Ischemic Heart Disease, Hematological Malignancies, and Infectious Diseases as Risk Factors for Cervical Cancer: A Study Based on Korean National Health Insurance Data
Abstract
1. Introduction
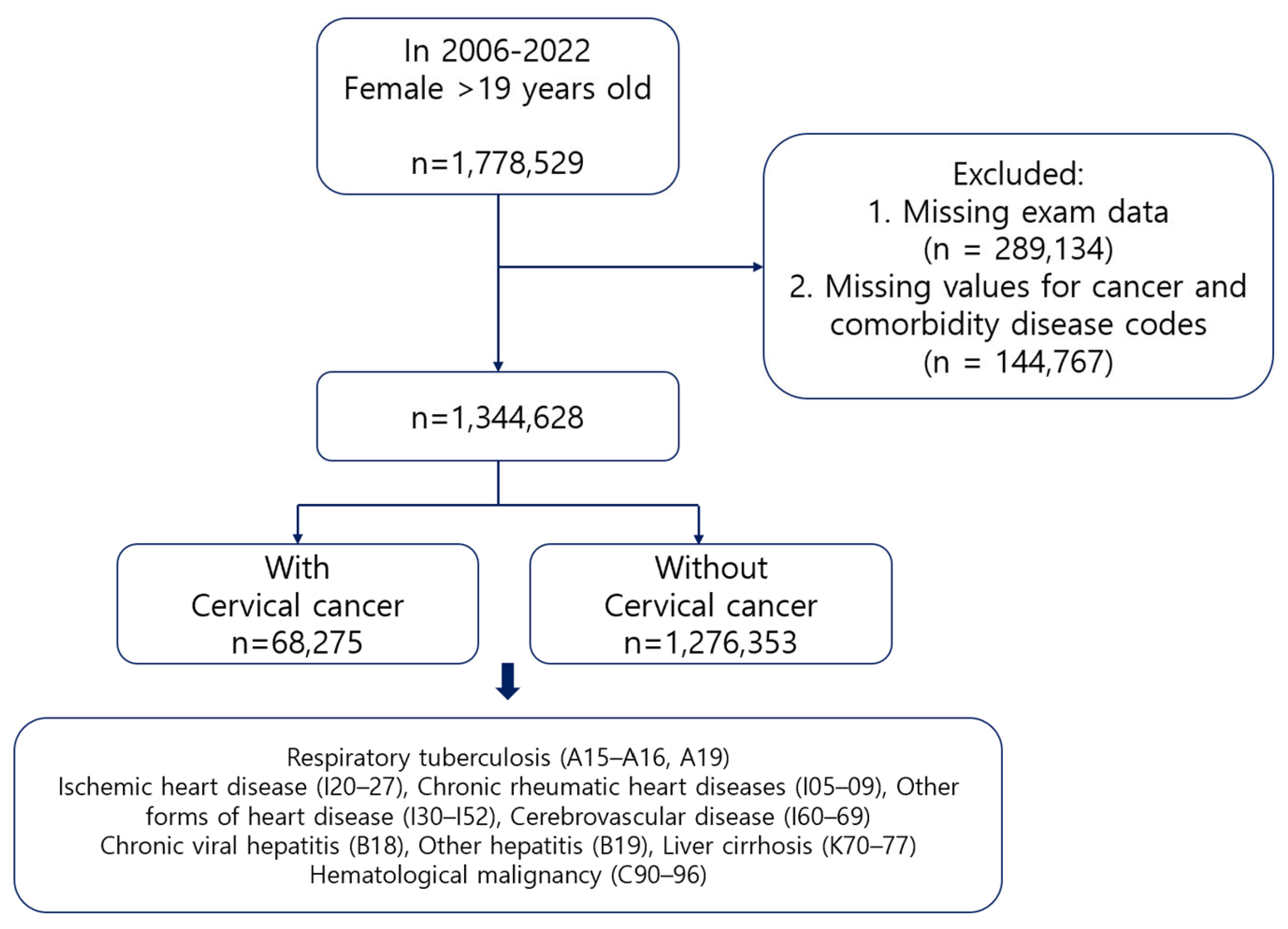
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Statistical Analysis
2.4. Ethics Statements
3. Results
3.1. Participant Characteristics
3.2. Prevalence of Underlying Diseases in the Study Groups
3.3. RR of Cervical Cancer Based on Underlying Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HPV | human papillomavirus |
| HIV | human immunodeficiency virus |
| NHIS | National Health Insurance |
| CIs | confidence intervals |
| vs. | versus |
| RR | relative risk |
| CI | confidence interval |
| OR | odds ratio |
| HBV | hepatitis B virus |
| HBsAg | hepatitis B surface antigen |
| HCV | hepatitis C virus |
| HCT | hematopoietic stem cell transplantation |
| BMI | body mass index |
| BP | blood pressure |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.J.; Jung, K.W.; Bang, S.H.; Choi, S.H.; Park, E.H.; Yun, E.H.; Kim, H.J.; Kong, H.J.; Im, J.S.; Seo, H.G. Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2020. Cancer Res. Treat. 2023, 55, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Georgieva, S.; Iordanov, V.; Sergieva, S. Nature of cervical cancer and other HPV—Associated cancers. J. BUON 2009, 14, 391–398. [Google Scholar] [PubMed]
- Rositch, A.F.; Koshiol, J.; Hudgens, M.G.; Razzaghi, H.; Backes, D.M.; Pimenta, J.M.; Franco, E.L.; Poole, C.; Smith, J.S. Patterns of persistent genital human papillomavirus infection among women worldwide: A literature review and meta-analysis. Int. J. Cancer 2013, 133, 1271–1285. [Google Scholar] [CrossRef]
- Choi, Y.J.; Park, J.S. Clinical significance of human papillomavirus genotyping. J. Gynecol. Oncol. 2016, 27, e21. [Google Scholar] [CrossRef]
