Return to Work After Work-Related Injuries: A Systematic Review and Meta-Analysis of Incidence and Determinants
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
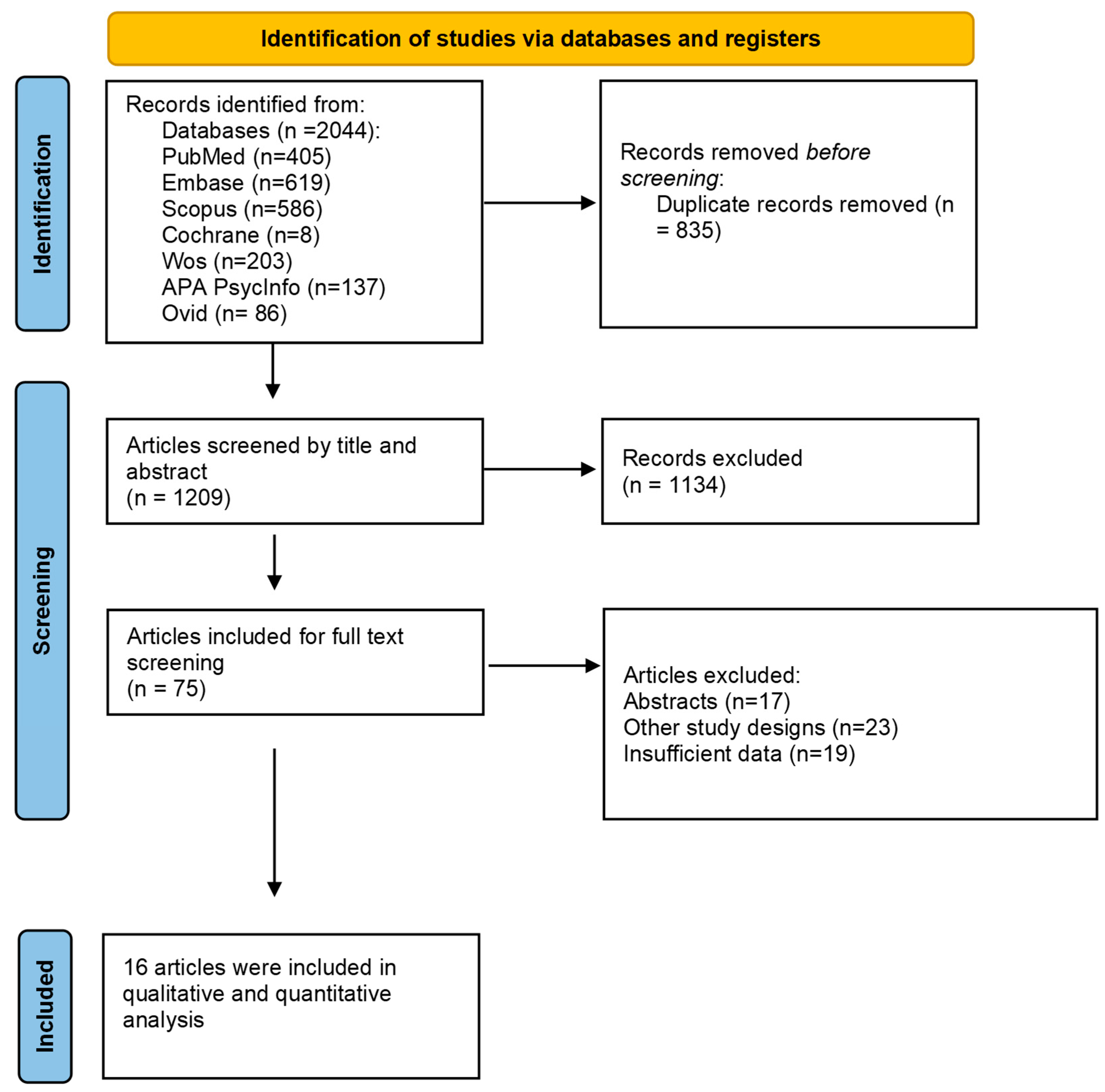
2.4. Screening Process
2.5. Data Extraction
2.6. Risk of Bias Assessment
2.7. Statistical Analysis
2.8. Ethical Considerations
3. Results
3.1. Risk of Bias Assessment
3.2. Outcomes
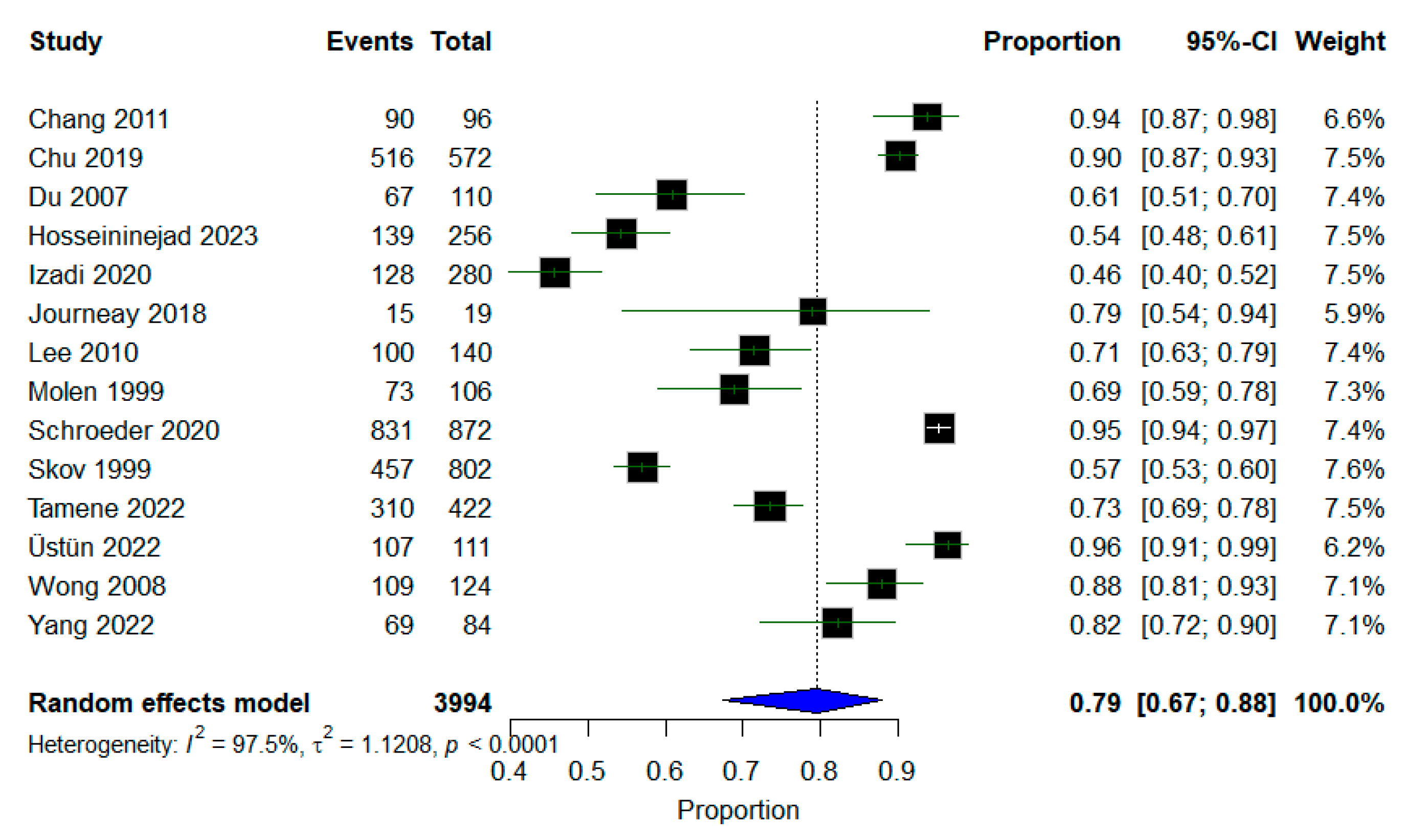
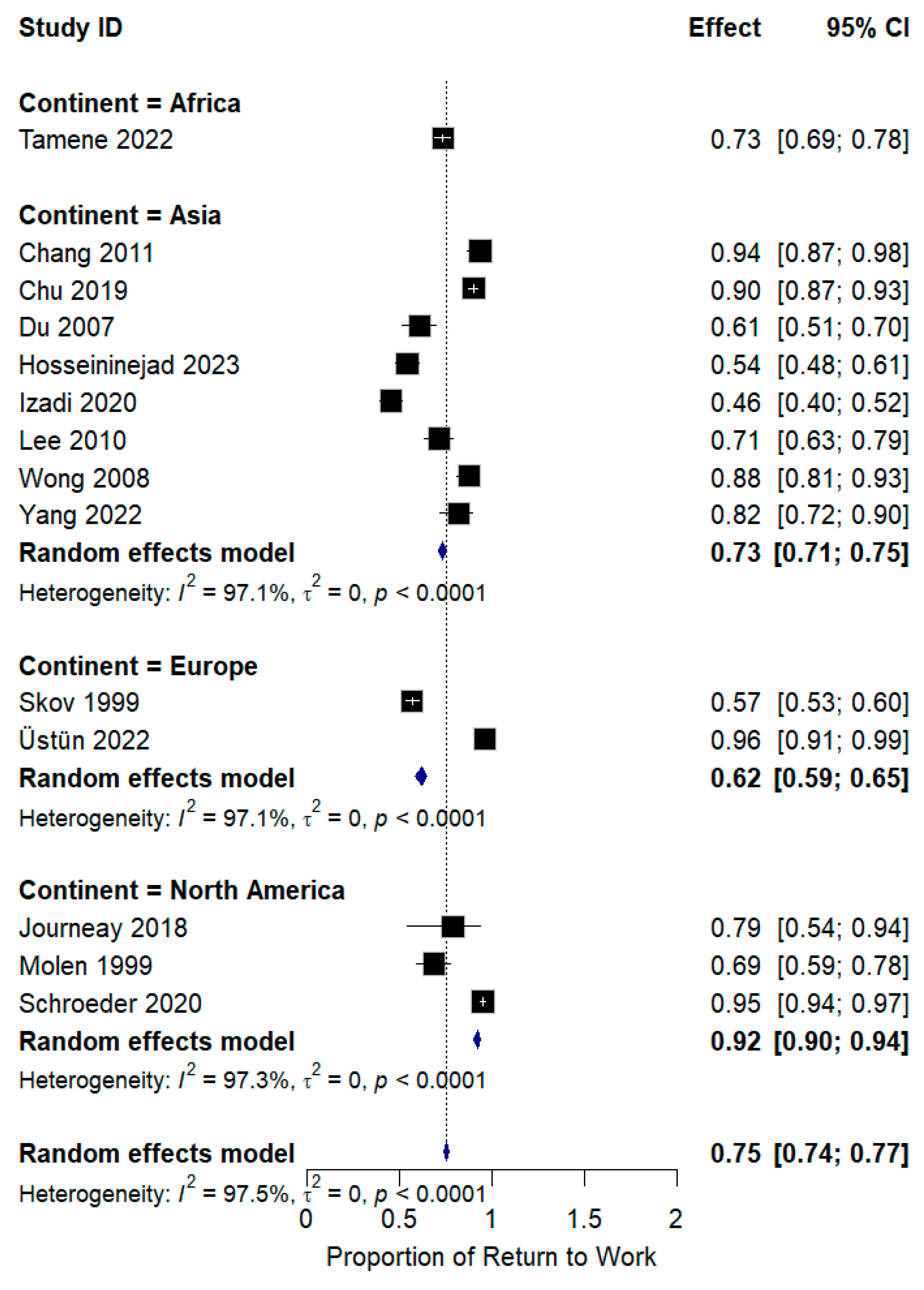
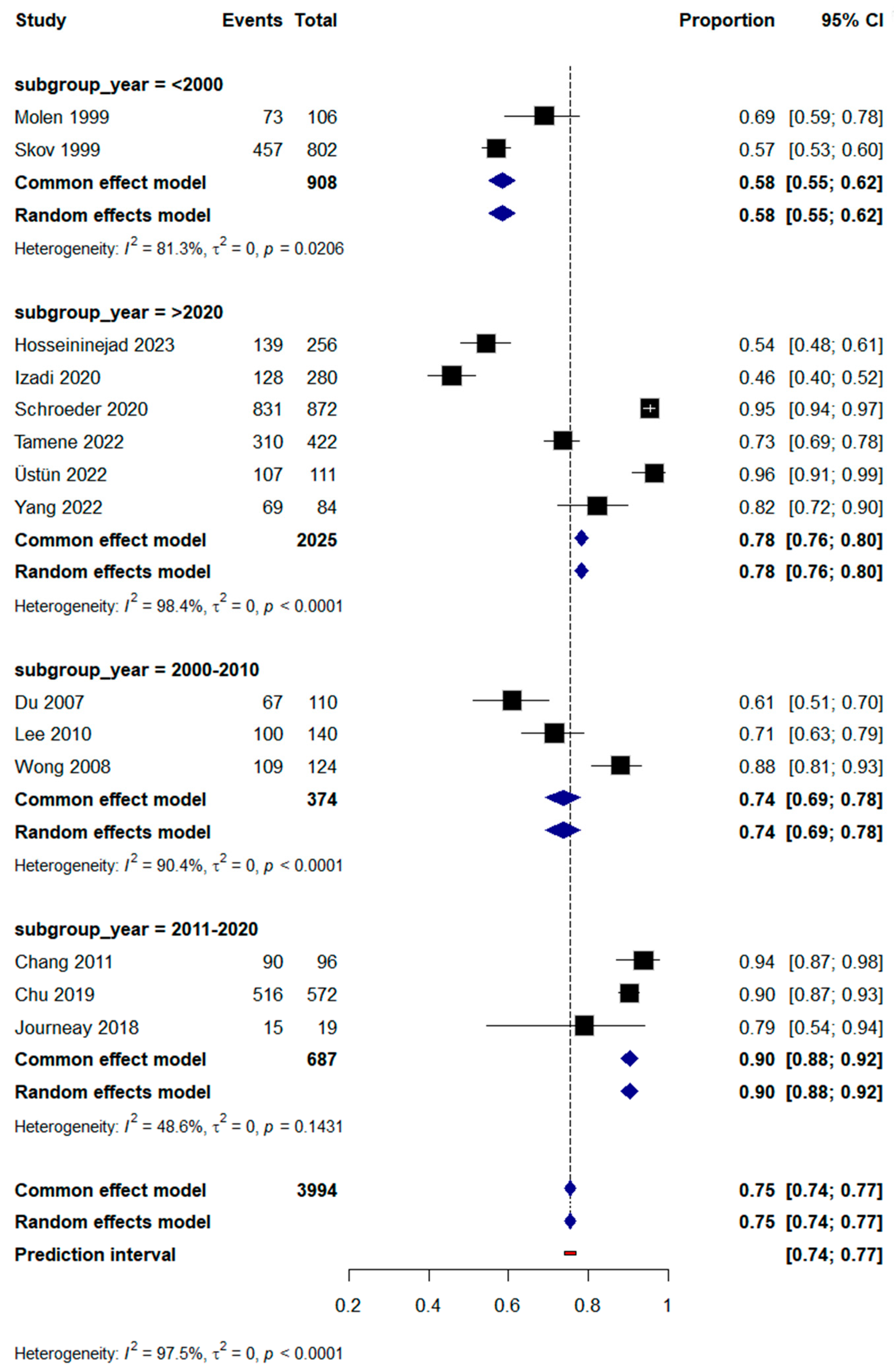
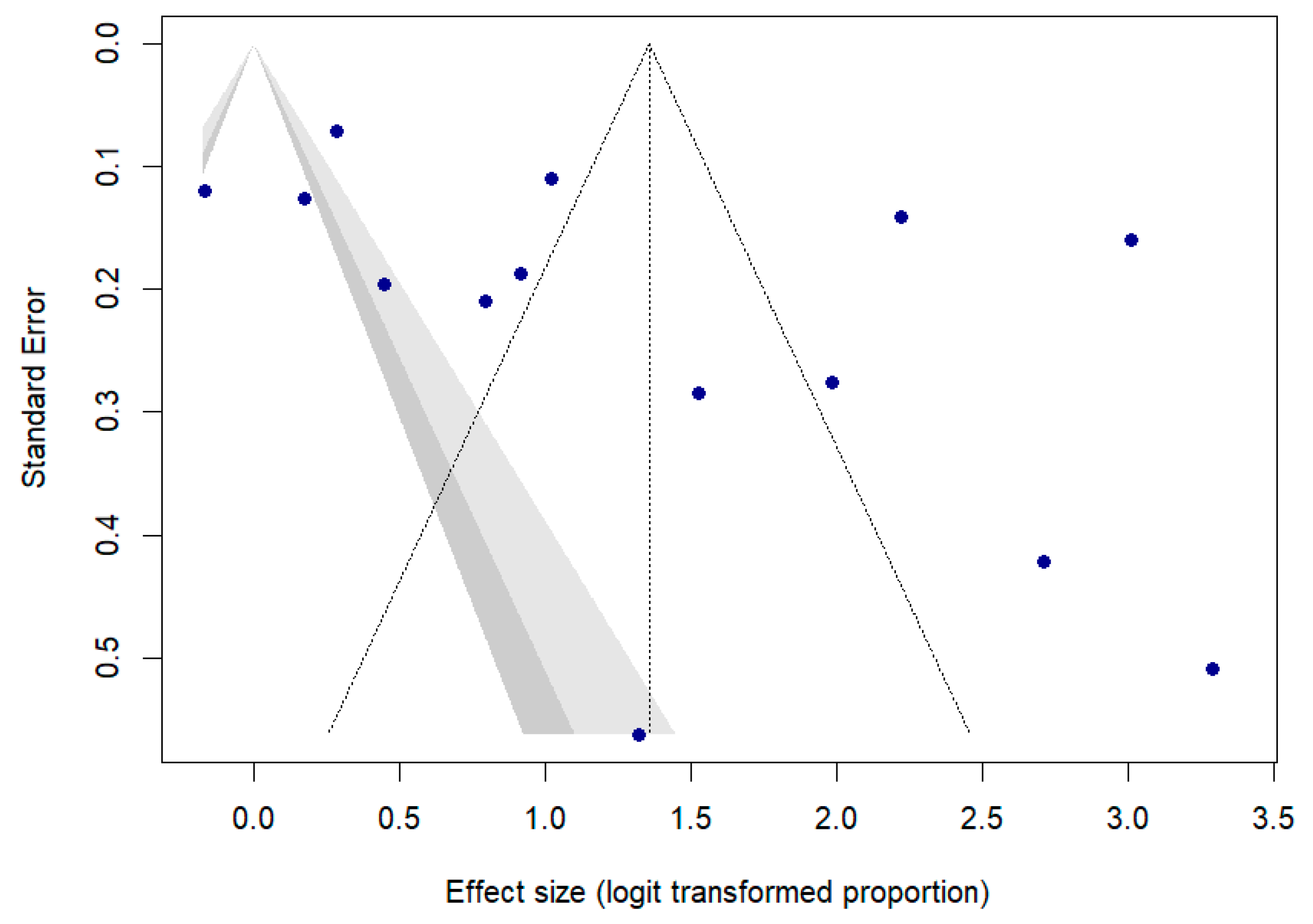
3.2.1. Incidence of RTW
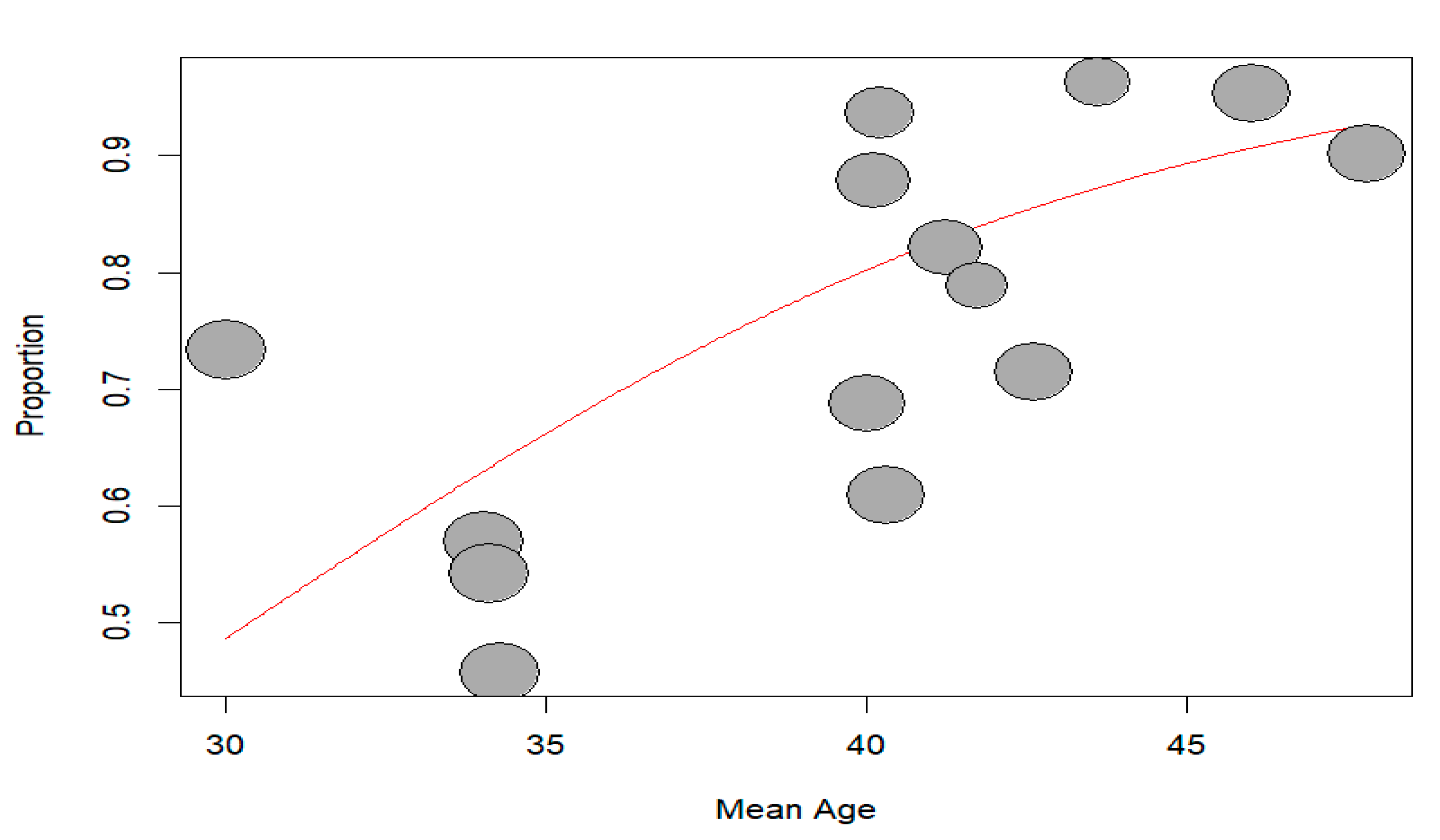
3.2.2. Meta-Regression
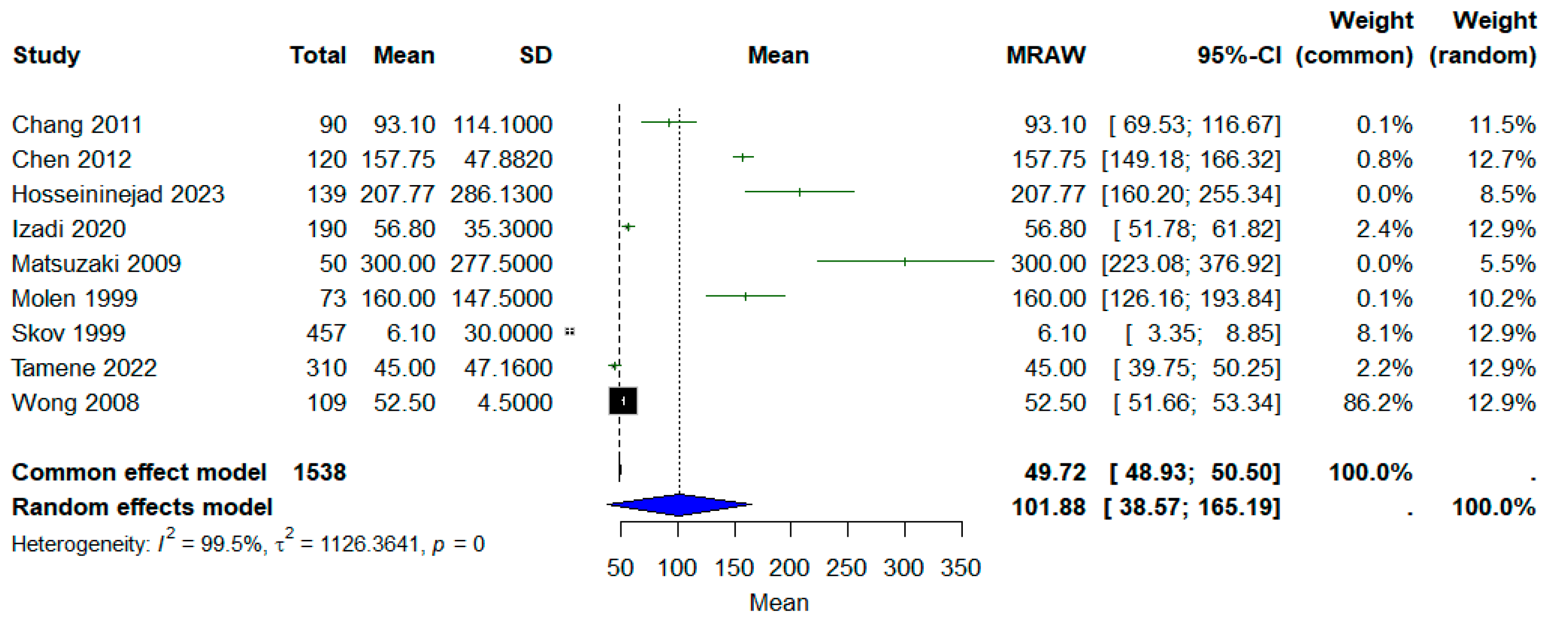
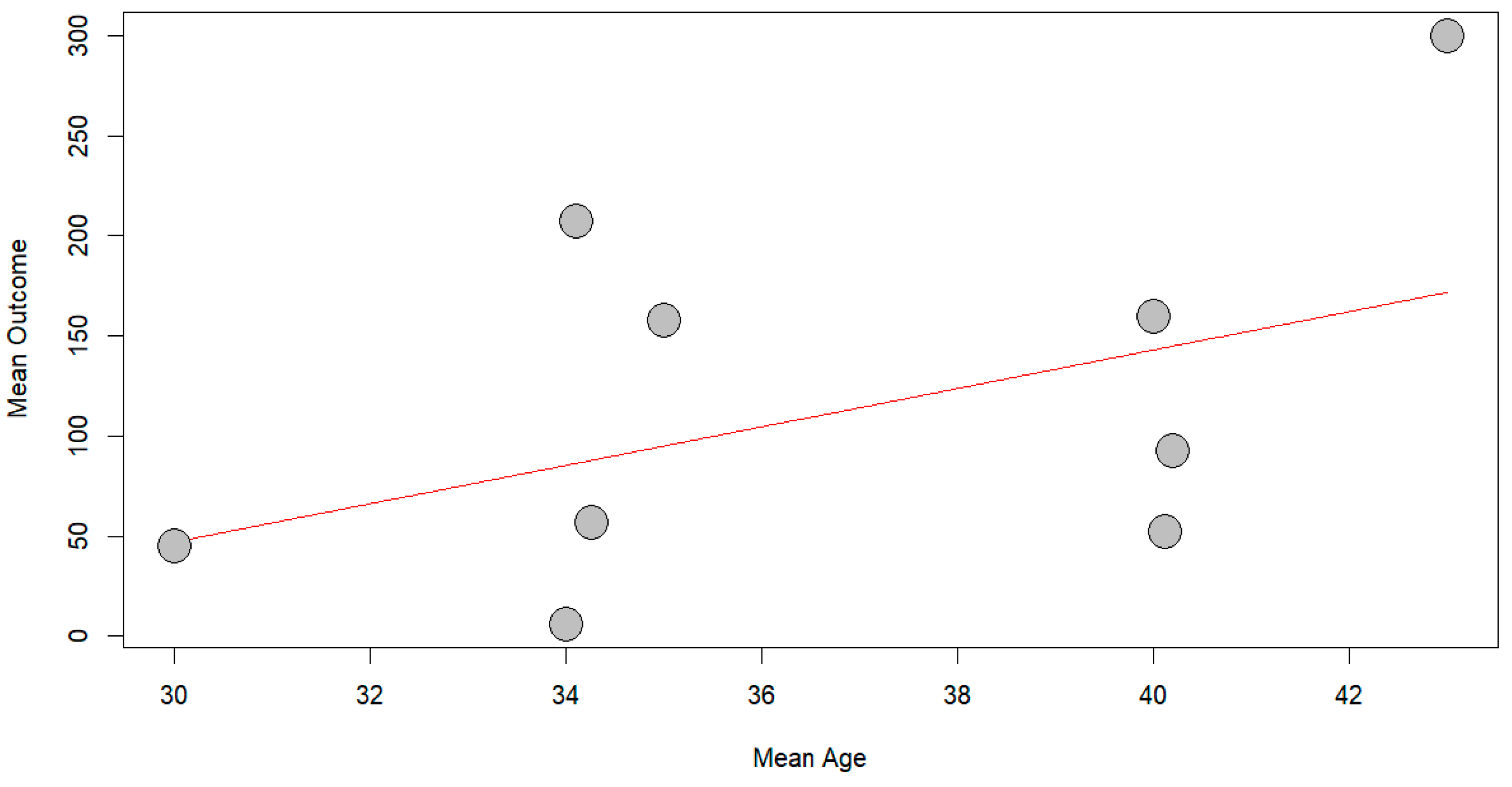
3.2.3. Time to Return to Work
3.2.4. Predictors of RTW
4. Discussion
4.1. Incidence and Timing of RTW
