Influence of Sex on Therapeutic Adherence in Cardiovascular Diseases: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Data Sources and Search Strategy
2.3. Inclusion and Exclusion Criteria
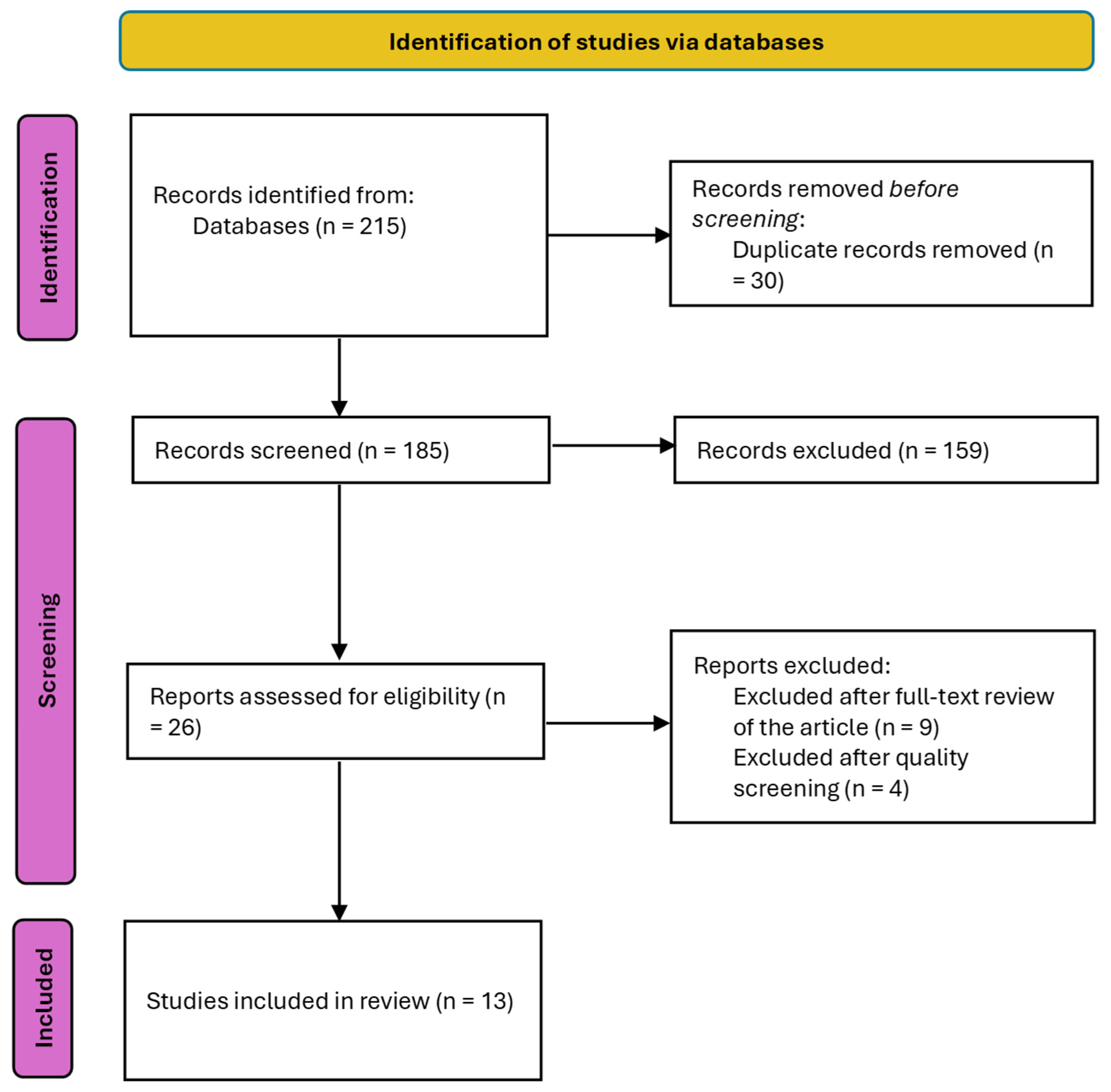
2.4. Selection Process
3. Results
3.1. Overview of Included Studies
3.2. Adherence to Pharmacological Treatment
3.3. Adherence to Lifestyle Modifications
3.4. Predictors of Poor Adherence
4. Discussion
4.1. Limitations
4.2. Implications for Research
4.3. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Cardiovascular Diseases (CVDs). Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 15 May 2025).
