Work Absenteeism in Inflammatory Bowel Disease Patients Related to Patient-Reported Anxiety Levels and Disease Activity: The IBD-GO-WORK Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Questionnaire Structure: Collected Variables
2.2.1. General Section of the Questionnaire
2.2.2. Psychometric Assessment Section for Anxiety Levels
2.2.3. Section Assessing Patient-Reported IBD Disease Activity
2.2.4. Section Assessing Work Absenteeism
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Sample
3.2. Demographic Factors Associated with Reduced Work Productivity
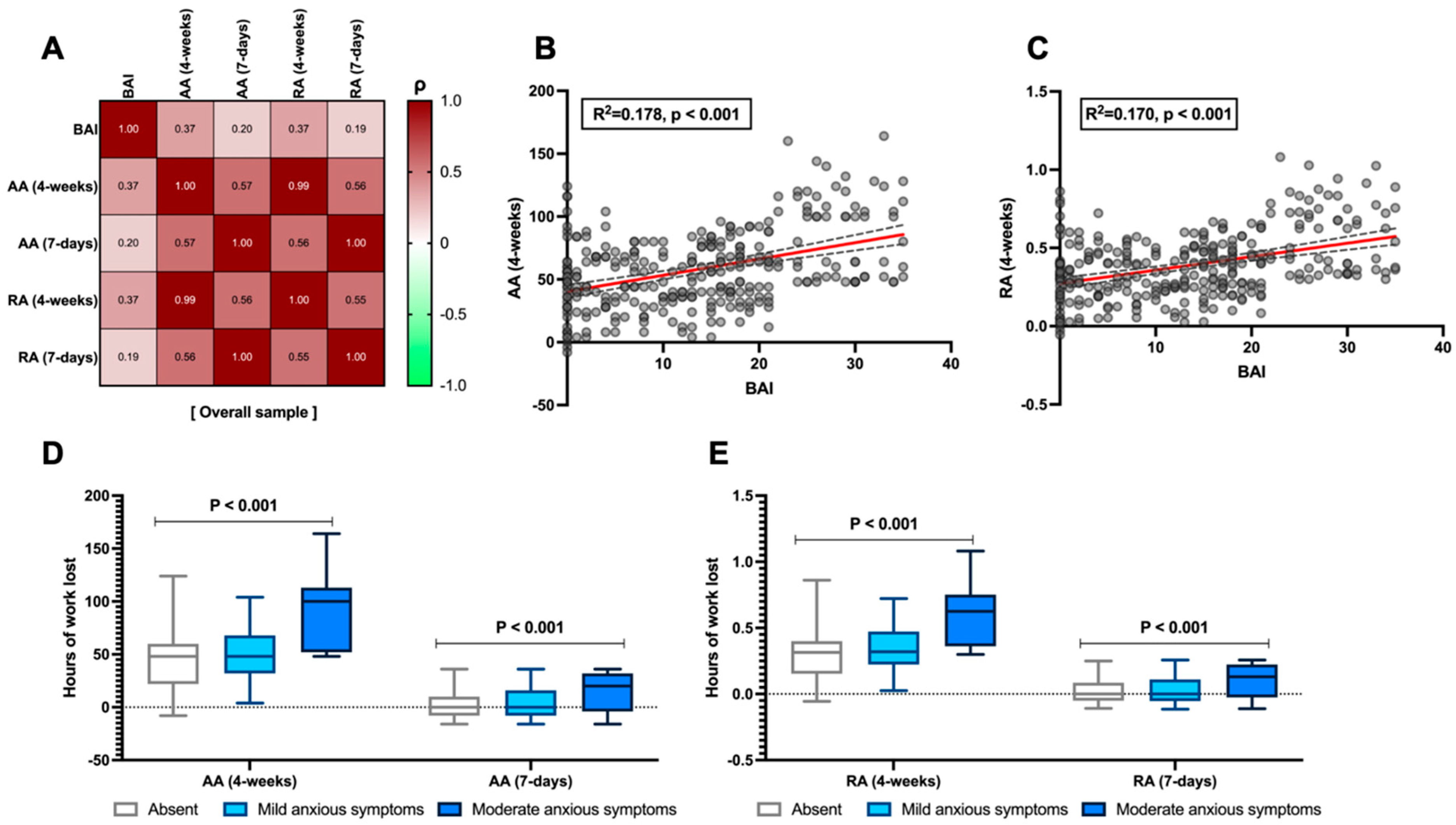
3.3. The Relationship Between Anxiety Symptoms and Work Productivity
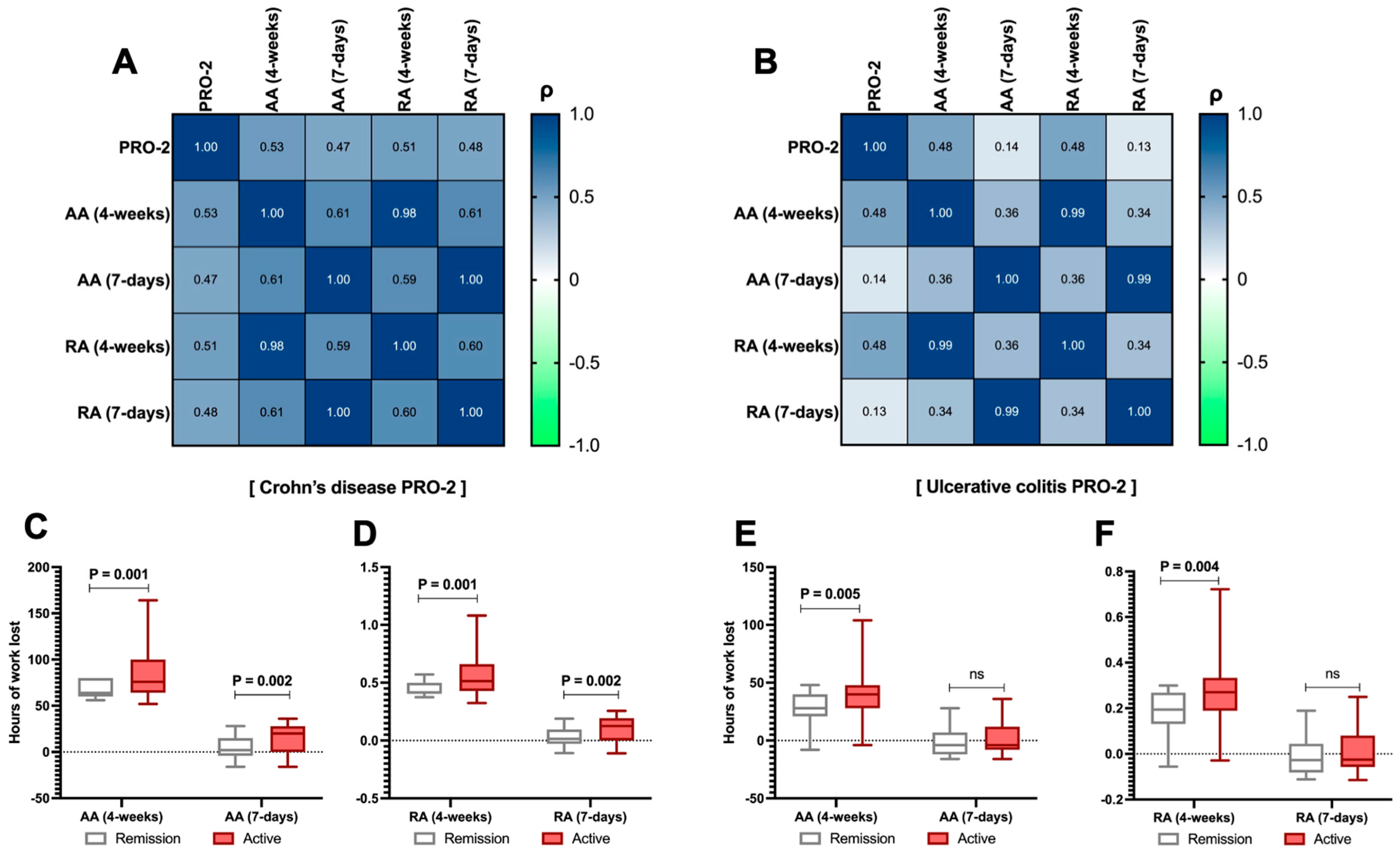
3.4. The Impact of Disease Activity Assessed Through PRO-2 and Work Productivity
3.5. Productivity Differences Within the Sample Based on Educational Level and Type of Work Performed
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, J.T. Pathophysiology of Inflammatory Bowel Diseases. N. Engl. J. Med. 2020, 383, 2652–2664. [Google Scholar] [CrossRef]
- Lo, B.; Prosberg, M.V.; Gluud, L.L.; Chan, W.; Leong, R.W.; van der List, E.; van der Have, M.; Sarter, H.; Gower-Rousseau, C.; Peyrin-Biroulet, L.; et al. Systematic Review and Meta-Analysis: Assessment of Factors Affecting Disability in Inflammatory Bowel Disease and the Reliability of the Inflammatory Bowel Disease Disability Index. Aliment. Pharmacol. Ther. 2018, 47, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Papadimitriou, K.; Deligiannidou, G.-E.; Voulgaridou, G.; Giaginis, C.; Papadopoulou, S.K. Nutritional Habits in Crohn’s Disease Onset and Management. Nutrients 2025, 17, 559. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Ricciuto, A.; Lewis, A.; D’Amico, F.; Dhaliwal, J.; Griffiths, A.M.; Bettenworth, D.; Sandborn, W.J.; Sands, B.E.; Reinisch, W.; et al. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target Strategies in IBD. Gastroenterology 2021, 160, 1570–1583. [Google Scholar] [CrossRef] [PubMed]
- Colombel, J.-F. Disease Clearance in Inflammatory Bowel Disease. Gastroenterol. Hepatol. 2021, 17, 233–235. [Google Scholar]
- Gomez, D.A.; Ahmad-Waqar, M.; Brookes, M.J.; Kumar, A. IBD-Related Mental Health Disorders: Where Do We Go from Here? Frontline Gastroenterol. 2023, 14, 512–520. [Google Scholar] [CrossRef]
- Leenhardt, R.; Rivière, P.; Papazian, P.; Nion-Larmurier, I.; Girard, G.; Laharie, D.; Marteau, P. Sexual Health and Fertility for Individuals with Inflammatory Bowel Disease. World J. Gastroenterol. 2019, 25, 5423–5433. [Google Scholar] [CrossRef]
