Biomechanical Analysis of Micromotion of Proximal Interphalangeal Joint Arthrodeses During Activities of Daily Life In Vitro
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PIJ | Proximal interphalangeal joint |
| ADLd | Activities of daily living |
| IFS | Interfragmentary strain |
| DIJ | Distal interphalangeal joint |
Appendix A
| Technique | Extension | Flexion |
|---|---|---|
| Cerclage | angle = −1.4753 + 1.2478 × √force | angle = −0.0918 + 1.1450 × √force |
| Compression wire | angle = −1.4251 + 1.1484 × √force | angle = −3.7193 + 3.4213 × log(force) |
| Fixation plate | angle = −1.2935 + 0.3699 × force2 | angle = −0.9852 + 2.077 × log(force) |
| Herbert screw | angle = −1.3818 + 1.1291 × √force | angle = −2.8308 + 1.8937 × √force |
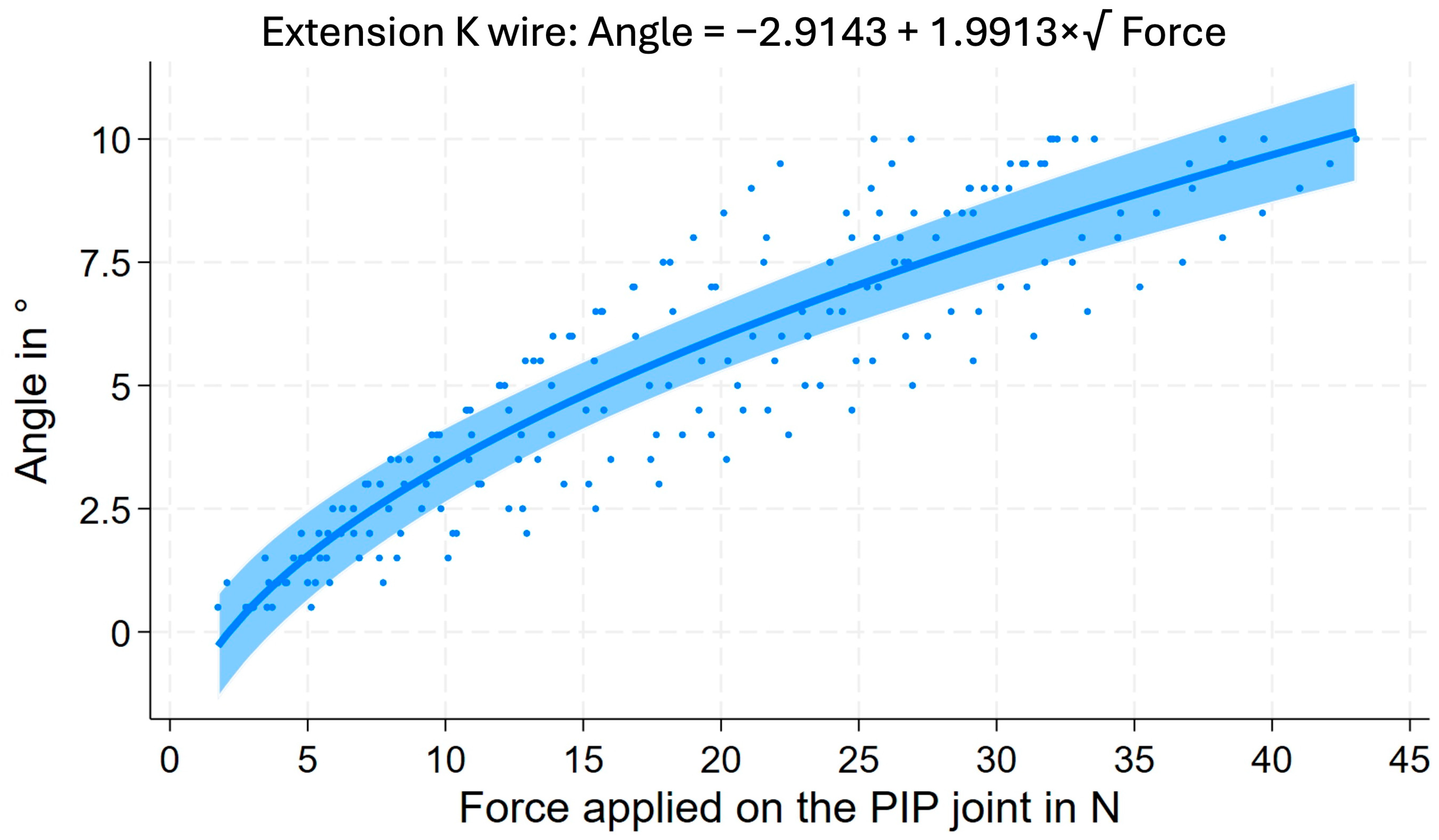
| K-Wire | angle = −2.9143 + 1.9913 × √force | angle = −4.2867 + 3.9663 × log(force) |
| Locking plate | angle = 0.6116 + 0.0426 × force2 | angle = −3.2307 + 2.5416 × log(force) |
| Tension band | angle = −3.5851 + 2.1517 × √force | angle = −2.5469 + 2.9747 × log(force) |
References
- Jacobs, B.J.; Verbruggen, G.; Kaufmann, R.A. Proximal interphalangeal joint arthritis. J. Hand Surg. Am. 2010, 35, 2107–2116. [Google Scholar] [CrossRef] [PubMed]
- Dahaghin, S.; Bierma-Zeinstra, S.M.; Ginai, A.Z.; Pols, H.A.; Hazes, J.M.; Koes, B.W. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann. Rheum. Dis. 2005, 64, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Millrose, M.; Gesslein, M.; Ittermann, T.; Kim, S.; Vonderlind, H.C.; Ruettermann, M. Arthrodesis of the proximal interphalangeal joint of the finger—A systematic review. EFORT Open Rev. 2022, 7, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Roll, S.C.; Hardison, M.E. Effectiveness of Occupational Therapy Interventions for Adults with Musculoskeletal Conditions of the Forearm, Wrist, and Hand: A Systematic Review. Am. J. Occup. Ther. 2017, 71, 7101180010p1–7101180010p12. [Google Scholar] [CrossRef]
- Butz, K.D.; Merrell, G.; Nauman, E.A. A biomechanical analysis of finger joint forces and stresses developed during common daily activities. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 131–140. [Google Scholar] [CrossRef]