- Statistics on Deaths by Cause of Death. Year 2023. National Statistics Institute. Available online: https://www.ine.es/dyngs/Prensa/pEDCM2023.htm (accessed on 15 May 2025).
- Romeo, B.; Bergami, M.; Cenko, E.; Manfrini, O.; Bugiardini, R. Sex Disparities in Ischemic Heart Disease Mortality in Europe, 2005–2019: Data from GBD and Eurostat. JACC Adv. 2024, 3, 101252. [Google Scholar] [CrossRef] [PubMed]
- Humphries, K.; Izadnegahdar, M.; Sedlak, T.; Saw, J.; Johnston, N.; Schenck-Gustafsson, K.; Shah, R.; Regitz-Zagrosek, V.; Grewal, J.; Vaccarino, V.; et al. Sex differences in cardiovascular disease—Impact on care and outcomes. Front. Neuroendocr. 2017, 46, 46–70. [Google Scholar] [CrossRef]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Maas, A.H.E.M.; Appelman, Y.E.A. Gender differences in coronary heart disease. Neth. Heart J. 2010, 18, 598–603. [Google Scholar] [CrossRef]
- Reckelhoff, J.F. Gender differences in the regulation of blood pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef]
- Stramba-Badiale, M.; Fox, K.M.; Priori, S.G.; Collins, P.; Daly, C.; Graham, I.; Jonsson, B.; Schenck-Gustafsson, K.; Tendera, M. Cardiovascular diseases in women: A statement from the policy conference of the European Society of Cardiology. Eur. Heart J. 2006, 27, 994–1005. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.E.; Huxley, R.R.; Woodward, M. Diabetes as risk factor for incident coronary heart disease in women compared with men: A systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 2014, 57, 1542–1551. [Google Scholar] [CrossRef]
- Huxley, R.; Barzi, F.; Woodward, M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: Meta-analysis of 37 prospective cohort studies. BMJ 2006, 332, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Remsberg, K.E.; Demerath, E.W.; Schubert, C.M.; Chumlea, W.C.; Sun, S.S.; Siervogel, R.M. Early menarche and the development of cardiovascular disease risk factors in adolescent girls: The Fels Longitudinal Study. J. Clin. Endocrinol. Metab. 2005, 90, 2718–2724. [Google Scholar] [CrossRef]
- Wilson, P.W.F. Smoking, smoking cessation, and risk of cardiovascular disease. Curr. Treat Options Cardiovasc. Med. 2006, 8, 276–281. [Google Scholar] [CrossRef]
- McArthur, D.; Dumas, A.; Woodend, K.; Beach, S.; Stacey, D. Factors influencing adherence to regular exercise in middle-aged women: A qualitative study to inform clinical practice. BMC Womens Health 2014, 14, 49. [Google Scholar] [CrossRef]
- Britton, L.E.; Kaur, G.; Zork, N.; Marshall, C.J.; George, M. ‘We tend to prioritise others and forget ourselves’: How women’s caregiving responsibilities can facilitate or impede diabetes self-management. Diabet. Med. 2023, 40, e15030. [Google Scholar] [CrossRef]
- Cederlöf, E.T.; Lundgren, M.; Lindahl, B.; Christersson, C. Pregnancy Complications and Risk of Cardiovascular Disease Later in Life: A Nationwide Cohort Study. J. Am. Heart Assoc. 2022, 11, e023079. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.P.; Sun, B.; Catov, J.M.; Carnethon, M.; Lewis, C.E.; Allen, N.B.; Sidney, S.; Wellons, M.; Rana, J.S.; Hou, L.; et al. Gestational Diabetes History and Glucose Tolerance After Pregnancy Associated With Coronary Artery Calcium in Women During Midlife The CARDIA Study. Circulation 2021, 143, 974–987. [Google Scholar] [CrossRef]