- Romano, L.; Pellegrino, R.; Arcaniolo, D.; Gravina, A.G.; Miranda, A.; Priadko, K.; De Gennaro, N.; Santonastaso, A.; Palladino, G.; Crocetto, F.; et al. Lower Urinary Tract Symptoms in Patients with Inflammatory Bowel Diseases: A Cross-Sectional Observational Study. Dig. Liver Dis. 2024, 56, 628–634. [Google Scholar] [CrossRef]
- Gravina, A.G.; Pellegrino, R.; Palladino, G.; Zanini, A.; Federico, A.; Zingone, F. Too Many Couch Potatoes Among Middle-Aged Inflammatory Bowel Disease Patients: Findings from the “BE-FIT-IBD-2” Study. Gastroenterol. Insights 2024, 15, 963–975. [Google Scholar] [CrossRef]
- Gravina, A.G.; Pellegrino, R.; Palladino, G.; Imperio, G.; Ventura, A.; Cipullo, M.; Coppola, A.; Federico, A. Profiling the Patient with Inflammatory Bowel Disease in the Relationship between Physical Activity and Partner/Social Network Status: A Post Hoc Patient-Tailored Analysis of the “BE-FIT-IBD” Study. Gastroenterol. Hepatol. 2025, 48, 502203. [Google Scholar] [CrossRef]
- Harbord, M.; Annese, V.; Vavricka, S.R.; Allez, M.; Barreiro-de Acosta, M.; Boberg, K.M.; Burisch, J.; De Vos, M.; De Vries, A.-M.; Dick, A.D.; et al. The First European Evidence-Based Consensus on Extra-Intestinal Manifestations in Inflammatory Bowel Disease. J. Crohn’s Colitis 2016, 10, 239–254. [Google Scholar] [CrossRef]
- Sange, A.H.; Srinivas, N.; Sarnaik, M.K.; Modi, S.; Pisipati, Y.; Vaidya, S.; Syed Gaggatur, N.; Sange, I. Extra-Intestinal Manifestations of Inflammatory Bowel Disease. Cureus 2021, 13, e17187. [Google Scholar] [CrossRef]
- Viganò, C.; Mulinacci, G.; Palermo, A.; Barisani, D.; Pirola, L.; Fichera, M.; Invernizzi, P.; Massironi, S. Impact of COVID-19 on Inflammatory Bowel Disease Practice and Perspectives for the Future. World J. Gastroenterol. 2021, 27, 5520–5535. [Google Scholar] [CrossRef]
- Pellegrino, R.; Pellino, G.; Selvaggi, F.; Federico, A.; Romano, M.; Gravina, A.G. Therapeutic Adherence Recorded in the Outpatient Follow-up of Inflammatory Bowel Diseases in a Referral Center: Damages of COVID-19. Dig. Liver Dis. 2022, 54, 1449–1451. [Google Scholar] [CrossRef]
- Leso, V.; Gervetti, P.; Macrini, M.C.; Russo, F.; Iavicoli, I. Inflammatory Bowel Diseases and Work Disability: A Systematic Review of Predictive Factors. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 165–181. [Google Scholar] [CrossRef]