- Stanley, M. Pathology and epidemiology of HPV infection in females. Gynecol. Oncol. 2010, 117, S5–S10. [Google Scholar] [CrossRef]
- Looker, K.J.; Rönn, M.M.; Brock, P.M.; Brisson, M.; Drolet, M.; Mayaud, P.; Boily, M.C. Evidence of synergistic relationships between HIV and human papillomavirus (HPV): Systematic reviews and meta-analyses of longitudinal studies of HPV acquisition and clearance by HIV status, and of HIV acquisition by HPV status. J. Int. AIDS Soc. 2018, 21, e25110. [Google Scholar] [CrossRef]
- Park, S.; Park, J.W.; Pitot, H.C.; Lambert, P.F. Loss of dependence on continued expression of the human papillomavirus 16 E7 oncogene in cervical cancers and precancerous lesions arising in fanconi anemia pathway-deficient mice. mBio 2016, 7, e00628-16. [Google Scholar] [CrossRef]
- Winer, R.L.; Lee, S.K.; Hughes, J.P.; Adam, D.E.; Kiviat, N.B.; Koutsky, L.A. Genital human papillomavirus infection: Incidence and risk factors in a cohort of female university students. Am. J. Epidemiol. 2003, 157, 218–226. [Google Scholar] [CrossRef]
- Roura, E.; Castellsagué, X.; Pawlita, M.; Travier, N.; Waterboer, T.; Margall, N.; Bosch, F.X.; de Sanjosé, S.; Dillner, J.; Gram, I.T.; et al. Smoking as a major risk factor for cervical cancer and pre-cancer: Results from the EPIC cohort. Int. J. Cancer 2014, 135, 453–466. [Google Scholar] [CrossRef]
- Palefsky, J.M.; Holly, E.A. Immunosuppression and co-infection with HIV. J. Natl. Cancer Inst. Monogr. 2003, 31, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Castle, P.E.; Einstein, M.H.; Sahasrabuddhe, V.V. Cervical cancer prevention and control in women living with human immunodeficiency virus. CA Cancer J. Clin. 2021, 71, 505–526. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cervical Cancer Elimination Initiative. Available online: https://www.who.int/initiatives/cervical-cancer-elimination-initiative (accessed on 2 May 2025).