- Mendelsohn, M.E.; Karas, R.H. The Protective Effects of Estrogen on the Cardiovascular System. N. Engl. J. Med. 1999, 340, 1801–1811. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.A.E.; Chlebowski, R.T.; Stefanick, M.L.; Aragaki, A.K.; Rossouw, J.E.; Prentice, R.L.; Anderson, G.; Howard, B.V.; Thomson, C.A.; LaCroix, A.Z.; et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the women’s health initiative randomized trials. JAMA 2013, 310, 1353–1368. [Google Scholar] [CrossRef] [PubMed]
- Colella, T.J.; Gravely, S.; Marzolini, S.; Grace, S.L.; Francis, J.A.; Oh, P.; Scott, L.B. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. Eur. J. Prev. Cardiol. 2015, 22, 423–441. [Google Scholar] [CrossRef]
- Arber, S.; Ginn, J. Gender and inequalities in health in later life. Soc. Sci. Med. 1993, 36, 33–46. [Google Scholar] [CrossRef]
- Healy, B. The Yentl syndrome. N. Engl. J. Med. 1991, 325, 274–276. [Google Scholar] [CrossRef]
- Smith, J.R.; Thomas, R.J.; Bonikowske, A.R.; Hammer, S.M.; Olson, T.P. Sex Differences in Cardiac Rehabilitation Outcomes. Circ. Res. 2022, 130, 552–565. [Google Scholar] [CrossRef]
- Aljofan, M.; Oshibayeva, A.; Moldaliyev, I.; Saruarov, Y.; Maulenkul, T.; Gaipov, A. The rate of medication nonadherence and influencing factors: A systematic Review. Electron. J. Gen. Med. 2023, 2023, 2516–3507. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization, 2003. Available online: https://iris.who.int/handle/10665/42682 (accessed on 9 June 2025).
- Venditti, V.; Bleve, E.; Morano, S.; Filardi, T. Gender-Related Factors in Medication Adherence for Metabolic and Cardiovascular Health. Metabolites 2023, 13, 1087. [Google Scholar] [CrossRef] [PubMed]
- Dean, Y.E.; Motawea, K.R.; Shebl, M.A.; Elawady, S.S.; Nuhu, K.; Abuzuaiter, B.; Awayda, K.; Fouad, A.M.; Tanas, Y.; Batista, R.; et al. Adherence to antihypertensives in the United States: A comparative meta-analysis of 23 million patients. J. Clin. Hypertens. 2024, 26, 303–313. [Google Scholar] [CrossRef] [PubMed]
- Kokenge, M.C.; Ruppar, T.M. Factors Influencing Antihypertensive Medication Adherence among Historically Underrepresented Adults: A Meta-analysis. J. Cardiovasc. Nurs. 2024, 39, 499–506. [Google Scholar] [CrossRef]
- Abegaz, T.M.; Shehab, A.; Gebreyohannes, E.A.; Bhagavathula, A.S.; Elnour, A.A. Nonadherence to antihypertensive drugs a systematic review and meta-analysis. Medicine 2017, 19, A657. [Google Scholar]
- Olmastroni, E.; Boccalari, M.T.; Tragni, E.; Rea, F.; Merlino, L.; Corrao, G.; Catapano, A.L.; Casula, M. Sex-differences in factors and outcomes associated with adherence to statin therapy in primary care: Need for customisation strategies. Pharmacol. Res. 2020, 155, 104514. [Google Scholar] [CrossRef]
- Lewey, J.; Shrank, W.H.; Bowry, A.D.K.; Kilabuk, E.; Brennan, T.A.; Choudhry, N.K. Gender and racial disparities in adherence to statin therapy: A meta-analysis. Am. Heart J. 2013, 165, 665–678.e1. [Google Scholar] [CrossRef]
- Oosenbrug, E.; Marinho, R.P.; Zhang, J.; Marzolini, S.; Colella, T.J.F.; Pakosh, M.; Grace, S.L. Sex Differences in Cardiac Rehabilitation Adherence: A Meta-analysis. Can. J. Cardiol. 2016, 32, 1316–1324. [Google Scholar] [CrossRef]
- Resurrección, D.M.; Moreno-Peral, P.; Gómez-Herranz, M.; Rubio-Valera, M.; Pastor, L.; de Almeida, J.M.C.; Motrico, E. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: A systematic review of prospective cohort studies. Eur. J. Cardiovasc. Nurs. 2019, 18, 38–47. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Antes, G.; Atkins, D.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 336–341. [Google Scholar] [CrossRef]
- Redcaspe—Critical Appraisal Skills Programme Español. Available online: https://redcaspe.org/ (accessed on 15 May 2025).
