treatment in adult patients with Class II malocclusion by cone-beam computed tomography. BMC Oral Health 2024, 24, 48. [Google Scholar] [CrossRef]
- Ahn, S.J.; Kim, T.W.; Nahm, D.S. Cephalometric keys to internal derangement of temporomandibular joint in women with Class II malocclusions. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 486–494; discussion 494–495. [Google Scholar] [CrossRef]
- Ferreira, R.; Seraidarian, P.; Silveira, G.; Horta, M.; Palomo, J.; Andrade, I., Jr. How a Discrepancy Between Centric Relation and Maximum Intercuspation Alters Cephalometric and Condylar Measurements. Compend. Contin. Educ. Dent. 2020, 41, e1–e6. [Google Scholar]
- Das, K.; Kour, J.; Priya, B.; Mishra, S.; Das, P.; Priya, S.; Gupta, S. Volumetric Comparison of the Temporomandibular Joint Space in Skeletal Class I and II Patients Using Cone-Beam Computed Tomography: A Cross-Sectional Study. Cureus 2024, 16, e75597. [Google Scholar] [CrossRef]
- Estomaguio, G.A.; Yamada, K.; Ochi, K.; Hayashi, T.; Hanada, K. Craniofacial morphology and inclination of the posterior slope of the articular eminence in female patients with and without condylar bone change. Cranio 2005, 23, 257–263. [Google Scholar] [CrossRef]
- Al-Hadad, A.S.; ALyafrusee, E.S.; Abdulqader, A.A.; Al-Gumaei, W.S.; Al-Mohana, R.A.A.M.; Ren, L. Comprehensive three-dimensional positional and morphological assessment of the temporomandibular joint in different vertical skeletal patterns. BMC Oral Health 2022, 22, 149. [Google Scholar] [CrossRef]
- Ahmad, M.; Hollender, L.; Anderson, Q.; Kartha, K.; Ohrbach, R.; Truelove, E.L.; John, M.T.; Schiffman, E.L. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): Development of image analysis criteria and examiner reliability for image analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Kawamura, A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 495–501. [Google Scholar] [CrossRef]
- Power, G.; Breckon, J.; Sherriff, M.; McDonald, F. Dolphin Imaging Software: An analysis of the accuracy of cephalometric digitization and orthognathic prediction. Int. J. Oral Maxillofac. Surg. 2005, 34, 619–626. [Google Scholar] [CrossRef]
- Schmitt, M.E.; Kulbersh, R.; Freeland, T.; Bever, K.; Pink, F.E. Reproducibility of the roth power centric in determining centric relation. Semin. Orthod. 2003, 9, 102–108. [Google Scholar] [CrossRef]
- Dygas, S.; Szarmach, I.; Radej, I. Assessment of the Morphology and Degenerative Changes in the Temporomandibular Joint Using CBCT according to the Orthodontic Approach: A Scoping Review. Biomed Res. Int. 2022, 2022, 6863014. [Google Scholar] [CrossRef]
- Čimić, S.; Kraljević Šimunković, S.; Savić Mlakar, A.; Simonić Kocijan, S.; Tariba, P.; Ćatić, A. Reproducibility of the Obtained Centric Relation Records in Patients with Disc Displacement with Reduction. Acta Stomatol. Croat. 2018, 52, 24–31. [Google Scholar] [CrossRef]
- Oliveira, D.; Fernandes, E.E.; Lopes, S.L.P.C.; Rode, S.M.; Oliveira, W.; Ertty, E.; Cardoso, M.A.; Tien-Li, A.; Meloti, F. Prevalence of condylar morphological changes in individuals with class II malocclusion. Braz. Oral Res. 2024, 38, e060. [Google Scholar] [CrossRef]
- Zhou, L.; Tao, K.; Ma, J.; Pan, X.; Zhang, K.; Feng, J. Relationship between temporomandibular joint space and articular disc displacement. BMC Oral Health 2025, 25, 611. [Google Scholar] [CrossRef]
- Alhammadi, M.S. Dimensional and positional characteristics of the temporomandibular joint of skeletal Class II malocclusion with and without temporomandibular disorders. J. Contemp. Dent. Pr. 2021, 22, 643–648. [Google Scholar]
- Muthuraman, N.R.; Gnaneswar, S.M.; Jasper, A.M.; Bahudeen, M.S. Is Centric Relation and Centric Occlusion Discrepancy an Enigma? An Orthodontic Perspective. J. Clin. Diagn. Res. 2023, 17, ZE01–ZE04. [Google Scholar] [CrossRef]
- Kamatchi, D.; Palanivel, V.; Sivalingam, S.K. Evaluation of correlation between cephalometric variables and internal derangement of temporomandibular joint in asymptomatic class II division I high angle patients using Helical computed tomography. SRM J. Res. Dent. Sci. 2013, 4, 6–11. [Google Scholar] [CrossRef]