4.2. Influence of Age
4.3. Sex Differences
4.4. Marital Status and Education
4.5. Impact of Injury Type
4.6. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CI | Confidence Interval |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RTW | Return to Work |
References
- McMullin, B.; Fraser, J.; Robinson, B.; French, J.; Adisesh, A. Work-related injuries and attendance at a Canadian regional emergency department. Occup. Med. 2023, 73, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Takala, J.; Hämäläinen, P.; Sauni, R.; Nygård, C.H.; Gagliardi, D.; Neupane, S. Global-, regional-and country-level estimates of the work-related burden of diseases and accidents in 2019. Scand. J. Work Environ. Health 2024, 50, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Debela, M.B.; Azage, M.; Begosaw, A.M. Prevalence of Occupational Injury among Workers in the Construction, Manufacturing, and Mining Industries in Africa: A Systematic Review and Meta-analysis. J. Occup. Health Epidemiol. 2021, 10, 113–126. [Google Scholar] [CrossRef]
- Abdalla, S.; Apramian, S.S.; Cantley, L.F.; Cullen, M.R. Occupation and Risk for Injuries, 3rd ed.; Mock, C.N., Nugent, R., Kobusingye, O., Smith, K., Eds.; The International Bank for Reconstruction and Development: Washington, DC, USA, 2017. [Google Scholar]
- Ronconi, L.; Anchorena, J.; Paz, J. The incidence and severe consequences of occupational injuries among informal workers in a developing country. Int. J. Occup. Saf. Ergon. 2025, 31, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Salminen, S. Have young workers more injuries than older ones? An international literature review. J. Saf. Res. 2004, 35, 513–521. [Google Scholar] [CrossRef]