- Andualem, A.; Liknaw, T.; Edmealem, A.; Gedefaw, M. Adherence to antihypertensive medications among adult hypertensive patients attending chronic follow-up units of Dessie Referral Hospital, Northeastern Ethiopia: A cross-sectional study. Medicine 2021, 100, e26818. [Google Scholar] [CrossRef] [PubMed]
- Moreno, G.; Vicent, L.; Rosillo, N.; Delgado, J.; Cerro EPDel Bueno, H. Do sex and gender aspects influence non-adherence to secondary prevention measures after myocardial infarction? Am. J. Prev. Cardiol. 2024, 19, 100713. [Google Scholar] [CrossRef]
- Consolazio, D.; Gattoni, M.E.; Russo, A.G. Exploring gender differences in medication consumption and mortality in a cohort of hypertensive patients in Northern Italy. BMC Public Health 2022, 22, 768. [Google Scholar] [CrossRef]
- Goodwin, A.M.; Duran, A.T.; Kronish, I.M.; Moise, N.; Sanchez, G.J.; Garber, C.E.; Schwartz, J.E.; Diaz, K.M. Factors associated with objectively measured exercise participation after hospitalization for acute coronary syndrome. Int. J. Cardiol. 2019, 275, 1–5. [Google Scholar] [CrossRef]
- Hyun, K.; Negrone, A.; Redfern, J.; Atkins, E.; Chow, C.; Kilian, J.; Rajaratnam, R.; Brieger, D. Gender Difference in Secondary Prevention of Cardiovascular Disease and Outcomes Following the Survival of Acute Coronary Syndrome. Heart Lung Circ. 2021, 30, 121–127. [Google Scholar] [CrossRef]
- Peersen, K.; Otterstad, J.E.; Sverre, E.; Perk, J.; Gullestad, L.; Moum, T.; Dammen, T.; Munkhaugen, J. Medical and Psychosocial Factors Associated with Low Physical Activity and Increasing Exercise Level after a Coronary Event. J. Cardiopulm. Rehabil. Prev. 2020, 40, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Haung, Z.; Hong, S.A.; Tejativaddhana, P.; Puckpinyo, A.; Myint, M.N.H.A. Multiple self-care behaviors and associated factors in community-dwelling patients with hypertension in Myanmar. Nagoya J. Med. Sci. 2020, 82, 363–376. [Google Scholar]
- Wawruch, M.; Wimmer, G.; Murin, J.; Paduchova, M.; Tesar, T.; Hlinkova, L.; Slavkovsky, P.; Fabryova, L.; Aarnio, E. Patient-Associated Characteristics Influencing the Risk for Non-Persistence with Statins in Older Patients with Peripheral Arterial Disease. Drugs Aging 2019, 36, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Setny, M.; Jankowski, P.; Kaminski, K.; Gasior, Z.; Haberka, M.; Czarnecka, D.; Pająk, A.; Kozieł, P.; Szóstak-Janiak, K.; Sawicka, E.; et al. Secondary prevention of coronary heart disease in Poland: Does sex matter? Results from the POLASPIRE survey. Pol. Arch. Intern. Med. 2021, 132, 16179. [Google Scholar] [CrossRef]
- Mahtta, D.; Ahmed, S.T.; Ramsey, D.J.; Akeroyd, J.M.; Lee, M.T.; Rodriguez, F.; Michos, E.D.; Itchhaporia, D.; Nasir, K.; Alam, M.; et al. Statin Prescription Rates, Adherence, and Associated Clinical Outcomes Among Women with PAD and ICVD. Cardiovasc. Drugs Ther. 2020, 34, 745–754. [Google Scholar] [CrossRef]
