The First Biological Respect Protocol: A Biodigital Technique for Definitive Customized One-Time Abutments—A Case Report
Abstract
1. Introduction
2. Case Presentation
2.1. Clinical Procedures
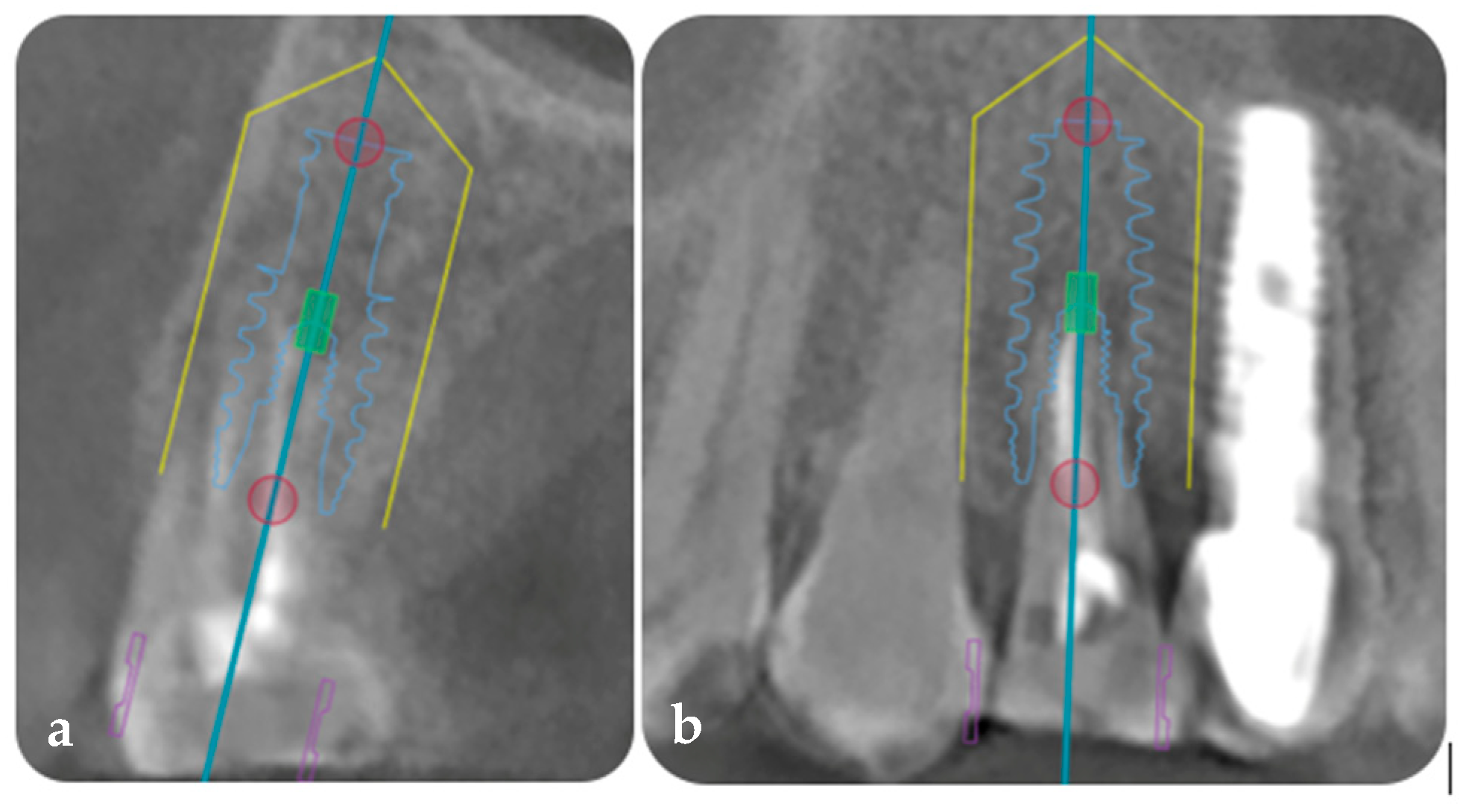
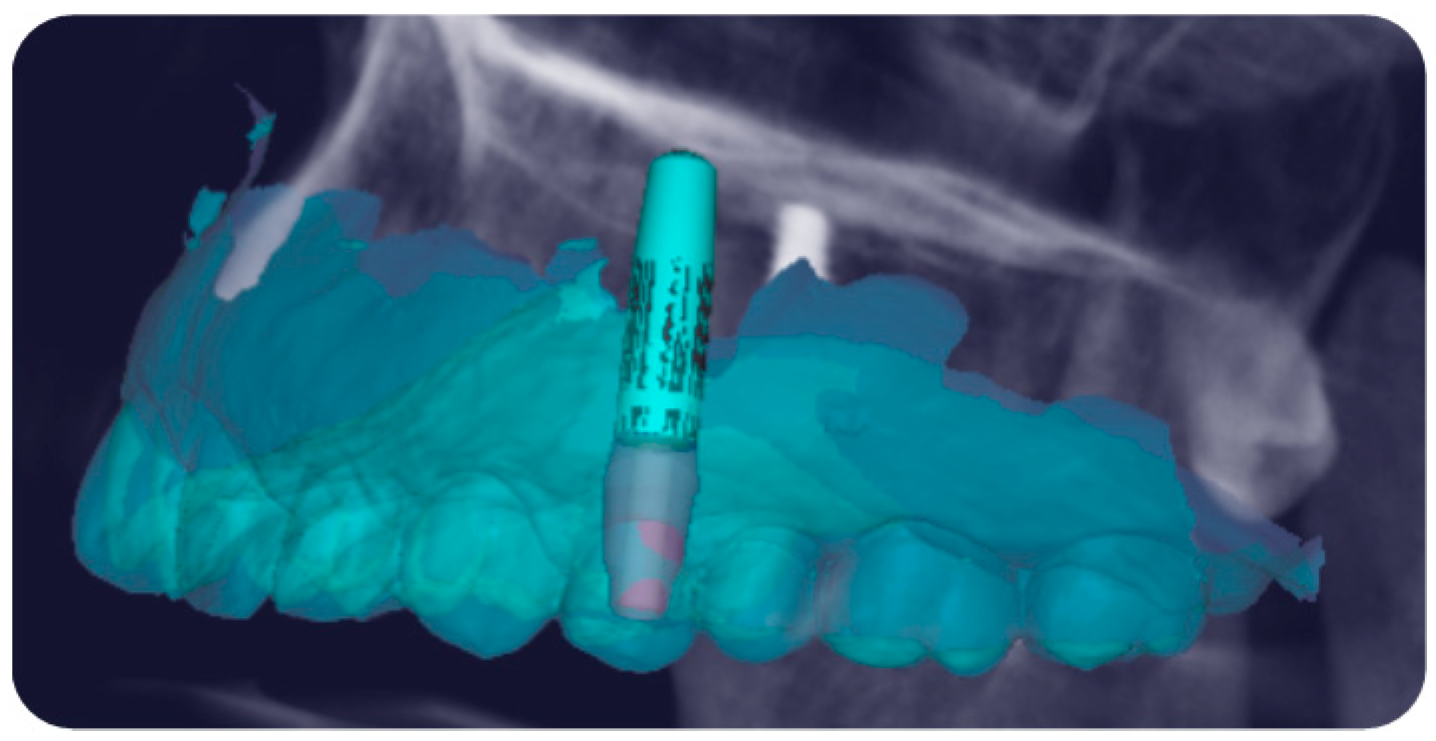
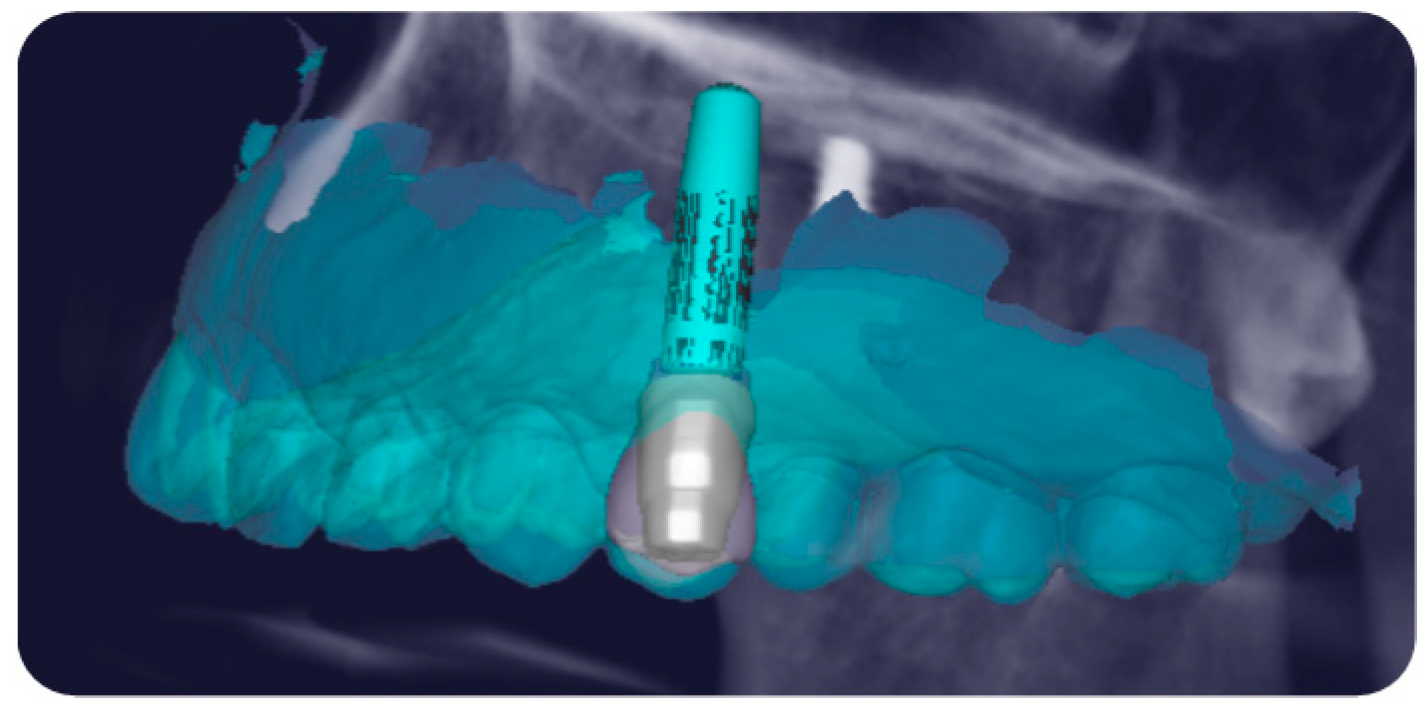
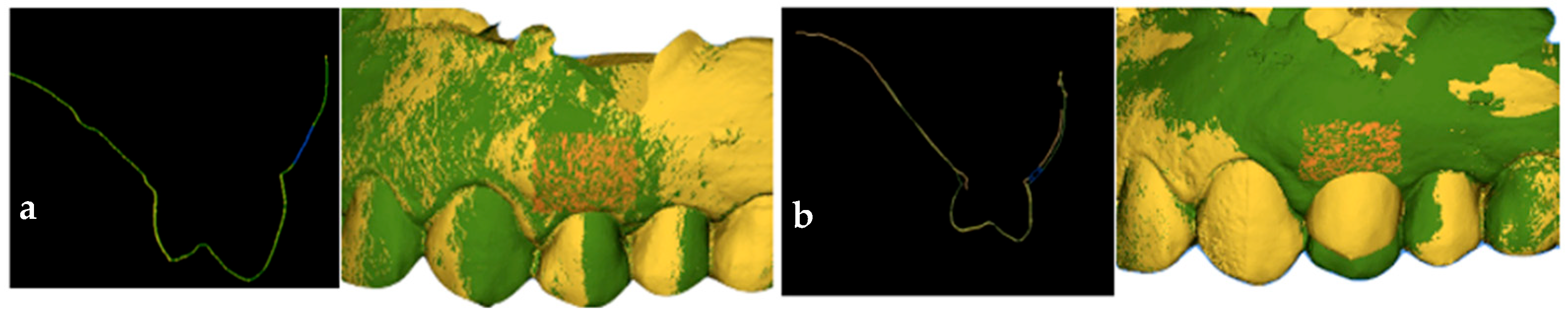