- Khorshidi, H.A.; Marembo, M.; Aickelin, U. Predictors of Return to Work for Occupational Rehabilitation Users in Work-Related Injury Insurance Claims: Insights from Mental Health. J. Occup. Rehabil. 2019, 29, 740–753. [Google Scholar] [CrossRef]
- Skov, O.; Jeune, B.; Lauritsen, J.M.; Barfred, T. Time Off Work After Occupational Hand Injuries. J. Hand Surg. Br. Eur. Vol. 1999, 24, 187–189. [Google Scholar] [CrossRef]
- Tamene, A.; Habte, A.; Derilo, H.T.; Endale, F.; Gizachew, A.; Sulamo, D.; Afework, A. Time to Return to Work After an Occupational Injury and Its Prognostic factors Among Employees of Large-Scale Metal Manufacturing Facilities in Ethiopia: A Retrospective Cohort. Environ. Health Insights 2022, 16, 11786302221109372. [Google Scholar] [CrossRef]
- Kalski, L.; Völkel, L.; Häußler, S.; Wolfarth, B.; Jacobs, K.; Soer, R. Efficacy of occupational rehabilitation in return to work for back pain: A systematic literature review. Work 2023, 78, 29–43. [Google Scholar] [CrossRef]
- Williams, R.M.; Westmorland, M.G.; Lin, C.A.; Schmuck, G.; Creen, M. Effectiveness of workplace rehabilitation interventions in the treatment of work-related low back pain: A systematic review. Disabil. Rehabil. 2007, 29, 607–624. [Google Scholar] [CrossRef]
- Grabe, E.M. Gradual Return to Work: Maximizing Benefits to Corporations and Their Caregiver Employees. J. Corp Law 2012, 37, 699. [Google Scholar]
- Flynn, S.; Ghent, A.C.; Nair, V. Determinants and Consequences of Return to Office Policies. SSRN Electron. J. 2024. Available online: https://api.semanticscholar.org/CorpusID:269102390 (accessed on 13 June 2025).