- Arauz, P.; DeChello, K.; Dagum, A.; Sisto, S.A.; Kao, I. Biomechanics and Pinch Force of the Index Finger Under Simulated Proximal Interphalangeal Arthrodesis. J. Hand Surg. Am. 2017, 42, 658.e1–658.e7. [Google Scholar] [CrossRef]
- Vonderlind, H.C.; Zach, A.; Eichenauer, F.; Kim, S.; Eisenschenk, A.; Millrose, M. Proximal interphalangeal joint arthrodesis using a compression wire: A comparative biomechanical study. Hand Surg. Rehabil. 2019, 38, 307–311. [Google Scholar] [CrossRef]
- Gueorguiev-Ruegg, B.; Stoddart, M. Biology and biomechanics in bone healing. In AO Principles of Fracture Management, 3rd ed.; Buckley, R.E., Moran, C.G., Eds.; George Thieme Verlag Publisher: Stuttgart, Germany, 2017; Volume 1, pp. 9–27. [Google Scholar]
- Claes, L.; Eckert-Hübner, K.; Augat, P. The fracture gap size influences the local vascularization and tissue differentiation in callus healing. Langenbecks Arch. Surg. 2003, 388, 316–322. [Google Scholar] [CrossRef]
- Claes, L.; Augat, P.; Suger, G.; Wilke, H.J. Influence of size and stability of the osteotomy gap on the success of fracture healing. J. Orthop. Res. 1997, 15, 577–584. [Google Scholar] [CrossRef]
- Millrose, M.; Vonderlind, H.C.; Thannheimer, A.; Ittermann, T.; Rüther, J.; Willauschus, M.; Bail, H.J.; Eisenschenk, A. Arthrodesis of the Proximal Interphalangeal Joint of the Finger-A Biomechanical Study of Primary Stability. J. Pers. Med. 2023, 13, 465. [Google Scholar] [CrossRef]
- Murray, P.M. Treatment of the osteoarthritic hand and thumb. In Green’s Operative Hand Surgery, 7th ed.; Wolfe, S.W., Hotchkiss, R.N., Pederson, W.C., Kozin, S.H., Cohen, M.S., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2017; pp. 345–372. [Google Scholar]
- Lister, G. Intraosseous wiring of the digital skeleton. J. Hand Surg. Am. 1978, 3, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Hohendorff, B.; Franke, J.; Spies, C.K.; Mueller, L.P.; Ries, C. Arthrodesis of the proximal interphalangeal joint of fingers with tension band wire. Oper. Orthop. Traumatol. 2017, 29, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.O.; Ittermann, T.; Schulz, A.; Grabe, H.J.; Baumeister, S.E. Linear, nonlinear or categorical: How to treat complex associations in regression analyses? Polynomial transformations and fractional polynomials. Int. J. Public Health 2013, 58, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Leibovic, S.J.; Strickland, J.W. Arthrodesis of the proximal interphalangeal joint of the finger: Comparison of the use of the Herbert screw with other fixation methods. J. Hand Surg. Am. 1994, 19, 181–188. [Google Scholar] [CrossRef]