2.1.1. Phase 1: Digital Planning of the Implant, Customized Definitive Abutment, Coping, Provisional, and Definitive Framework
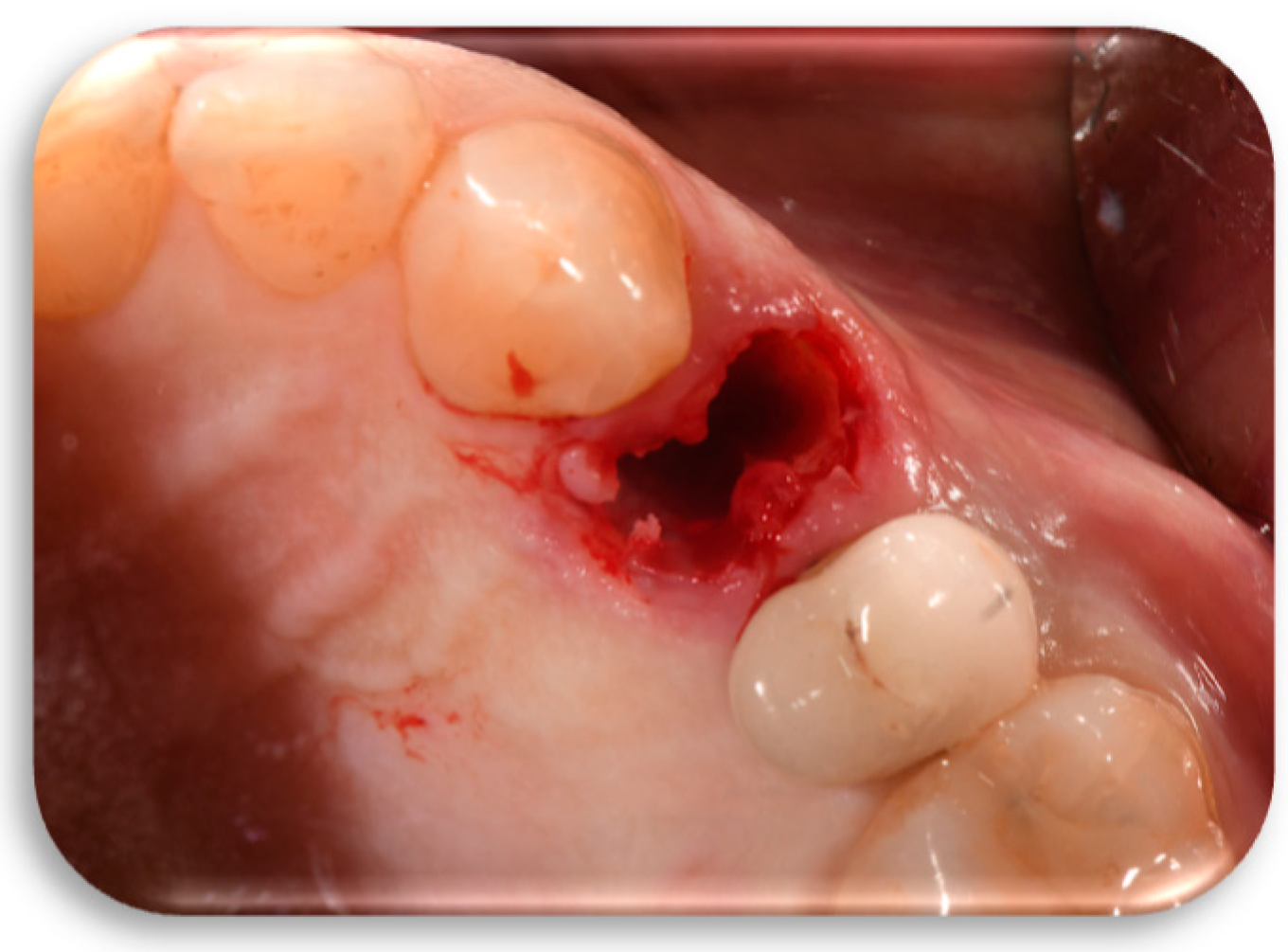
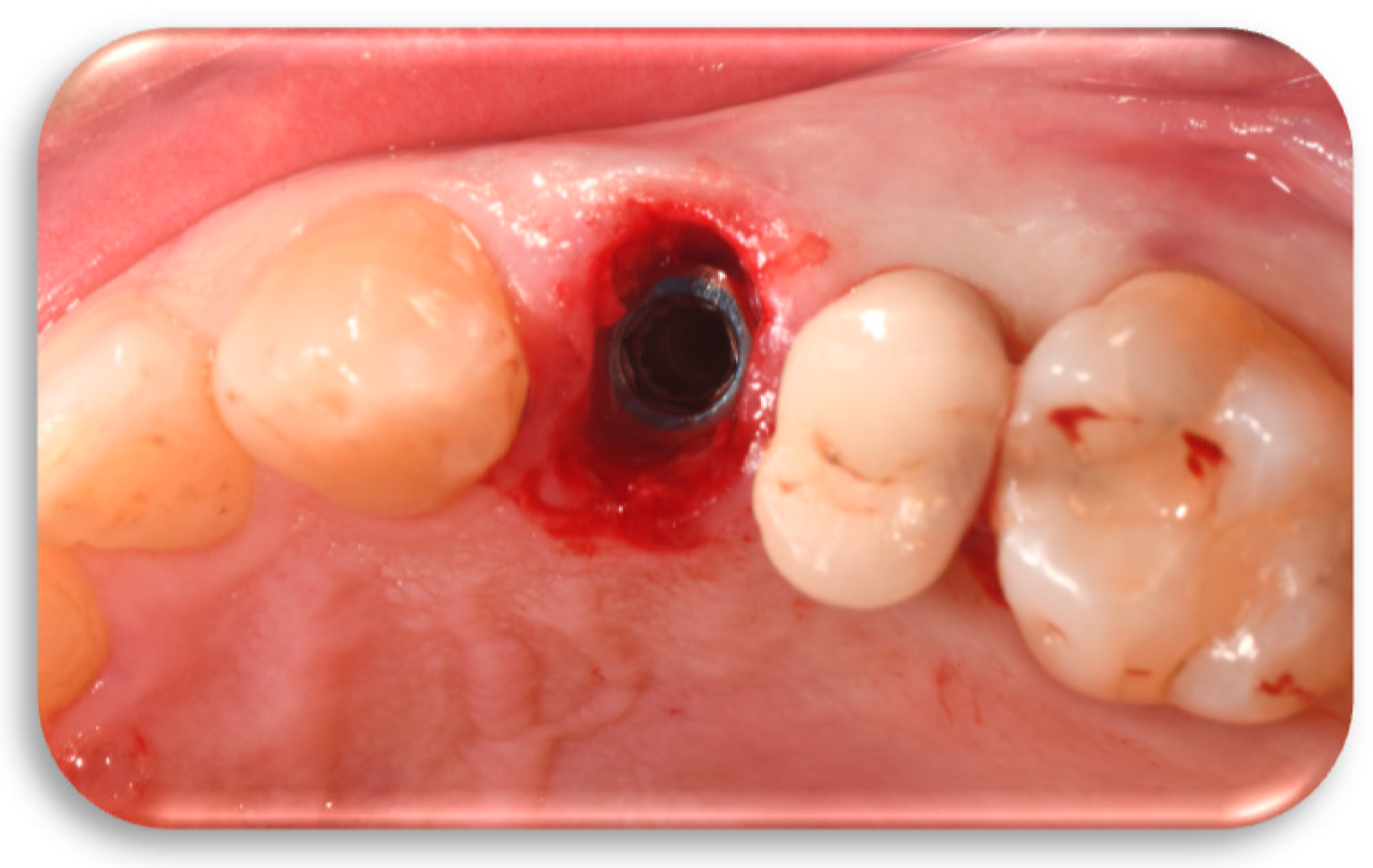
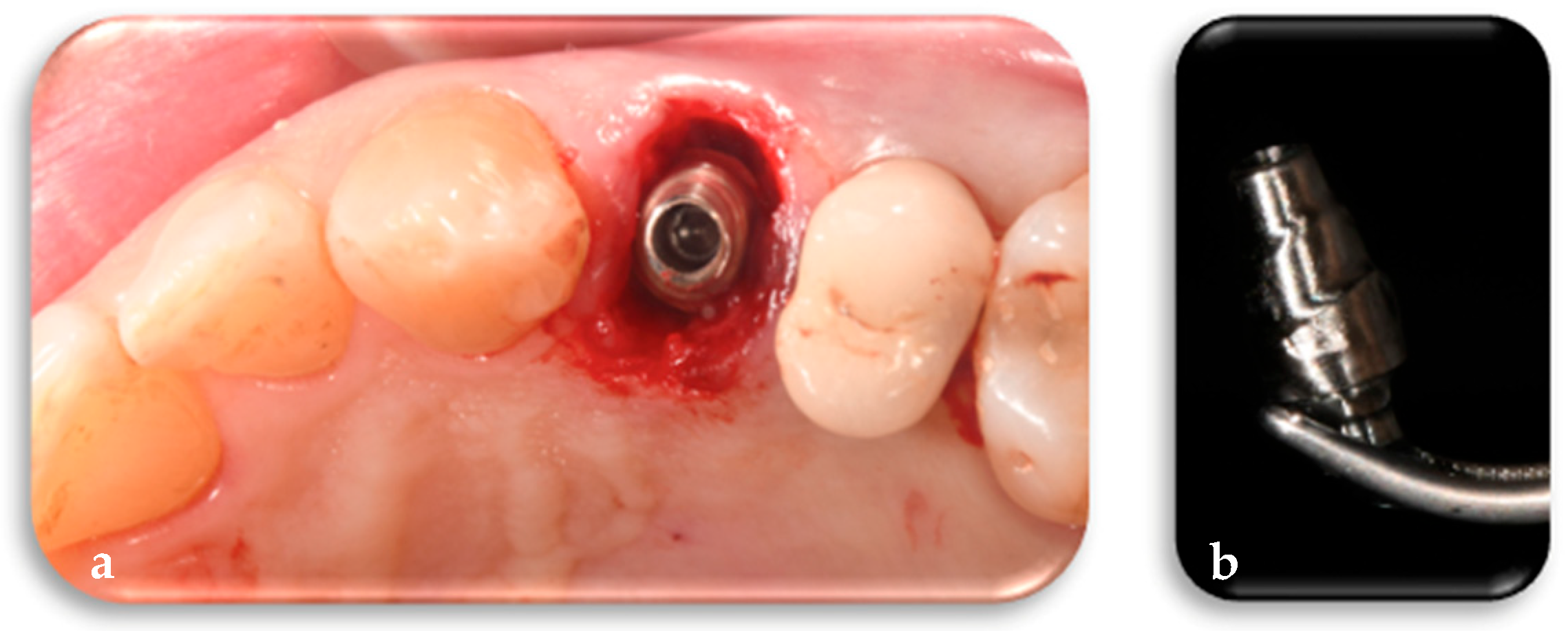
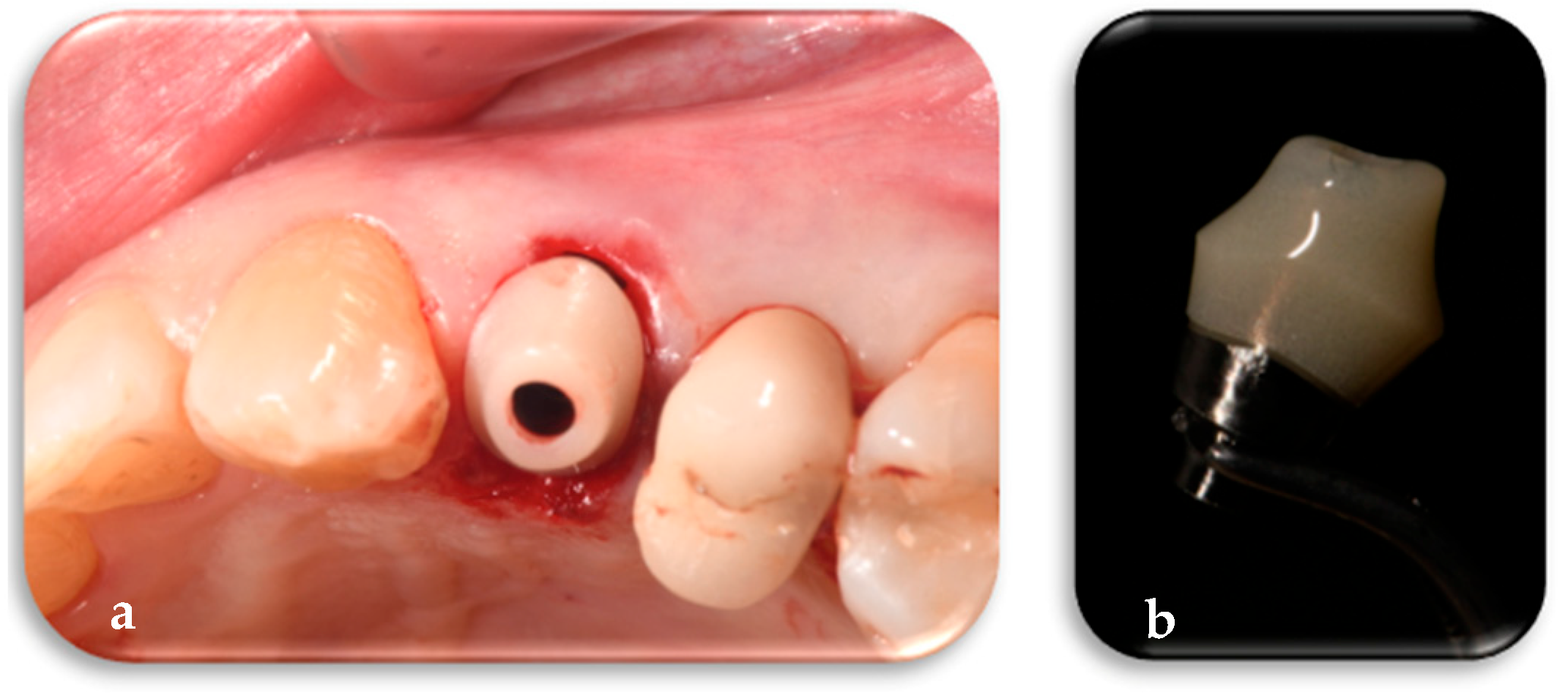
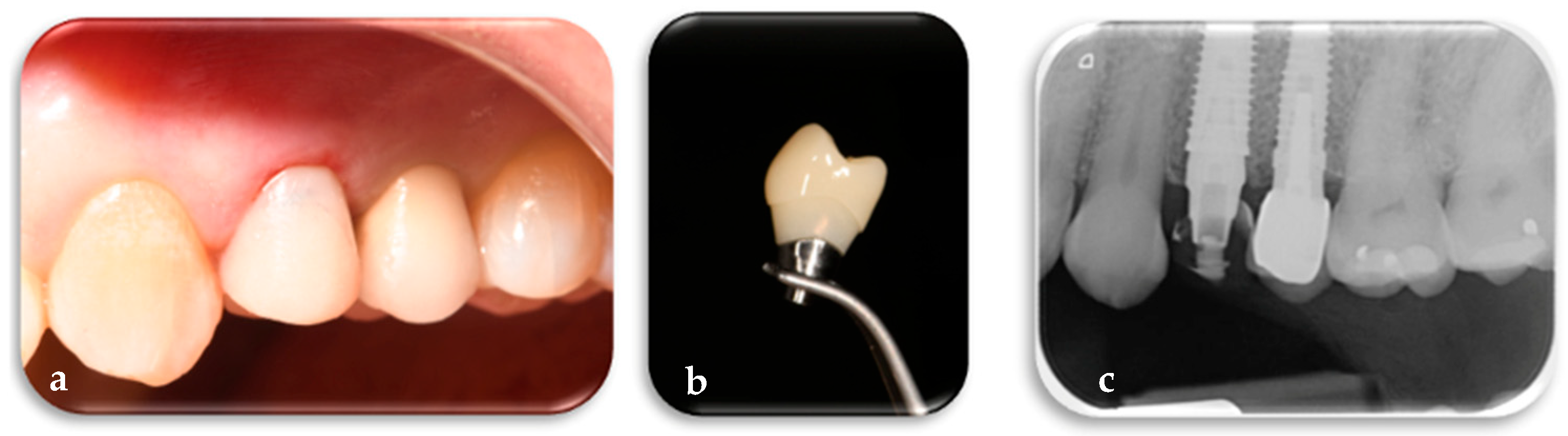
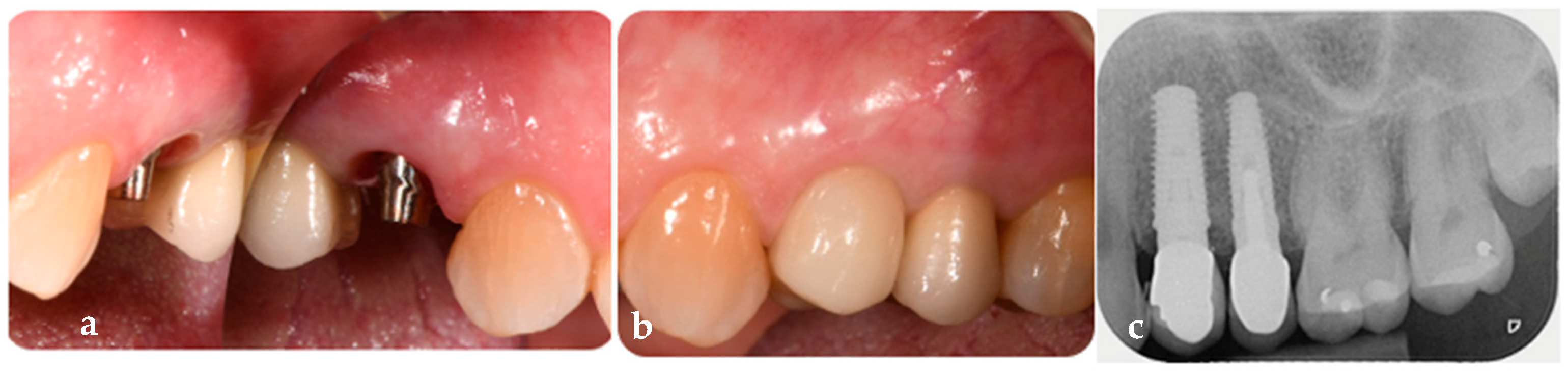
2.1.2. Phase 2: Implant Placement, Delivery of the Definitive Customized Abutment, Coping, Provisional Restoration, and Fitting of the Definitive Framework