- Youssef, M.; Hossein-Javaheri, N.; Hoxha, T.; Mallouk, C.; Tandon, P. Work Productivity Impairment in Persons with Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. J. Crohn’s Colitis 2024, 18, 1486–1504. [Google Scholar] [CrossRef]
- Wang, R.; Li, Z.; Liu, S.; Zhang, D. Global, Regional and National Burden of Inflammatory Bowel Disease in 204 Countries and Territories from 1990 to 2019: A Systematic Analysis Based on the Global Burden of Disease Study 2019. BMJ Open 2023, 13, e065186. [Google Scholar] [CrossRef]
- Manceur, A.M.; Ding, Z.; Muser, E.; Obando, C.; Voelker, J.; Pilon, D.; Kinkead, F.; Lafeuille, M.-H.; Lefebvre, P. Burden of Crohn’s Disease in the United States: Long-Term Healthcare and Work-Loss Related Costs. J. Med. Econ. 2020, 23, 1092–1101. [Google Scholar] [CrossRef]
- Zagórowicz, E.; Binowski, G.; Strządała, D.; Pruszko, C.; Kucha, P.; Reguła, J. Savings in Social Expenditures for Work Incapacity in Patients with Inflammatory Bowel Disease Depend on Access to Innovative Therapies in Poland. Eur. J. Gastroenterol. Hepatol. 2024, 36, 695–703. [Google Scholar] [CrossRef]
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial Diagnosis, Monitoring of Known IBD, Detection of Complications. J. Crohn’s Colitis 2019, 13, 144–164. [Google Scholar] [CrossRef]
- Harvey, R.F.; Bradshaw, J.M. A Simple Index of Crohn’s-Disease Activity. Lancet 1980, 1, 514. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.D.; Chuai, S.; Nessel, L.; Lichtenstein, G.R.; Aberra, F.N.; Ellenberg, J.H. Use of the Noninvasive Components of the Mayo Score to Assess Clinical Response in Ulcerative Colitis. Inflamm. Bowel Dis. 2008, 14, 1660–1666. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE Guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An Inventory for Measuring Clinical Anxiety: Psychometric Properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.; Zou, G.; D’Haens, G.; Feagan, B.G.; Sandborn, W.J.; Vandervoort, M.K.; Rolleri, R.L.; Bortey, E.; Paterson, C.; Forbes, W.P.; et al. A Retrospective Analysis: The Development of Patient Reported Outcome Measures for the Assessment of Crohn’s Disease Activity. Aliment. Pharmacol. Ther. 2015, 41, 77–86. [Google Scholar] [CrossRef]
- Jairath, V.; Khanna, R.; Zou, G.Y.; Stitt, L.; Mosli, M.; Vandervoort, M.K.; D’Haens, G.; Sandborn, W.J.; Feagan, B.G.; Levesque, B.G. Development of Interim Patient-Reported Outcome Measures for the Assessment of Ulcerative Colitis Disease Activity in Clinical Trials. Aliment. Pharmacol. Ther. 2015, 42, 1200–1210. [Google Scholar] [CrossRef]