- Højskov, I.E.; Thygesen, L.C.; Moons, P.; Egerod, I.; Olsen, P.S.; Berg, S.K. The challenge of non-adherence to early rehabilitation after coronary artery bypass surgery: Secondary results from the SheppHeartCABG trial. Eur. J. Cardiovasc. Nurs. 2020, 19, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Ritchey, M.D.; Maresh, S.; McNeely, J.; Shaffer, T.; Jackson, S.L.; Keteyian, S.J.; Brawner, C.A.; Whooley, M.A.; Chang, T.; Stolp, H.; et al. Tracking cardiac rehabilitation participation and completion among Medicare beneficiaries to inform the efforts of a national initiative. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e005902. [Google Scholar] [CrossRef]
- Rea, F.; Mella, M.; Monzio Compagnoni, M.; Cantarutti, A.; Merlino, L.; Mancia, G.; Corrao, G. Women discontinue antihypertensive drug therapy more than men. Evidence from an Italian population-based study. J. Hypertens. 2020, 38, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Aslam, A.; Stehli, J.; Kaye, D.; Layland, J.; Nicholls, S.J.; Cameron, J.; Zaman, S. Gender Differences in Healthy Lifestyle Adherence Following Percutaneous Coronary Intervention for Coronary Artery Disease. Heart Lung Circ. 2021, 30, e37–e40. [Google Scholar] [CrossRef]
- Khan, N.N.S.; Kelly-Blake, K.; Luo, Z.; Olomu, A. Sex Differences in Statin Prescribing in Diabetic and Heart Disease Patients in FQHCs: A Comparison of the ATPIII and 2013 ACC/AHA Cholesterol Guidelines. Health Serv. Res. Manag. Epidemiol. 2019, 6, 233339281882541. [Google Scholar] [CrossRef]
- Mehta, L.S.; Velarde, G.P.; Lewey, J.; Sharma, G.; Bond, R.M.; Navas-Acien, A.; Fretts, A.M.; Magwood, G.S.; Yang, E.; Blumenthal, R.S.; et al. Cardiovascular Disease Risk Factors in Women: The Impact of Race and Ethnicity: A Scientific Statement from the American Heart Association. Circulation 2023, 147, 1471–1487. [Google Scholar] [CrossRef] [PubMed]
- Bautista, L.E.; Vera-Cala, L.M.; Colombo, C.; Smith, P. Symptoms of depression and anxiety and adherence to antihypertensive medication. Am. J. Hypertens. 2012, 25, 505–511. [Google Scholar] [CrossRef]
- Marshall, I.J.; Wolfe, C.D.A.; McKevitt, C. Lay perspectives on hypertension and drug adherence: Systematic review of qualitative research. BMJ 2012, 345, e3953. [Google Scholar] [CrossRef]
- Resurrección, D.M.; Motrico, E.; Rigabert, A.; Rubio-Valera, M.; Conejo-Cerón, S.; Pastor, L.; Moreno-Peral, P. Barriers for Nonparticipation and Dropout of Women in Cardiac Rehabilitation Programs: A Systematic Review. J. Women’s Health 2017, 26, 849–859. [Google Scholar] [CrossRef]
- Mosca, L.; Barrett-Connor, E.; Kass Wenger, N. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation 2011, 124, 2145–2154. [Google Scholar] [CrossRef]
- Mosca, L.; Mochari-Greenberger, H.; Dolor, R.J.; Newby, L.K.; Robb, K.J. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.M.; King-Shier, K.M.; Duncan, A.; Spaling, M.; Stone, J.A.; Jaglal, S.; Angus, J. Factors influencing referral to cardiac rehabilitation and secondary prevention programs: A systematic review. Eur. J. Prev. Cardiol. 2013, 20, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Smolderen, K.G.; Strait, K.M.; Dreyer, R.P.; D’Onofrio, G.; Zhou, S.; Lichtman, J.H.; Geda, M.; Bueno, H.; Beltrame, J.; Safdar, B.; et al. Depressive symptoms in younger women and men with acute myocardial infarction: Insights from the VIRGO study. J. Am. Heart Assoc. 2015, 4, e001424. [Google Scholar] [CrossRef]