- Maas, E.T.; Koehoorn, M.; McLeod, C.B. Does gradually returning to work improve time to sustainable work after a work-acquired musculoskeletal disorder in British Columbia, Canada? A matched cohort effectiveness study. Occup. Environ. Med. 2021, 78, 715. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.P.; Garcia, A.; Hilfiker, R.; Léger, B.; Luthi, F. Systematic Review of Biopsychosocial Prognostic Factors for Return to Work After Acute Orthopedic Trauma: A 2020 Update. Front. Rehabil. Sci. 2022, 2, 791351. [Google Scholar] [CrossRef] [PubMed]
- Cullen, K.L.; Irvin, E.; Collie, A.; Clay, F.; Gensby, U.; Jennings, P.A.; Hogg-Johnson, S.; Kristman, V.; Laberge, M.; McKenzie, D.; et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: An update of the evidence and messages for practitioners. J. Occup. Rehabil. 2018, 28, 1–15. [Google Scholar] [CrossRef]
- Cancelliere, C.; Donovan, J.; Stochkendahl, M.J.; Biscardi, M.; Ammendolia, C.; Myburgh, C.; Cassidy, J.D. Factors affecting return to work after injury or illness: Best evidence synthesis of systematic reviews. Chiropr. Man. Ther. 2016, 24, 32. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hosseininejad, M.; Javadifar, S.; Mohammadi, S.; Mirzamohammadi, E. Assessment of the relationship between the return to work and the severity of work-related upper limb injuries using the whole person impairment. Chin. J. Traumatol. 2023, 26, 77–82. [Google Scholar] [CrossRef]
- Chen, Y.H.; Lin, H.T.; Chao, Y.H.; Lin, C.H.; Wei, F.C.; Lien, S.H. Self-perceived health and return to work following work-related hand injury. Occup. Med. 2012, 62, 295–297. [Google Scholar] [CrossRef]
- Chang, J.-H.; Wu, M.; Lee, C.-L.; Guo, Y.-L.; Chiu, H.-Y. Correlation of return to work outcomes and hand impairment measures among workers with traumatic hand injury. J. Occup. Rehabil. 2011, 21, 9–16. [Google Scholar] [CrossRef]
- Mink Van Der Molen, A.B.; Matloub, H.S.; Dzwierzynski, W.; Sanger, J.R. The Hand Injury Severity Scoring System and Workers’ Compensation Cases in Wisconsin, USA. J. Hand Surg. 1999, 24, 184–186. [Google Scholar] [CrossRef]
- Wong, J.Y.P. Time Off Work in Hand Injury Patients. J. Hand Surg. 2008, 33, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, H.; Narisawa, H.; Miwa, H.; Toishi, S. Predicting Functional Recovery and Return to Work After Mutilating Hand Injuries: Usefulness of Campbell’s Hand Injury Severity Score. J. Hand Surg. 2009, 34, 880–885. [Google Scholar] [CrossRef] [PubMed]
- Journeay, W.S.; Pauley, T.; Kowgier, M.; Devlin, M. Return to work after occupational and non-occupational lower extremity amputation. Occup. Med. 2018, 68, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.L.; Yin, Y.R.; Chu, C.M.; Tang, P.L. Does category of strength predict return-to-work after occupational injury? BMC Public Health 2022, 22, 1472. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Chang, J.H.; Shieh, S.J.; Lee, Y.C.; Kuo, L.C.; Lee, Y.L. Association between the initial anatomical severity and opportunity of return to work in occupational hand injured patients. J. Trauma 2010, 69, E88–E93. [Google Scholar] [CrossRef]
- von Schroeder, H.P.; Xue, C.; Yak, A.; Gandhi, R. Factors associated with unsuccessful return-to-work following work-related upper extremity injury. Occup. Med. 2020, 70, 434–438. [Google Scholar] [CrossRef]
- Üstün, G.G.; Küçük, K.Y.; Sert, G.; Kara, M.; Uzun, H. Factors Influencing the Time to Return to Work After Occupational Hand Injuries. Acta Med. 2022, 53, 362–366. [Google Scholar] [CrossRef]
- Izadi, N.; Jamshidi, S.; Mehrdad, R.; Nasibi, E. Predictors of return to work in patients with occupational hand injury. Hand Surg. Rehabil. 2020, 39, 218–222. [Google Scholar] [CrossRef]
- Chu, P.-C.; Chin, W.-S.; Guo, Y.L.; Shiao, J.S.-C. Long-term effects of psychological symptoms after occupational injury on return to work: A 6-year follow-up. Int. J. Environ. Res. Public Health 2019, 16, 235. [Google Scholar] [CrossRef]
- Du, C.-L.; Lai, C.-F.; Wang, J.-D. Delayed Return-to-work in Workers After Non-severe Occupational Upper Extremity Fracture in Taiwan. J. Formos. Med. Assoc. 2007, 106, 887–893. [Google Scholar] [CrossRef]
- Shi, Q.; Sinden, K.; MacDermid, J.C.; Walton, D.; Grewal, R. A systematic review of prognostic factors for return to work following work-related traumatic hand injury. J. Hand Ther. 2014, 27, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Bloom, B.; Thomas, S.; Ahrensberg, J.M.; Weaver, R.; Fowler, A.; Bestwick, J.; Harris, T.; Pearse, R. A systematic review and meta-analysis of return to work after mild Traumatic brain injury. Brain Inj. 2018, 32, 1623–1636. [Google Scholar] [CrossRef] [PubMed]
- Ottiger, M.; Poppele, I.; Sperling, N.; Schlesinger, T.; Müller, K. Work ability and return-to-work of patients with post-COVID-19: A systematic review and meta-analysis. BMC Public Health 2024, 24, 1811. [Google Scholar] [CrossRef] [PubMed]