- Kessler, R.C.; Ames, M.; Hymel, P.A.; Loeppke, R.; McKenas, D.K.; Richling, D.E.; Stang, P.E.; Ustun, T.B. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to Evaluate the Indirect Workplace Costs of Illness. J. Occup. Environ. Med. 2004, 46, S23–S37. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barber, C.; Beck, A.; Berglund, P.; Cleary, P.D.; McKenas, D.; Pronk, N.; Simon, G.; Stang, P.; Ustun, T.B.; et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J. Occup. Environ. Med. 2003, 45, 156–174. [Google Scholar] [CrossRef]
- Noor, N.M.; Lee, J.C.; Bond, S.; Dowling, F.; Brezina, B.; Patel, K.V.; Ahmad, T.; Banim, P.J.; Berrill, J.W.; Cooney, R.; et al. A Biomarker-Stratified Comparison of Top-down versus Accelerated Step-up Treatment Strategies for Patients with Newly Diagnosed Crohn’s Disease (PROFILE): A Multicentre, Open-Label Randomised Controlled Trial. Lancet Gastroenterol. Hepatol. 2024, 9, 415–427. [Google Scholar] [CrossRef]
- Kuenzig, M.E.; Fung, S.G.; Marderfeld, L.; Mak, J.W.Y.; Kaplan, G.G.; Ng, S.C.; Wilson, D.C.; Cameron, F.; Henderson, P.; Kotze, P.G.; et al. Twenty-First Century Trends in the Global Epidemiology of Pediatric-Onset Inflammatory Bowel Disease: Systematic Review. Gastroenterology 2022, 162, 1147–1159.e4. [Google Scholar] [CrossRef]
- Piovani, D.; Danese, S.; Peyrin-Biroulet, L.; Nikolopoulos, G.K.; Lytras, T.; Bonovas, S. Environmental Risk Factors for Inflammatory Bowel Diseases: An Umbrella Review of Meta-Analyses. Gastroenterology 2019, 157, 647–659.e4. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Sebastian, S.A.; Parmar, M.P.; Ghadge, N.; Padda, I.; Keshta, A.S.; Minhaz, N.; Patel, A. Factors Influencing the Quality of Life in Inflammatory Bowel Disease: A Comprehensive Review. Dis. Mon. 2024, 70, 101672. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Rohde, J.; Farraye, F.A. Stigma and Disclosure in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2020, 26, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Ross, E.J.; Shanahan, M.L.; Joseph, E.; Reynolds, J.M.; Jimenez, D.E.; Abreu, M.T.; Carrico, A.W. The Relationship Between Loneliness, Social Isolation, and Inflammatory Bowel Disease: A Narrative Review. Ann. Behav. Med. 2024, 58, 779–788. [Google Scholar] [CrossRef]
- Sciberras, M.; Karmiris, K.; Nascimento, C.; Tabone, T.; Nikolaou, P.; Theodoropoulou, A.; Mula, A.; Goren, I.; Yanai, H.; Amir, H.; et al. Mental Health, Work Presenteeism, and Exercise in Inflammatory Bowel Disease. J. Crohn’s Colitis 2022, 16, 1197–1201. [Google Scholar] [CrossRef]