- Stahl, S.; Rozen, N. Tension-band arthrodesis of the small joints of the hand. Orthopedics 2001, 24, 981–983. [Google Scholar] [CrossRef]
- Sheerin, M.; O’Riordan, C.; Conneely, M.; Carey, L.; Ryan, D.; Galvin, R.; Morrissey, A.M. Effectiveness of occupational therapy interventions on function and occupational performance among adults with conditions of the hand, wrist, and forearm: A systematic review and meta-analysis. Aust. Occup. Ther. J. 2024, 71, 175–189. [Google Scholar] [CrossRef]
- Dimitrova, P.; Reger, A.; Prommersberger, K.J.; van Schoonhoven, J.; Mühldorfer-Fodor, M. Effect of a single proximal interphalangeal Joint Fusion of the Index, Middle or Ring Finger on the Grip and Finger Force and Load Distribution in the Hand. Handchir. Mikrochir. Plast. Chir. 2022, 54, 409–417. [Google Scholar] [CrossRef]
- Perren, S.M.; Cordey, J. The concept of interfragmentary strain. In Current Concepts of Internal Fixation of Fractures; Uhthoff, H.K., Ed.; Springer: Berlin, Germany, 1980; pp. 63–77. [Google Scholar]
- Claes, L.E.; Heigele, C.A.; Neidlinger-Wilke, C.; Kaspar, D.; Seidl, W.; Margevicius, K.J.; Augat, P. Effects of mechanical factors on the fracture healing process. Clin. Orthop. Relat. Res. 1998, 355, S132–S147. [Google Scholar] [CrossRef]
- Gilardino, M.S.; Chen, E.; Bartlett, S.P. Choice of internal rigid fixation materials in the treatment of facial fractures. Craniomaxillofacial Trauma Reconstr. 2009, 2, 49–60. [Google Scholar] [CrossRef]
- Gautier, E.; Perren, S.M.; Cordey, J. Effect of plate position relative to bending direction on the rigidity of a plate osteosynthesis. A theoretical analysis. Injury 2000, 31 (Suppl. 3), C14–C20. [Google Scholar] [CrossRef]
- Nousiainen, M. Tension Band Principle. In AO Principles of Fracture Management, 3rd ed.; Buckley, R.E., Moran, C.G., Apivatthakakul, T., Eds.; Georg Thieme Verlag: Stuttgart, Germany, 2017; pp. 345–372. [Google Scholar]