- Chen, G.L.; Guo, L.; Yang, S.; Ji, D.M. Cancer risk in tuberculosis patients in a high endemic area. BMC Cancer 2021, 21, 679. [Google Scholar] [CrossRef] [PubMed]
- Everatt, R.; Kuzmickiene, I.; Davidaviciene, E.; Cicenas, S. Non-pulmonary cancer risk following tuberculosis: A nationwide retrospective cohort study in Lithuania. Infect. Agent Cancer 2017, 12, 33. [Google Scholar] [CrossRef]
- Manickam, A.; Sivanandham, M. Mycobacterium bovis BCG and purified protein derivative-induced reduction in the CD80 expression and the antigen up-take function of dendritic cells from patients with cervical cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 159, 413–417. [Google Scholar] [CrossRef]
- Min, Y.; Wei, X.; Xia, X.; Wei, Z.; Li, R.; Jin, J.; Liu, Z.; Hu, X.; Peng, X. Hepatitis B virus infection: An insight into the clinical connection and molecular interaction between hepatitis B virus and host extrahepatic cancer risk. Front. Immunol. 2023, 14, 1141956. [Google Scholar] [CrossRef]
- An, J.; Kim, J.W.; Shim, J.H.; Han, S.; Yu, C.S.; Choe, J.; Lee, D.; Kim, K.M.; Lim, Y.S.; Chung, Y.H.; et al. Chronic hepatitis B infection and non-hepatocellular cancers: A hospital registry-based, case-control study. PLoS ONE 2018, 13, e0193232. [Google Scholar] [CrossRef]
- Lu, T.; Yang, Q.; Li, M.; Zhang, J.; Zou, J.; Huang, L.; Lin, J.; Jin, H.; He, J. HBV infection and extra-hepatic cancers in adolescents and 20s: A retrospective study in China. Cancer Epidemiol. 2018, 55, 149–155. [Google Scholar] [CrossRef]
- Luo, C.; Yu, S.; Zhang, J.; Wu, X.; Dou, Z.; Li, Z.; Yang, E.; Zhang, L. Hepatitis B or C viral infection and the risk of cervical cancer. Infect. Agent Cancer 2022, 17, 54. [Google Scholar] [CrossRef]
- Bomfim-Hyppólito, S.; Eleuterio, J., Jr.; Nunes, G.C.; Bomfim-Hyppólito, E.; Franco, E.S.; Neto, R.J.P. HIV or human papillomavirus co-infection among Brazilian individuals infected with hepatitis B and/or hepatitis C. Int. J. Gynecol. Obstet. 2013, 122, 258–260. [Google Scholar] [CrossRef]
- Cheong, H.S.; Chang, Y.; Kim, Y.; Kwon, M.J.; Cho, Y.; Kim, B.; Joo, E.J.; Bae, Y.H.; Kim, C.; Ryu, S. Human papillomavirus infection and cardiovascular mortality: A cohort study. Eur. Heart J. 2024, 45, 1072–1082. [Google Scholar] [CrossRef] [PubMed]
- Mazibrada, J.; Rittà, M.; Mondini, M.; De Andrea, M.; Azzimonti, B.; Borgogna, C.; Ciotti, M.; Orlando, A.; Surico, N.; Chiusa, L.; et al. Interaction between inflammation and angiogenesis during different stages of cervical carcinogenesis. Gynecol. Oncol. 2008, 108, 112–120. [Google Scholar] [CrossRef]
- Bravo, I.G.; Crusius, K.; Alonso, A. The E5 protein of the human papillomavirus type 16 modulates composition and dynamics of membrane lipids in keratinocytes. Arch. Virol. 2005, 150, 231–246. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Kostev, K. Cancer risk in stroke survivors followed for up to 10 years in general practices in Germany. J. Cancer Res. Clin. Oncol. 2019, 145, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Jung, W.; Kim, S.Y.; Park, J.H.; Shin, D.W. The Korea National Disability Registration System. Epidemiol. Health 2023, 45, e2023053. [Google Scholar] [CrossRef]