- Nasr, S.; Dahmani, W.; Jaziri, H.; Hammami, A.; Slama, A.B.; Ameur, W.B.; Elleuch, N.; Ksiaa, M.; Jmaa, A. Exploring Work Productivity Loss in Patients with Inflammatory Bowel Disease. Future Sci. OA 2023, 9, FSO872. [Google Scholar] [CrossRef]
- Andersen, V.; Pingel, J.; Søfelt, H.L.; Hikmat, Z.; Johansson, M.; Pedersen, V.S.; Bertelsen, B.; Carlsson, A.; Lindh, M.; Svavarsdóttir, E.; et al. Sex and Gender in Inflammatory Bowel Disease Outcomes and Research. Lancet Gastroenterol. Hepatol. 2024, 9, 1041–1051. [Google Scholar] [CrossRef]
- Domènech, E.; Mañosa, M.; Cabré, E. An Overview of the Natural History of Inflammatory Bowel Diseases. Dig. Dis. 2014, 32, 320–327. [Google Scholar] [CrossRef]
- Parra, R.S.; Chebli, J.M.F.; Amarante, H.M.B.S.; Flores, C.; Parente, J.M.L.; Ramos, O.; Fernandes, M.; Rocha, J.J.R.; Feitosa, M.R.; Feres, O.; et al. Quality of Life, Work Productivity Impairment and Healthcare Resources in Inflammatory Bowel Diseases in Brazil. World J. Gastroenterol. 2019, 25, 5862–5882. [Google Scholar] [CrossRef]
- Zand, A.; van Deen, W.K.; Inserra, E.K.; Hall, L.; Kane, E.; Centeno, A.; Choi, J.M.; Ha, C.Y.; Esrailian, E.; DʼHaens, G.R.; et al. Presenteeism in Inflammatory Bowel Diseases: A Hidden Problem with Significant Economic Impact. Inflamm. Bowel Dis. 2015, 21, 1623–1630. [Google Scholar] [CrossRef]
- Nardone, O.M.; Calabrese, G.; La Mantia, A.; Caso, R.; Testa, A.; Castiglione, F. Insights into Disability and Psycho-Social Care of Patients with Inflammatory Bowel Disease. Front. Med. 2024, 11, 1416054. [Google Scholar] [CrossRef] [PubMed]
- van Gennep, S.; Gielen, M.E.; Rietdijk, S.T.; de Boer, N.K.H.; Duijvestein, M.; Gecse, K.B.; Ponsioen, C.Y.; D’Haens, G.R.; de Boer, A.G.E.M.; Löwenberg, M. Work Productivity Loss Is Determined by Fatigue and Reduced Quality of Life in Employed Inflammatory Bowel Disease Patients: A Prospective Multicentre Cohort Study. Eur. J. Gastroenterol. Hepatol. 2021, 33, e594–e602. [Google Scholar] [CrossRef] [PubMed]
- Barberio, B.; Zamani, M.; Black, C.J.; Savarino, E.V.; Ford, A.C. Prevalence of Symptoms of Anxiety and Depression in Patients with Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Spina, A.; Mazzarella, C.; Dallio, M.; Romeo, M.; Pellegrino, R.; Durante, T.; Romano, M.; Loguercio, C.; Di Mauro, M.; Federico, A.; et al. The Lesson from the First Italian Lockdown: Impacts on Anxiety and Depressive Symptoms and Sleep Quality in Patients with Remission of Inflammatory Bowel Disease. Rev. Recent. Clin. Trials 2022, 17, 109–119. [Google Scholar] [CrossRef]