2.1.3. Phase 3: Finalization of Aesthetics on the Definitive Framework and Follow-Up
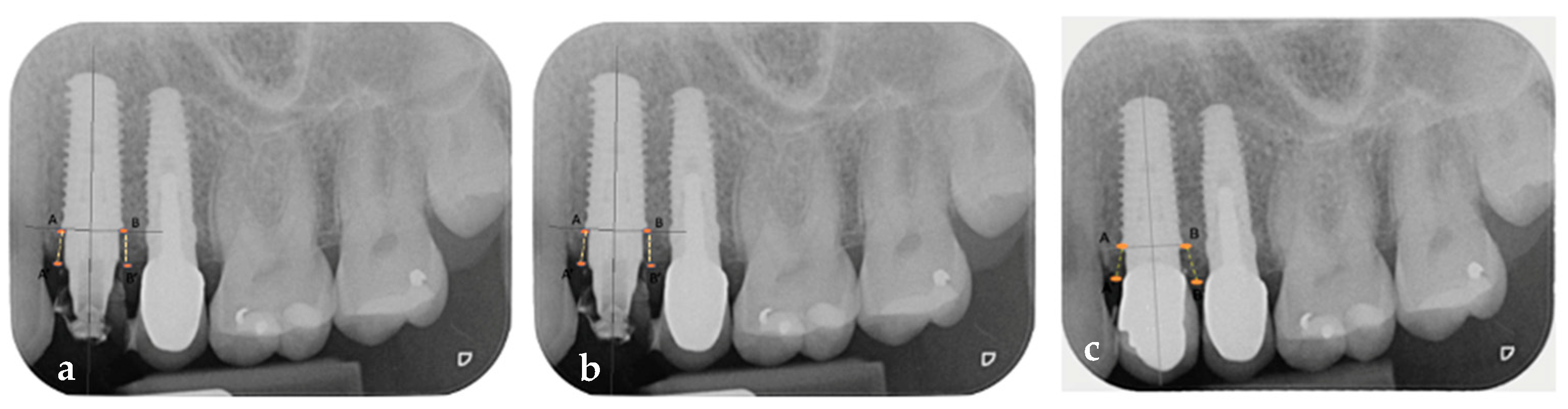
2.2. Measurements
3. Discussion and Limitations
- Absence of mobility of the prosthesis, abutment, and implant at both 6-month and 1-year follow-up.
- Presence of keratinized peri-implant on the mid-buccal and mid-lingual aspects at 6-month and 1-year follow-up.
- Sulcus Bleeding Index (SBI) score of 0 at both 6-month and 1-year follow-up.
- Modified Plaque Index (mPLI) score of 0 at both 6-month and 1-year follow-up.
- Probing Depth (PD) < 4 mm at both 6-month and 1-year follow-up.
- Keratinized mucosa width (KMW) values of 4 mm before surgery, 4 mm at 6 months, and 5 mm at 1 year after implant, customized abutment, coping, and restoration placement.
- Differs from the “one abutment, one time” protocol because FR abutments are not round-shaped but definitive and customized, specifically designed according to the tooth to be replaced and the arch in which it is located.
- Differs from customized healing abutments fabricated using indirect techniques, which are not exempt from disconnections and reconnections, as FR abutments are definitive and digitally customized based on the digital mathematics of the tooth to be replaced and the corresponding arch.
- Allows for digital planning not only of the implant placement but also of the customized prosthetic components—definitive abutment, coping, provisional restoration, and final prosthetic structure—thereby reducing working time, waiting time, the number of disconnections, components, and intermediate impressions.