- Robledo-Resina, I.d.M.; Romero-Morales, C.; Martín-Casas, P.; Villafañe, J.H.; Abuín-Porras, V. Relationship between Female Sexual Dysfunction and Trunk Stability Post-Stroke: A Cross-Sectional Study. Medicina 2024, 60, 324. [Google Scholar] [CrossRef]
- Marijon, E.; Mirabel, M.; Celermajer, D.S.; Jouven, X. Rheumatic heart disease. Lancet 2012, 379, 953–964. [Google Scholar] [CrossRef]
- Inamoto, Y.; Shah, N.N.; Savani, B.N.; Shaw, B.E.; Abraham, A.A.; Ahmed, I.A.; Akpek, G.; Atsuta, Y.; Baker, K.S.; Basak, G.W.; et al. Secondary solid cancer screening following hematopoietic cell transplantation. Bone Marrow Transplant. 2015, 50, 1013–1023. [Google Scholar] [CrossRef]
- Savani, B.N.; Stratton, P.; Shenoy, A.; Kozanas, E.; Goodman, S.; Barrett, A.J. Increased risk of cervical dysplasia in long-term survivors of allogeneic stem cell transplantation—Implications for screening and HPV vaccination. Biol. Blood Marrow Transplant. 2008, 14, 1072–1075. [Google Scholar] [CrossRef]
- McNally, G.A. HIV and cancer: An overview of AIDS-defining and non-AIDS-defining cancers in patients with HIV. Clin. J. Oncol. Nurs. 2019, 23, 327–331. [Google Scholar] [CrossRef]
- Liebenberg, L.J.P.; McKinnon, L.R.; Yende-Zuma, N.; Garrett, N.; Baxter, C.; Kharsany, A.B.M.; Archary, D.; Rositch, A.; Samsunder, N.; Mansoor, L.E.; et al. HPV infection and the genital cytokine milieu in women at high risk of HIV acquisition. Nat. Commun. 2019, 10, 5227. [Google Scholar] [CrossRef]
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef]
| Cervical Cancer (Mean ± SD) | General Population (Mean ± SD) | p-Value | |
|---|---|---|---|
| Age (years) | 52.45 (13.55) | 57.78 (13.05) | <0.001 |
| BMI (kg/m2) | 23.49 (3.55) | 23.21 (3.51) | <0.001 |
| Systolic BP (mmHg) | 120.9 (16.28) | 119.3 (15.71) | <0.001 |
| Diastolic BP (mmHg) | 74.95 (10.37) | 74.11 (10.22) | <0.001 |
| Hypertension a | <0.001 | ||
| Yes | 531,260 (41.62%) | 21,407 (31.35%) | |
| No | 745,093 (58.38%) | 46,868 (68.65%) | |
| Diabetes mellitus b | <0.001 | ||
| Yes | 17,034 (24.95%) | 531,944 (41.68%) | |
| No | 51,241 (75.05%) | 744,409 (58.32%) | |
| Smoking c | <0.001 | ||
| Yes | 120,697 (9.46%) | 7414 (10.86%) | |
| No | 1,155,656 (90.54%) | 60,861 (89.14%) | |
| Hemoglobin level (g/dL) | 12.84 (1.30) | 12.85 (1.26) | 0.0052 |
| Total cholesterol level (mg/dL) | 197.5 (40.57) | 195.6 (39.30) | 0.0245 |
| Underlying Disease a | Cervical Cancer, n (%) | General Population, n (%) |
|---|---|---|
| Respiratory tuberculosis (A15–16, A19) | 2549 (6.77%) | 54,939 (5.36%) |
| Disease of the circulating system | ||