- Marcon, T.; Lorenzon, G.; Zanotti, R.; Danielis, M. Anxiety and Work Disability in Patients with Immune-Mediated Inflammatory Diseases: A Cross-Sectional Study from a Single Center. Gastroenterol. Nurs. 2024, 47, 349–357. [Google Scholar] [CrossRef]


| Variable | CD N = 133 | UC N = 167 | p-Value 1 |
|---|---|---|---|
| Age (y) | 44 (29–55) | 43 (32–56) | 0.681 |
| Gender | 0.175 3 | ||
| Male | 66 (49.6%) | 96 (57.5%) | |
| Female | 67 (50.4%) | 71 (42.5%) | |
| BMI (Kg/m2) | 27.05 (22.76–32.24) | 27.47 (23.72–31.53) | 0.543 |
| Education level | 0.015 | ||
| Primary | 53 (39.8%) | 40 (24%) | |
| Secondary | 61 (45.9%) | 94 (56.3%) | |
| Degree | 19 (14.3%) | 33 (19.8%) | |
| Job-status | 0.163 | ||
| Freelancer | 62 (46.6%) | 56 (33.5%) | |
| Employee | 23 (17.3%) | 48 (28.7%) | |
| Entrepreneur | 20 (15%) | 26 (15.6%) | |
| Worker | 10 (7.5%) | 15 (9%) | |
| Student | 14 (10.5%) | 18 (10.8%) | |
| Intern (stage) | 4 (3%) | 4 (2.4%) | |
| Smoking status | 0.0001 | ||
| Active | 33 (24.8%) | 30 (18%) | |
| Past smoker | 44 (33.1%) | 27 (16.2%) | |
| Never | 56 (42.1%) | 110 (65.9%) | |
| Alcohol consumer 2 | 0.460 3 | ||
| Yes | 25 (18.8%) | 26 (15.6%) | |
| Partner (yes) | 91 (68.4%) | 108 (64.7%) | 0.495 3 |
| Biologics (yes) | 98 (73.7%) | 96 (57.5%) | 0.004 3 |
| Steroids active use (yes) | 5 (3.8%) | 9 (5.4%) | 0.399 3 |
| Associated arthritis (yes) | 49 (36.8%) | 51 (30.5%) | 0.250 3 |
| Diabetes (yes) | 25 (18.8%) | 22 (13.2%) | 0.183 3 |
| Previous surgery 4 (yes) | 85 (63.9%) | 49 (29.3%) | <0.001 3 |
| Active disease (yes) | 105 (78.9%) | 143 (85.6%) | 0.700 3 |
| Variable | N | Absolute Absenteeism (4-Weeks) | p-Value a | Absolute Absenteeism (7-Days) | p-Value b | Relative Absenteeism (4-Weeks) | p-Value c | Relative Absenteeism (7-Days) | p-Value d |
|---|---|---|---|---|---|---|---|---|---|
| Crohn’s disease | 133 | 76 (64–92) # | <0.001 | 12 (0–28) # | <0.001 | 0.5 (0.4–0.62) # | <0.001 | 0.08 (0–0.19) # | <0.001 |
| Ulcerative colitis | 167 | 40 (28–48) | a | −4 (−8–12) | 0.25 (0.17–0.32) | −0.025 (−0.05–0.075) | |||
| Males | 162 | 50 (32–68) | 0.024 | 0 (−8–16) | 0.381 | 0.33 (0.22–0.47) | 0.044 | 0 (−0.05–0.11) | 0.4 |
| Females | 138 | 60 (40–84) # | a | 8 (−8–21) | 0.4 (0.25–0.55) # | 0.05 (−0.05–0.14) | |||