- Beemster, T.T.; van Bennekom, C.A.M.; van Velzen, J.M.; Frings-Dresen, M.H.W.; Reneman, M.F. Vocational rehabilitation with or without work module for patients with chronic musculoskeletal pain and sick leave from work: Longitudinal impact on work participation. J. Occup. Rehabil. 2021, 31, 72–83. [Google Scholar] [CrossRef]
- Pransky, G.S.; Benjamin, K.L.; Savageau, J.A.; Currivan, D.; Fletcher, K. Outcomes in work-related injuries: A comparison of older and younger workers. Am. J. Ind. Med. 2005, 47, 104–112. [Google Scholar] [CrossRef]
- Savitsky, B.; Radomislensky, I.; Goldman, S.; Gitelson, N.; Frid, Z.; Peleg, K. Socio-economic disparities and returning to work following an injury. Isr. J. Health Policy Res. 2020, 9, 35. [Google Scholar] [CrossRef]
- Etuknwa, A.; Daniels, K.; Eib, C. Sustainable Return to Work: A Systematic Review Focusing on Personal and Social Factors. J. Occup. Rehabil. 2019, 29, 679–700. [Google Scholar] [CrossRef]
- De Rijk, A.; Nijhuis, F.; Alexanderson, K. Gender Differences in Work Modifications and Changed Job Characteristics During the Return-To-Work Process: A Prospective Cohort Study. J. Occup. Rehabil. 2009, 19, 185–193. [Google Scholar] [CrossRef]
- Panisoara, G.; Serban, M. Marital Status and Work-Life Balance. Procedia Soc. Behav. Sci. 2013, 78, 21–25. [Google Scholar] [CrossRef]
- Skagseth, M.; Fimland, M.; Rise, M.; Nilsen, T.; Aasdahl, L. Return-to-work self-efficacy after occupational rehabilitation for musculoskeletal and common mental health disorders: Secondary outcomes of a randomized clinical trial. J. Rehabil. Med. 2021, 53, jrm00146. [Google Scholar] [CrossRef]
- Matos, J.; Henriques, A.; Moura, A.; Alves, E. Professional reintegration of stroke survivors and their mental health, quality of life and community integration. Qual. Life Res. 2024, 33, 3259–3273. [Google Scholar] [CrossRef]
- Brenneman, F.D.; Redelmeier, D.A.; Boulanger, B.R.; McLellan, B.A.; Culhane, J.P. Long-term Outcomes in Blunt Trauma: Who Goes Back to Work? J. Trauma Acute Care Surg. 1997, 42, 778–781. [Google Scholar] [CrossRef]
| Study ID | Study Design | Country | Injury Site | Treatment | Period of Data Collection | Age Means (SD) | Sex M/F |
|---|---|---|---|---|---|---|---|
| Skov et al., 1999 [8] | Retrospective cohort | Denmark | Hand injury | Surgical, clinical, and rehabilitation | - | ||
| Tamene et al., 2022 [9] | Retrospective cohort | Ethiopia | Spine (29.6%), the upper limbs (34.1%), head and neck (21.1%), and the lower limbs (15.2%). | Surgical, clinical, and rehabilitation | Between 1 January 2017, and 31 December 2021 | 30 (4.5) | 398/24 |
| Hosseininejad et al., 2023 [19] | Retrospective cohort | Iran | Upper limb injuries | Physiotherapy and prosthesis use | March 2011 to December 2018 | 34.10 ± 9.04 | 245/11 |
| Chen et al., 2012 [20] | Prospective cohort | Taiwan | Hand injury | Surgical, clinical, and rehabilitation | - | 35 (6.7) | 92/28 |
| Chang et al., 2011 [21] | Retrospective cohort | Taiwan | Traumatic hand injury | - | From 2003 to 2006 | 40.2 (12.5) | 80/16 |
| Molen et al., 1999 [22] | Prospective cohort | USA | Hand injury | - | - | - | - |
| Wong, 2008 [23] | Prospective cohort | China | Hand Injury | Surgical reconstruction | - | 40 (12) | 100/24 |
| Matsuzaki, 2009 [24] | Retrospective cohort | Japan | Hand Injury | Surgical, clinical, and rehabilitation | Between October 1990 and August 2003 | 43 (18–69) | 40/10 |
| Journeay et al., 2018 [25] | Retrospective cohort | Canada | Lower extremity | Surgical amputation | - | 41.7 (15) | 19/0 |
| Yang et al., 2022 [26] | Retrospective Cohort | Taiwan | The upper limbs (61.9%), the lower limbs (13.1%), others (25%) | - | September 2016 and December 2018 | 41.24 ± 12.33 | 54/30 |
| Lee et al., 2010 [27] | Retrospective cohort | Taiwan | Hand injury | Surgical, clinical, and rehabilitation | Between September and November 2008 | 42.6 (12.9) | 99/41 |
| Schroeder et al., 2020 [28] | Retrospective cohort | Canada | Upper limb injuries | Physiotherapy, pain treatment, surgery, psychological treatment | Between April 2011 and September 2015 | 46 (11) | 570/298 |
| Üstün et al., 2022 [29] | Retrospective cohort | Turkey | Hand injury | Surgical, clinical, and rehabilitation | Between April 2020 and October 2021 | 43.6 | 99/12 |
| Izadi et al., 2020 [30] | Prospective cohort | Iran | Hand injury | - | Between July 2017 and February 2018 | 34.26 (9.67) | 271/8 |
| Chu et al., 2019 [31] | Prospective cohort | Taiwan | - | Physiotherapy, pain treatment, pharmacist assessment, surgery, psychology | Between 1 February and 31 August 2009. | 47.8 (11.1) | 386/186 |
| Du et al., 2007 [32] | Retrospective cohort | Taiwan | Upper limb injuries | Surgical, clinical, and rehabilitation | 16 August to 15 October 2003 | 40.3 ± 9.8 | 91/19 |
| Study | Population Defined | Exposure Measured | Outcome Measured | Confounding Controlled | Follow-Up Adequate | Overall Rating |