| - Ischemic heart disease (I20–27) | 18,300 (6.39%) | 39,188 (5.30%) |
| - Chronic rheumatic heart diseases (I05-09) | 960 (6.57%) | 56,528 (5.39%) |
| - Other forms of heart disease (I30–I52) | 18,461 (6.51%) | 39,027 (5.26%) |
| - Cerebrovascular disease (I60–69) | 7088 (2.65%) | 61,187 (5.68%) |
| Disease of the liver | ||
| - Chronic viral hepatitis (B18) | 9321 (6.77%) | 48,167 (5.43%) |
| - Other hepatitis (B19) | 1063 (5.62%) | 56,425 (5.61%) |
| - Liver cirrhosis (K70–77) | 5219 (5.66%) | 52,269 (5.60%) |
| Hematological malignancy (C90–96) | 57,179 (5.60) | 309 (8.86) |
| Underlying Disease a | Univariate RR (95% CI) | p-Value | Multivariate RR (95% CI) b | p-Value |
|---|---|---|---|---|
| Respiratory tuberculosis (A15–16, A19) | 1.22 (1.17–1.26) | <0.001 | 1.32 (1.27–1.38) | <0.001 |
| Disease of the circulating system | ||||
| - Ischemic heart disease (I20–27) | 1.21 (1.18–1.22) | <0.001 | 1.72 (1.69–1.76) | <0.001 |
| - Chronic rheumatic heart diseases (I05–09) | 1.17 (1.10–1.25) | <0.001 | 1.53 (1.44–1.64) | <0.001 |
| - Other forms of heart disease (I30–I52) | 1.24 (1.22–1.26) | <0.001 | 1.60 (1.57–1.63) | <0.001 |
| - Cerebrovascular disease (I60–69) | 0.47 (0.46–0.48) | <0.001 | 0.58 (0.57–0.60) | <0.001 |
| Disease of the liver | ||||
| - Chronic viral hepatitis (B18) | 1.25 (1.22–1.28) | <0.001 | 1.33 (1.31–1.36) | <0.001 |
| - Other hepatitis (B19) | 1.00 (0.94–1.06) | 0.961 | 1.10 (1.03–1.17) | 0.0025 |
| - Liver cirrhosis (K70–77) | 0.99 (0.96–1.02) | 0.46 | 1.07 (1.04–1.10) | <0.001 |
| Hematological malignancy (C90–96) | 1.58 (1.42–1.76) | <0.001 | 1.87 (1.67–2.09) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, H.; Shin, M.; Seo, M.; Kim, Y.-W. Ischemic Heart Disease, Hematological Malignancies, and Infectious Diseases as Risk Factors for Cervical Cancer: A Study Based on Korean National Health Insurance Data. J. Clin. Med. 2025, 14, 4282. https://doi.org/10.3390/jcm14124282
Song H, Shin M, Seo M, Kim Y-W. Ischemic Heart Disease, Hematological Malignancies, and Infectious Diseases as Risk Factors for Cervical Cancer: A Study Based on Korean National Health Insurance Data. Journal of Clinical Medicine. 2025; 14(12):4282. https://doi.org/10.3390/jcm14124282
Chicago/Turabian StyleSong, Heekyoung, Mirae Shin, Minji Seo, and Yong-Wook Kim. 2025. "Ischemic Heart Disease, Hematological Malignancies, and Infectious Diseases as Risk Factors for Cervical Cancer: A Study Based on Korean National Health Insurance Data" Journal of Clinical Medicine 14, no. 12: 4282. https://doi.org/10.3390/jcm14124282
APA StyleSong, H., Shin, M., Seo, M., & Kim, Y.-W. (2025). Ischemic Heart Disease, Hematological Malignancies, and Infectious Diseases as Risk Factors for Cervical Cancer: A Study Based on Korean National Health Insurance Data. Journal of Clinical Medicine, 14(12), 4282. https://doi.org/10.3390/jcm14124282