- Bernstein, M.L.; Chung, K.C. Hand fractures and their management: An international view. Injury 2006, 37, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Hashem, A.M. Metacarpal and phalangeal fractures: Experience of a plastic surgeon in a developing country. Plast. Reconstr. Surg. 2010, 126, 201e–203e. [Google Scholar] [CrossRef] [PubMed]
- Darowish, M.; Brenneman, R.; Bigger, J. Dimensional analysis of the distal phalanx with consideration of distal interphalangeal joint arthrodesis using a headless compression screw. Hand 2015, 10, 100–104. [Google Scholar] [CrossRef] [PubMed]
| Technique | ADL | Change of Fusion Angle | Clearance Center | Clearance Palmar |
|---|---|---|---|---|
| [°] | [mm] | [mm] | ||
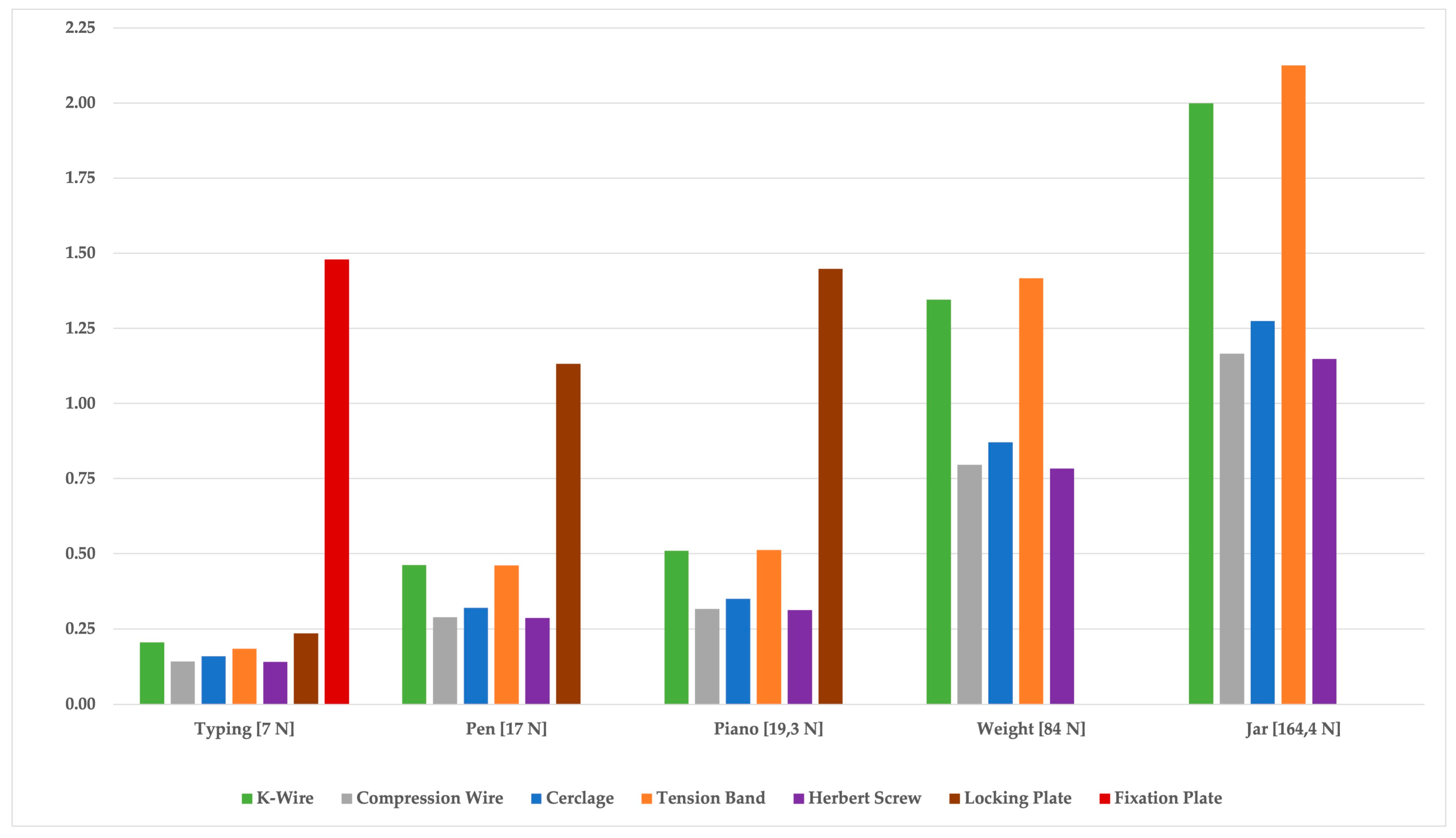
| Cerclage | Typing | 1.83 (1.2–2.5) * | 0.08 (0.05–0.11) | 0.16 (0.10–0.22) |
| Cerclage | Piano | 4.01 (3.6–4.4) * | 0.17 (0.16–0.19) | 0.35 (0.31–0.38) |
| Cerclage | Pencil | 3.67 (3.2–4.1) * | 0.16 (0.14–0.18) | 0.32 (0.28–0.36) |
| Cerclage | Weight | 9.96 (9.1–10.8) * | 0.44 (0.40–0.47) | 0.87 (0.80–0.95) |
| Cerclage | Jar | 14.52 (13.0–16.0) * | 0.64 (0.57–0.70) | 1.27 (1.14–1.41) |
| Compression wire | Typing | 1.61 (1.2–2.1) * | 0.07 (0.05–0.09) | 0.14 (0.10–0.18) |
| Compression wire | Piano | 3.62 (3.3–3.9) * | 0.16 (0.14–0.17) | 0.32 (0.29–0.34) |
| Compression wire | Pencil | 3.31 (3.0–3.6) * | 0.14 (0.13–0.16) | 0.29 (0.26–0.31) |
| Compression wire | Weight | 9.10 (8.6–9.6) * | 0.40 (0.38–0.42) | 0.80 (0.75–0.84) |
| Compression wire | Jar | 13.30 (12.4–14.2) * | 0.58 (0.54–0.62) | 1.17 (1.09–1.25) |
| Fixation Plate | Typing | 16.83 (16.2–17.5) * | 0.74 (0.71–0.77) | 1.48 (1.42–1.54) |
| Fixation Plate | Piano | X | X | X |
| Fixation Plate | Pencil | X | X | X |
| Fixation Plate | Weight | X | X | X |
| Fixation Plate | Jar | X | X | X |
| Herbert Screw | Typing | 1.61 (1.1–2.1) * | 0.07 (0.05–0.09) | 0.14 (0.10–0.18) |
| Herbert Screw | Piano | 3.58 (3.2–3.9) * | 0.16 (0.14–0.17) | 0.31 (0.28–0.34) |
| Herbert Screw | Pencil | 3.27 (2.9–3.6) * | 0.14 (0.13–01.6) | 0.29 (0.25–0.31) |
| Herbert Screw | Weight | 8.97 (8.5–9.5) * | 0.39 (0.37–0.42) | 0.78 (0.74–0.83) |
| Herbert Screw | Jar | 13.10 (12.2–14.0) * | 0.57 (0.53–0.61) | 1.15 (1.07–1.23) |
| K-Wire | Typing | 2.35 (2.0–2.7) | 0.10 (0.09–0.12) | 0.21 (0.17–0.24) |
| K-Wire | Piano | 5.83 (5.6–6.1) | 0.25 (0.24–0.27) | 0.51 (0.49–0.53) |