|---|---|---|---|---|---|---|
| Skov et al., 1999 [8] | Yes | Yes | Yes | No | Yes | High |
| Tamene et al., 2022 [9] | Yes | Yes | Yes | Yes | Yes | High |
| Hosseininejad et al., 2023 [19] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Chen et al., 2012 [20] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Chang et al., 2011 [21] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Molen et al., 1999 [22] | Yes | Yes | Yes | No | No | Low |
| Wong, 2008 [23] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Matsuzaki, 2009 [24] | Yes | Yes | Yes | Yes | Yes | High |
| Journeay et al., 2018 [25] | Yes | Yes | Yes | Yes | Yes | High |
| Yang et al., 2022 [26] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Lee et al., 2010 [27] | Yes | Yes | Yes | Yes | Yes | High |
| Schroeder et al., 2020 [28] | Yes | Yes | Yes | Yes | Yes | High |
| Üstün et al., 2022 [29] | Yes | Yes | Yes | Yes | Yes | High |
| Izadi et al., 2020 [30] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Chu et al., 2019 [31] | Yes | Yes | Yes | Yes | Yes | Moderate |
| Du et al., 2007 [32] | Yes | Yes | Yes | No | No | Low |
| Predictor | Comparison | Included Studies | Risk Ratio (RR) | 95% Confidence Interval | p-Value | I2 (%) | Model | Interpretation |
|---|---|---|---|---|---|---|---|---|
| Sex | Male vs. Female | Chang et al., 2011 [21], Du et al., 2007 [32], Hosseininejad et al., 2023 [19], Izadi et al., 2020 [30], Lee et al., 2010 [27], Schroeder et al., 2020 [28], Tamene, 2022 [9], and Yang et al., 2022 [26] | 6.12 | 2.33–16.06 | <0.0001 | 95.8 | Random-effects | Males had significantly higher RTW rates. |
| Sex subgrouping | Subgroup: Before 2015 | Chang et al., 2011 [21], Du et al., 2007 [32], and Lee et al., 2010 [27] | 4.25 | 1.38–13.05 | 0.0193 | 74.7 | Random-effects | Moderate heterogeneity in older studies, with no change in the context of results |
| Subgroup: 2015 and after | Hosseininejad et al., 2023 [19], Izadi et al., 2020 [30], Schroeder et al., 2020 [28], Tamene, 2022 [9], and Yang et al., 2022 [26] | 7.95 | 1.29–49.00 | <0.0001 | 97.2 | Random-effects | Very high heterogeneity in recent studies, with no change in the context of results | |
| Subgroup difference test | — | — | 0.3750 | — | — | No statistically significant subgroup difference (χ2 = 0.79, df = 1) | ||
| Marital Status | Married vs. Single | Hosseininejad et al., 2023 [19], Du et al., 2007 [32], Lee et al., 2010 [27], and Yang et al., 2022 [26] | 0.43 | 0.18–1.02 | <0.0001 | 88.3 | Random-effects | Married workers showed higher RTW |
| Marital Status (SA *) | Married vs. Single (SA) | Sensitivity analysis excluding Hosseininejad et al. [19] | 0.55 | 0.30–1.01 | 0.1563 | 46.1% | Random-effects | There was no difference between the two groups in terms of RTW incidence. |
| Education | >Grade 12 vs. ≤Grade 12 | Hosseininejad et al., 2023 [19], Tamene, 2022 [9], Lee et al., 2010 [27], and Yang et al., 2022 [26] | 0.54 | 0.34–0.87 | 0.0033 | 78.1 | Random-effects | Higher education is linked to more RTW. |
| Education (SA *) | >Grade 12 vs. ≤Grade 12 | Sensitivity analysis excluding Tamene et al. [9] | 0.47 | 0.29–0.77 | 0.2562 | 26.6 | Random-effects | There was no difference between the two groups in terms of RTW incidence. |
| Injury | Laceration vs. Crushing | Üstün et al., 2022 [29], Du et al., 2007 [32], and Wong, 2008 [23] | 1.89 | 0.11–33.74 | <0.0001 | 91.6 | Random-effects | Workers with lacerations had higher RTW |
| Injury (SA *) | Laceration vs. Crushing | Sensitivity analysis excluding Du et al. [32] | 3.99 | 0.20–80.10 | 0.2667 | 19.3 | Random-effects | There was no difference between the two groups in terms of RTW incidence. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, W.; Rojas, C.; Isidoro, R.; Lorente, A.; Dias, A.; Mariscal, G.; Zabady, A.H.; Lorente, R. Return to Work After Work-Related Injuries: A Systematic Review and Meta-Analysis of Incidence and Determinants. J. Clin. Med. 2025, 14, 4343. https://doi.org/10.3390/jcm14124343
Santos W, Rojas C, Isidoro R, Lorente A, Dias A, Mariscal G, Zabady AH, Lorente R. Return to Work After Work-Related Injuries: A Systematic Review and Meta-Analysis of Incidence and Determinants. Journal of Clinical Medicine. 2025; 14(12):4343. https://doi.org/10.3390/jcm14124343
Chicago/Turabian StyleSantos, Weiner, Carmen Rojas, Rui Isidoro, Alejandro Lorente, Ana Dias, Gonzalo Mariscal, Ahmed Hamdy Zabady, and Rafael Lorente. 2025. "Return to Work After Work-Related Injuries: A Systematic Review and Meta-Analysis of Incidence and Determinants" Journal of Clinical Medicine 14, no. 12: 4343. https://doi.org/10.3390/jcm14124343
APA StyleSantos, W., Rojas, C., Isidoro, R., Lorente, A., Dias, A., Mariscal, G., Zabady, A. H., & Lorente, R. (2025). Return to Work After Work-Related Injuries: A Systematic Review and Meta-Analysis of Incidence and Determinants. Journal of Clinical Medicine, 14(12), 4343. https://doi.org/10.3390/jcm14124343