- Choi, A.; Park, J.H.; Bay, C.; Chae, J.-M. Evaluation of Condyle–Fossa Relationships in Adults with Various Skeletal Patterns Using Cone-Beam Computed Tomography. Appl. Sci. 2025, 15, 944. [Google Scholar] [CrossRef]
- Mohlin, B.; Axelsson, S.; Paulin, G.; Pietilä, T.; Bondemark, L.; Brattström, V.; Hansen, K.; Holm, A.K. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007, 77, 542–548. [Google Scholar] [CrossRef] [PubMed]





| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Skeletal class II malocclusion (ANB angle values above the 2 ± 2.5° interval) Age 18 years or older TMJ sounds and mild-to-moderate TMJ pain No prior orthodontic treatment | Congenital craniofacial malformations Severe facial asymmetry Deformity secondary to trauma Ankylosis Endocrine–metabolic diseases/severe systematic diseases Autoimmune diseases Rheumatoid/other type of arthritis Unilateral condylar bony changes Acute or severe TMJ pain, masticatory muscle tenderness, or a restricted range of mandibular motion |
| Angular Cephalometric Variables | Description | Linear Cephalometric Variables | Description |
|---|---|---|---|
| SNA SNB ANB PP/MP PP/Go-Gn Ar/Go-Me PP/SN SN/Go-Gn FMA MP/SN occ/SN | sella–nasion–point A sella–nasion–point B difference between SNA and SNB palatal plane/mandibular plane palatal plane/gonion–gnathion articulare/gonion–menton palatal plane/sella–nasion sella–nasion/gonion–gnathion Frankfurt mandibular plane angle mandibular plane/sella–nasion occlusal plane/sella–nasion | WITS ANS-Gn ANS-Me Co-Gn/Co-A overjet overbite | Wits appraisal (points A and B relation on occlusal plane) anterior nasal spine–gnathion (lower face height) anterior nasal spine–menton condylion–gonion/condylion–point A horizontal overlap of the maxillary central incisors over the mandibular central incisors vertical overlap of the maxillary central incisors over the mandibular central incisors |
| Cephalometric Variable | Study Group (Mean ± SD) | Control Group (Mean ± SD) | p-Value |
|---|---|---|---|
| ANB_CR (degrees) | 7.4 ± 2.5 | 5.9 ± 1.1 | 0.055 |
| Overjet (mm) | 4.6 ± 1.9 | 3.6 ± 1.2 | 0.0164 * |
| Overjet_CR (mm) | 5.5 ± 2 | 3.7 ± 1.2 | 0.0001 *** |
| Cephalometric Variable | p-Value (Δx L) | p-Value (Δx R) | p-Value (Δz L) | p-Value (Δz R) |
|---|---|---|---|---|
| ANB_CR | 0.0057 * | 0.048 * | 0.3 | 0.26 |
| WITS_CR | 0.08 | 0.31 | 0.64 | 0.34 |
| ANS-Gn_CR | 0.84 | 0.32 | 0.08 | 0.77 |
| Overjet_CR | 0.0002 *** | 0.0002 *** | 0.0013 * | 0.0068 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dygas, S.; Szarmach, I.; Radej, I.; Chaqués-Asensi, J. Influence of Maxillofacial Morphology on Temporomandibular Joint Degenerative Alterations and Condyle Position Assessed by CBCT in Class II Malocclusion Adult Patients—A Cross-Sectional Study. J. Clin. Med. 2025, 14, 4499. https://doi.org/10.3390/jcm14134499
Dygas S, Szarmach I, Radej I, Chaqués-Asensi J. Influence of Maxillofacial Morphology on Temporomandibular Joint Degenerative Alterations and Condyle Position Assessed by CBCT in Class II Malocclusion Adult Patients—A Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(13):4499. https://doi.org/10.3390/jcm14134499
Chicago/Turabian StyleDygas, Sebastian, Izabela Szarmach, Ilona Radej, and José Chaqués-Asensi. 2025. "Influence of Maxillofacial Morphology on Temporomandibular Joint Degenerative Alterations and Condyle Position Assessed by CBCT in Class II Malocclusion Adult Patients—A Cross-Sectional Study" Journal of Clinical Medicine 14, no. 13: 4499. https://doi.org/10.3390/jcm14134499
APA StyleDygas, S., Szarmach, I., Radej, I., & Chaqués-Asensi, J. (2025). Influence of Maxillofacial Morphology on Temporomandibular Joint Degenerative Alterations and Condyle Position Assessed by CBCT in Class II Malocclusion Adult Patients—A Cross-Sectional Study. Journal of Clinical Medicine, 14(13), 4499. https://doi.org/10.3390/jcm14134499