| K-Wire | Pencil | 5.30 (5.0–5.5) | 0.23 (0.22–0.24) | 0.46 (0.44–0.48) |
| K-Wire | Weight | 15.34 (14.3–16.3) | 0.67 (0.63–0.72) | 1.35 (1.25–1.43) |
| K-Wire | Jar | 22.62 (20.9–24.3) | 1.00 (0.92–1.08) | 2.00 (1.84–2.15) |
| Locking Plate | Typing | 2.70 (2.5–2.9) * | 0.12 (0.11–0.13) | 0.24 (0.22–0.25) |
| Locking Plate | Piano | 16.48 (16.0–17.0) * | 0.72 (0.70–0.75) | 1.45 (1.41–1.49) |
| Locking Plate | Pencil | 12.92 (12.6–13.3) * | 0.57 (0.55–0.58) | 1.13 (1.10–1.17) |
| Locking Plate | Weight | X | X | X |
| Locking Plate | Jar | X | X | X |
| Tension Band | Typing | 2.11 (1.7–2.5) | 0.09 (0.07–0.11) | 0.18 (0.15–0.22) |
| Tension Band | Piano | 5.87 (5.6–6.1) | 0.26 (0.24–0.27) | 0.51 (0.49–0.53) |
| Tension Band | Pencil | 5.29 (5.0–5.6) | 0.23 (0.22–0.24) | 0.46 (0.44–0.49) |
| Tension Band | Weight | 16.13 (15.0–17.3) | 0.71 (0.66–0.76) | 1.42 (1.32–1.52) |
| Tension Band | Jar | 24.00 (22.0–26.0) | 1.06 (0.97–1.15) | 2.13 (1.94–2.31) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Millrose, M.; Ittermann, T.; Vonderlind, H.C.; Willauschus, M.; Rüther, J.; Bail, H.-J.; Geßlein, M. Biomechanical Analysis of Micromotion of Proximal Interphalangeal Joint Arthrodeses During Activities of Daily Life In Vitro. J. Clin. Med. 2025, 14, 4420. https://doi.org/10.3390/jcm14134420
Millrose M, Ittermann T, Vonderlind HC, Willauschus M, Rüther J, Bail H-J, Geßlein M. Biomechanical Analysis of Micromotion of Proximal Interphalangeal Joint Arthrodeses During Activities of Daily Life In Vitro. Journal of Clinical Medicine. 2025; 14(13):4420. https://doi.org/10.3390/jcm14134420
Chicago/Turabian StyleMillrose, Michael, Till Ittermann, Hans Christoph Vonderlind, Maximilian Willauschus, Johannes Rüther, Hermann-Josef Bail, and Markus Geßlein. 2025. "Biomechanical Analysis of Micromotion of Proximal Interphalangeal Joint Arthrodeses During Activities of Daily Life In Vitro" Journal of Clinical Medicine 14, no. 13: 4420. https://doi.org/10.3390/jcm14134420
APA StyleMillrose, M., Ittermann, T., Vonderlind, H. C., Willauschus, M., Rüther, J., Bail, H.-J., & Geßlein, M. (2025). Biomechanical Analysis of Micromotion of Proximal Interphalangeal Joint Arthrodeses During Activities of Daily Life In Vitro. Journal of Clinical Medicine, 14(13), 4420. https://doi.org/10.3390/jcm14134420