| Alcohol (no) | 249 | 52 (36–76) | 0.450 | 0 (−4–20) | 0.574 | 0.36 (0.25–0.5) | 0.559 | 0 (−0.02–0.135) | 0.555 |
| Alcohol (yes) | 51 | 60 (36–80) | 4 (−8–20) | 0.37 (0.24–0.51) | 0.02 (−0.05–0.125) | ||||
| Arthritis (no) | 200 | 52 (36–76) | 0.246 | 4 (−7–20) | 0.653 | 0.36 (0.23–0.5) | 0.195 | 0.02 (−0.04–0.132) | 0.677 |
| Arthritis (yes) | 100 | 56 (36–80) | 0 (−8–20) | 0.38 (0.25–0.54) | 0 (−0.05–0.135) | ||||
| Diabetes (no) | 253 | 52 (36–76) | 0.087 | 0 (−8–20) | 0.095 | 0.35 (0.24–0.49) | 0.067 | 0 (−0.05–0.125) | 0.091 |
| Diabetes (yes) | 47 | 64 (36–92) | 12 (−4–24) | 0.43 (0.25–0.62) | 0.08 (−0.02–0.171) | ||||
| Smoking (no) | 237 | 52 (36–76) | 0.036 | 0 (−8–20) | 0.519 | 0.35 (0.24–0.5) | 0.04 | 0 (−0.05–0.138) | 0.549 |
| Smoking (yes) | 63 | 60 (40–80) # | 8 (−4–16) | 0.4 (0.27–0.52) # | 0.05 (−0.02–0.114) | ||||
| Partner (no) | 101 | 52 (34–78) | 0.736 | 0 (−12–20) | 0.407 | 0.36 (0.22–0.5) | 0.684 | 0 (−0.75–0.142) | 0.427 |
| Partner (yes) | 199 | 56 (36–76) | 4 (−4–20) | 0.37 (0.25–0.51) | 0.028 (−0.02–0.125) | ||||
| Biologic/SM (no) | 106 | 46 (32–76) | 0.016 | 0 (−8–20) | 0.904 | 0.3 (0.2–0.5) | 0.024 | 0 (−0.05–0.13) | 0.845 |
| Biologic/SM (yes) | 194 | 60 (40–77) # | 4 (−8–20) | 0.4 (0.266–0.51) # | 0.02 (−0.05–0.13) | ||||
| No surgery | 166 | 48 (32–64) | <0.001 | 0 (−8–16) | 0.011 | 0.3 (0.21–0.43) | <0.001 | 0 (−0.05–0.11) | 0.014 |
| Previous surgery | 134 | 64 (44–88) # | 8 (−4–24) # | 0.42 (0.28–0.58) # | 0.05 (−0.02–0.15) # |
| Variable | N | Usual Performance of Colleagues [0–10] | p-Value a | Self-Perceived Usual Job Performance (1–2 Years) [0–10] | p-Value a | Self-Perceived Usual Job Performance (4-Weeks) [0–10] | p-Value a |
|---|---|---|---|---|---|---|---|
| Crohn’s disease | 133 | 8 (6–9) | 0.625 | 4 (2–7) | <0.001 | 3 (2–6) | <0.001 |
| Ulcerative colitis | 167 | 8 (6–9) | 6 (4–9) | 6 (3–8) | |||
| Males | 162 | 8 (6–9) | 0.225 | 6 (3–8) | 0.116 | 5 (2–8) | 0.397 |
| Females | 138 | 8 (6.75–9) | 5 (3–8) | 5 (2–7) | |||
| Alcohol (no) | 249 | 8 (6–9) | 0.791 | 6 (3–8) | 0.989 | 5 (2–8) | 0.481 |
| Alcohol (yes) | 51 | 7 (7–9) | 5 (3–8) | 5 (2–7) | |||
| Arthritis (no) | 200 | 8 (6–9) | 0.924 | 5 (3–8) | 0.766 | 5 (2–7) | 0.769 |
| Arthritis (yes) | 100 | 8 (6–9) | 6 (3–7) | 5 (2–8) | |||
| Diabetes (no) | 253 | 8 (6–9) | 0.569 | 6 (3–8) | 0.087 | 5 (2–8) | 0.083 |
| Diabetes (yes) | 47 | 8 (6–9) | 4 (2–8) | 4 (2–6) | |||
| Smoking (no) | 237 | 8 (6–9) | 0.207 | 6 (3–8) | 0.356 | 5 (2–7) | 0.355 |