4. Clinical Relevance
5. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Chen, S.T.; Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int. J. Oral Maxillofac. Implant. 2009, 24, 186–217. [Google Scholar]
- Zupnik, J.; Kim, S.; Ravens, D.; Karimbux, N.; Guze, K. Factors associated with dental implant survival: A 4-year retrospective analysis. J. Periodontol. 2011, 82, 1390–1395. [Google Scholar] [CrossRef] [PubMed]
- Brugnami, F.; Caleffi, C. Prosthetically driven implant placement. How to achieve the appropriate implant site development. Keio J. Med. 2005, 54, 172–178. [Google Scholar] [CrossRef]
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontology 2000 2017, 73, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Smitkarn, P.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery. J. Clin. Periodontol. 2019, 46, 949–957. [Google Scholar] [CrossRef]
- Kalaivani, G.; Balaji, V.R.; Manikandan, D.; Rohini, G. Expectation and reality of guided implant surgery protocol using computer-assisted static and dynamic navigation system at present scenario: Evidence-based literature review. J. Indian Soc. Periodontol. 2020, 24, 398–408. [Google Scholar] [CrossRef]
- Panchal, N.; Mahmood, L.; Retana, A.; Emery, R., 3rd. Dynamic navigation for dental implant surgery. Oral Maxillofac. Surg. Clin. North Am. 2019, 31, 539–547. [Google Scholar] [CrossRef]
- Abrahamsson, I.; Berglundh, T.; Lindhe, J. The mucosal barrier following abutment dis/reconnection: An experimental study in dogs. J. Clin. Periodontol. 1997, 24, 568–572. [Google Scholar] [CrossRef]
- Berglundh, T.; Lindhe, J. Dimension of the periimplant mucosa: Biological width revisited. J. Clin. Periodontol. 1996, 23, 971–973. [Google Scholar] [CrossRef]
- Moon, I.S.; Berglundh, T.; Abrahamsson, I.; Linder, E.; Lindhe, J. The barrier between the keratinized mucosa and the dental implant: An experimental study in the dog. J. Clin. Periodontol. 1999, 26, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Grandi, T.; Guazzi, P.; Samarani, R.; Maghaireh, H.; Grandi, G. One abutment-one time versus a provisional abutment in immediately loaded post-extractive single implants: A 1-year follow-up of a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2014, 7, 141–149. [Google Scholar]
- Canullo, L.; Bignozzi, I.; Cocchetto, R.; Cristalli, M.P.; Iannello, G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow-up of a randomised multicentre clinical trial. Eur. J. Oral Implantol. 2010, 3, 285–296. [Google Scholar] [PubMed]
- Degidi, M.; Nardi, D.; Piattelli, A. One abutment at one time: Non-removal of an immediate abutment and its effect on bone healing around subcrestal tapered implants. Clin. Oral Implant. Res. 2011, 22, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Tawse-Smith, A.; Alsabeeha, N.H.; Ma, S.; Duncan, W.J. The one abutment-one time protocol: A systematic review and meta-analysis. J. Periodontol. 2017, 88, 1173–1185. [Google Scholar] [CrossRef]
- Tallarico, M.; Caneva, M.; Meloni, S.M.; Xhanari, E.; Covani, U.; Canullo, L. Definitive abutments placed at implant insertion and never removed: Is it an effective approach? A systematic review and meta-analysis of randomized controlled trials. J. Oral Maxillofac. Surg. 2018, 76, 316–324. [Google Scholar] [CrossRef]
- Canullo, L.; Omori, Y.; Amari, Y.; Iannello, G.; Pesce, P. Five-year cohort prospective study on single implants in the esthetic area restored using one-abutment/one-time prosthetic approach. Clin. Implant. Dent. Relat. Res. 2018, 20, 668–673. [Google Scholar] [CrossRef]
- Lambrechts, T.; Doornewaard, R.; De Bruyckere, T.; Matthijs, L.; Deschepper, E.; Cosyn, J. A multicenter cohort study on the association of the one-abutment one-time concept with marginal bone loss around bone level implants. Clin. Oral. Impl Res. 2021, 32, 192–202. [Google Scholar] [CrossRef]
- Micarelli, C.; Canullo, L.; Iannello, G. Implant-abutment connection deformation after prosthetic procedures: An in vitro study. Int. J. Prosthodont. 2019, 28, 282. [Google Scholar] [CrossRef]
- Hämmerle, C.H.; Chen, S.T.; Wilson, T.G., Jr. Consensus statements recommended clinical procedures regarding the placement of implants in extraction sockets. Int. J. Oral Maxillofac. Implant. 2004, 19, 26–28. [Google Scholar][Green Version]
- Pitman, J.; Seyssens, L.; Christiaens, V.; Cosyn, J. Immediate implant placement with or without immediate provisionalization: A systematic review and meta-analysis. J. Clin. Periodontol. 2022, 49, 1012–1023. [Google Scholar] [CrossRef] [PubMed]
- Zipprich, H.; Miatke, S.; Hmaidouch, R.; Lauer, H.-C. A new experimental design for bacterial microleakage investigation at the implant-abutment interface: An in vitro study. Int. J. Oral Maxillofac. Implant. 2016, 31, 37–44. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Gianluca, S.; Piattelli, A. The Conometric Concept: A 5-Year follow-up of fixed partial monolithic zirconia restorations supported by cone-in-cone abutments. Int. J. Periodontics Restor. Dent 2018, 38, 363–371. [Google Scholar] [CrossRef]
- Koutouzis, T. Implant-abutment connection as contributing factor to peri-implant diseases. Periodontology 2000 2019, 81, 152–166. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, P.; Burg, S.; Peters, U.; Beikler, T.; Fischer, C.; Rupp, F.; Schweizer, E.; Weigl, P.; Sader, R.; Smeets, R.; et al. Bacterial translocation and microgap formation at a novel conical indexed implant abutment system for single crowns. Clin. Oral Investig. 2022, 26, 1375–1389. [Google Scholar] [CrossRef] [PubMed]