| Smoking (yes) | 63 | 8 (6–9) | 5 (2–8) | 5 (2–7) | |||
| Partner (no) | 101 | 8 (7–9) | 0.225 | 6 (3–8) | 0.116 | 5 (2–7) | 0.397 |
| Partner (yes) | 199 | 8 (6–9) | 5 (3–8) | 5 (2–8) | |||
| Biologic/SM (no) | 106 | 8 (6–9) | 0.836 | 6 (3–9) | 0.659 | 5 (2–8) | 0.971 |
| Biologic/SM (yes) | 194 | 8 (6–9) | 5 (3–8) | 5 (2–7) | |||
| No surgery | 166 | 8 (6–9) | 0.698 | 6 (3–8) | 0.02 | 5 (3–8) | 0.698 |
| Previous surgery | 134 | 8 (6–9) | 4 (3–7.25) # | 4 (2–7) | |||
| No anxiety | 42 | 8 (6–9) | 0.739 | 6 (4–8) | 0.003 | 6 (4–9) | 0.001 |
| Mild anxious symptoms | 196 | 8 (6–9) | 6 (3–8) | 5 (2–8) | |||
| Moderate anxious symptoms | 62 | 7 (6–9) | 3 (2–6.25) # | 3 (1.75–5)# | |||
| Crohn’s disease (remission) | 28 | 8 (7–9) | 0.472 | 5.5 (3–8) | 0.094 | 5 (2.25–8) | 0.034 |
| Crohn’s disease (active) | 105 | 8 (6–9) | 4 (2–6) | 3 (1.5–5) # | |||
| Ulcerative colitis (remission) | 143 | 8 (6–9) | 0.662 | 6 (3–9) | 0.197 | 6 (3–8) | 0.539 |
| Ulcerative colitis (active) | 24 | 8 (6–10) | 8 (4.25–9) | 5 (4.25–8.75) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellegrino, R.; De Costanzo, I.; Imperio, G.; Izzo, M.; Landa, F.; Durante, A.; Federico, A.; Gravina, A.G. Work Absenteeism in Inflammatory Bowel Disease Patients Related to Patient-Reported Anxiety Levels and Disease Activity: The IBD-GO-WORK Study. J. Clin. Med. 2025, 14, 4410. https://doi.org/10.3390/jcm14134410
Pellegrino R, De Costanzo I, Imperio G, Izzo M, Landa F, Durante A, Federico A, Gravina AG. Work Absenteeism in Inflammatory Bowel Disease Patients Related to Patient-Reported Anxiety Levels and Disease Activity: The IBD-GO-WORK Study. Journal of Clinical Medicine. 2025; 14(13):4410. https://doi.org/10.3390/jcm14134410
Chicago/Turabian StylePellegrino, Raffaele, Ilaria De Costanzo, Giuseppe Imperio, Michele Izzo, Fabio Landa, Andrea Durante, Alessandro Federico, and Antonietta Gerarda Gravina. 2025. "Work Absenteeism in Inflammatory Bowel Disease Patients Related to Patient-Reported Anxiety Levels and Disease Activity: The IBD-GO-WORK Study" Journal of Clinical Medicine 14, no. 13: 4410. https://doi.org/10.3390/jcm14134410
APA StylePellegrino, R., De Costanzo, I., Imperio, G., Izzo, M., Landa, F., Durante, A., Federico, A., & Gravina, A. G. (2025). Work Absenteeism in Inflammatory Bowel Disease Patients Related to Patient-Reported Anxiety Levels and Disease Activity: The IBD-GO-WORK Study. Journal of Clinical Medicine, 14(13), 4410. https://doi.org/10.3390/jcm14134410