- Calatrava, J.; Sanz-Sánchez, I.; Molina, A.; Bollain, J.; Martín, C.; Sanz, M. Effect of one-time placement of the definitive abutment versus multiple healing abutment disconnections and reconnections during the prosthetic phase on radiographic and clinical outcomes: A 12-month randomized clinical trial. Clin. Implant. Dent Relat. Res. 2024, 26, 998–1011. [Google Scholar] [CrossRef]
- Fernandes, D.; Nunes, S.; López-Castro, G.; Marques, T.; Montero, J.; Borges, T. Effect of customized healing abutments on the peri-implant linear and volumetric tissue changes at maxillary immediate implant sites: A 1-year prospective randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 745–757. [Google Scholar] [CrossRef]
- Molina, A.; Sanz-Sánchez, I.; Martín, C.; Blanco, J.; Sanz, M. The effect of one-time abutment placement on interproximal bone levels and peri- implant soft tissues: A prospective randomized clinical trial. Clin. Oral Implant. Res. 2017, 28, 443–452. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Daprile, G.; Piattelli, A. Nonremoval of immediate abutments in cases involving subcrestally placed postextractive tapered single implants: A randomized controlled clinical study. Clin. Implant. Dent. Relat. Res. 2014, 16, 794–805. [Google Scholar] [CrossRef]
- Kou, Y.; Li, Q.; Tang, Z. Prosthetic emergence angle in different implant sites and their correlation with marginal bone loss: A retrospective study. J. Dent Sci. 2022, 18, 534–540. [Google Scholar] [CrossRef]
- Guglielmi, D.; Di Domenico, G.L.; Aroca, S.; Vignoletti, F.; Ciaravino, V.; Donghia, R.; de Sanctis, M. Soft and hard tissue changes after immediate implant placement with or without a sub-epithelial connective tissue graft: Results from a 6-month pilot randomized controlled clinical trial. J. Clin. Periodontol. 2022, 49, 999–1011. [Google Scholar] [CrossRef] [PubMed]
- Koutouzis, T.; Gholami, F.; Reynolds, J.; Lundgren, T.; Kotsakis, G. Abutment disconnection/reconnection affects peri-implant marginal bone levels: A meta-analysis. Int. J. Oral Maxillofac. Implant. 2017, 32, 575–581. [Google Scholar] [CrossRef]
- Parpaiola, A.; Sbricoli, L.; Guazzo, R.; Bressan, E.; Lops, D. Managing the peri-implant mucosa: A clinically reliable method for optimizing soft tissue contours and emergence profile. J. Esthet. Restor. Dent. 2013, 25, 317–323. [Google Scholar] [CrossRef] [PubMed]
- González-Martín, O.; Lee, E.; Weisgold, A.; Veltri, M.; Su, H. Contour management of implant restorations for optimal emergence profiles: Guidelines for immediate and delayed provisional restorations. Int. J. Periodontics Restor. Dent. 2020, 40, 61–70. [Google Scholar] [CrossRef]
- Corrado, F.; Marconcini, S.; Cosola, S.; Giammarinaro, E.; Covani, U. Immediate implant and customized healing abutment promotes tissues regeneration: A 5-year clinical report. J. Oral Implantol. 2023, 49, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Lertwongpaisan, T.; Amornsettachai, P.; Panyayong, W.; Suphangul, S. Soft tissue dimensional change using customized titanium healing abutment in immediate implant placement in posterior teeth. BMC Oral Health 2023, 23, 384. [Google Scholar] [CrossRef]
- Atieh, M.A.; Ibrahim, H.M.; Atieh, A.H. Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis. J. Periodontol. 2010, 81, 1350–1366. [Google Scholar] [CrossRef]
- Beuer, F.; Groesser, J.; Schweiger, J.; Hey, J.; Güth, J.F.; Stimmelmayr, M. The digital one-abutment/one-time concept. A clinical report. J. Prosthodont. 2015, 24, 580–585. [Google Scholar] [CrossRef]
- Souza, A.B.; Alshihri, A.; Kämmerer, P.W.; Araújo, M.G.; Gallucci, G.O. Histological and micro-CT analysis of peri-implant soft and hard tissue healing on implants with different healing abutments configurations. Clin. Oral Implant. Res. 2018, 29, 1007–1015. [Google Scholar] [CrossRef]
- Mihali, S.G.; Wang, H.-L.; Karancsi, O.; Bratu, E.A. Internal Hexagon vs Conical Implant-Abutment Connections: Evaluation of 3-Year Postloading Outcomes. J. Oral Implantol. 2021, 47, 485–490. [Google Scholar] [CrossRef]
- Scarano, A.; Mortellaro, C.; Mavriqi, L.; Pecci, R.; Valbonetti, L. Evaluation of microgap with three-dimensional X-ray microtomography: Internal hexagon versus cone morse. J. Craniofac. Surg. 2016, 27, 682–685. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Maghaireh, H.; Pistilli, R.; Grusovin, M.G.; Lee, S.T.; Trullenque-Eriksson, A.; Gualini, F. Dental implants with internal versus external connections: 5-year post-loading results from a pragmatic multicenter randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Coppedê, A.R.; Bersani, E.; de Mattos, M.D.G.C.; Rodrigues, R.C.S.; de Mattias Sartori, I.A.; Ribeiro, R.F. Fracture resistance of the implant-abutment connection in implants with internal hex and internal conical connections under oblique compressive loading: An in vitro study. Int. J. Prosthodont. 2009, 22, 283–286. [Google Scholar] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rizzuto, F.; Rizzuto, S. The First Biological Respect Protocol: A Biodigital Technique for Definitive Customized One-Time Abutments—A Case Report. J. Clin. Med. 2025, 14, 4448. https://doi.org/10.3390/jcm14134448
Rizzuto F, Rizzuto S. The First Biological Respect Protocol: A Biodigital Technique for Definitive Customized One-Time Abutments—A Case Report. Journal of Clinical Medicine. 2025; 14(13):4448. https://doi.org/10.3390/jcm14134448
Chicago/Turabian StyleRizzuto, Franco, and Silvia Rizzuto. 2025. "The First Biological Respect Protocol: A Biodigital Technique for Definitive Customized One-Time Abutments—A Case Report" Journal of Clinical Medicine 14, no. 13: 4448. https://doi.org/10.3390/jcm14134448
APA StyleRizzuto, F., & Rizzuto, S. (2025). The First Biological Respect Protocol: A Biodigital Technique for Definitive Customized One-Time Abutments—A Case Report. Journal of Clinical Medicine, 14(13), 4448. https://doi.org/10.3390/jcm14134448