- Ferreruela, I.L.; Azuara, B.O.; Fumanal, S.M.; Hernández, M.J.R.; Aguilar-Palacio, I. Gender inequalities in secondary prevention of cardiovascular disease: A scoping review. Int. J. Equity Health 2024, 23, 146. [Google Scholar] [CrossRef]
- Vaccarino, V.; Sullivan, S.; Hammadah, M.; Wilmot, K.; Al Mheid, I.; Ramadan, R.; Elon, L.; Pimple, P.M.; Garcia, E.V.; Nye, J.; et al. Mental stress-induced-myocardial ischemia in young patients with recent myocardial infarction: Sex differences and mechanisms. Circulation 2018, 137, 794–805. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C.; Kirby, A.; Sourjina, T.; Peto, R.; Collins, R.; et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef]
- Lee, H.; Park, J.H.; Floyd, J.S.; Park, S.; Kim, H.C. Combined Effect of Income and Medication Adherence on Mortality in Newly Treated Hypertension: Nationwide Study of 16 Million Person-Years. J. Am. Heart Assoc. 2019, 8, e013148. [Google Scholar] [CrossRef]
| Database | Search with MeSH and Free Terms | Results |
|---|---|---|
| PUBMED | (“Sex Factors” [Mesh]) AND (“Patient Compliance” [Mesh] OR “Medication Adherence” [Mesh] OR “Treatment Adherence and Compliance” [Mesh]) AND (“Cardiovascular Diseases” [Mesh] OR “Arrhythmias, Cardiac” [Mesh] OR “Heart Valve Diseases” [Mesh] OR “Acute Coronary Syndrome” [Mesh] OR “Hypertension, Malignant” [Mesh] OR “Hypertension, Pulmonary” [Mesh] OR “Cardiomyopathies” [Mesh] OR “Heart Failure” [Mesh] OR “Pulmonary Embolism” [Mesh] OR “Pericarditis” [Mesh] OR “Endocarditis” [Mesh] OR “Aortic Diseases” [Mesh] OR “Peripheral Arterial Disease” [Mesh]) | 63 |
| WEB OF SCIENCE | TS=(“Health Status Disparities” OR “Sex Factors”) AND TS=(“Patient Compliance” OR “Treatment Adherence” OR “Medication Adherence” OR “Compliance” OR “Medication Continuation” OR “Adherence” OR “Therapeutic Compliance”) AND TS=(“Secondary Prevention” OR “Therapeutics”) AND ALL=(“Arrhythmias” OR “Cardiovascular diseases” OR “Heart Valve Diseases” OR “Acute Coronary Syndrome” OR “Chronic Coronary Syndrome” OR “Hypertension” OR “Pulmonary Hypertension” OR “Cardiomyopathies” OR “Heart Failure” OR “Pulmonary Embolism” OR “Pericardial Diseases” OR “Endocarditis” OR “Aortic Diseases” OR “Peripheral Arterial Disease”) | 41 |
| SCOPUS | TITLE-ABS-KEY (“Sex Factors”) AND TITLE-ABS-KEY (“Patient Compliance” OR “Treatment Adherence” OR “Medication Adherence” OR “Compliance” OR “Medication Continuation” OR “Adherence” OR “Therapeutic Compliance”) AND ALL (“Therapeutics” OR “Secondary Prevention”) AND ALL (“Arrhythmias” OR “Cardiovascular diseases” OR “Heart Valve Diseases” OR “Acute Coronary Syndrome” OR “Chronic Coronary Syndrome” OR “Hypertension” OR “Pulmonary Hypertension” OR “Cardiomyopathies” OR “Heart Failure” OR “Pulmonary Embolism” OR “Pericardial Diseases” OR “Endocarditis” OR “Aortic Diseases” OR “Peripheral Arterial Disease”) | 109 |
| Authors | Illness | Sample | Results/Sex | Predictors | |
|---|---|---|---|---|---|
| N | |||||
| Andualem et al. [35] | Hypertension | 366 | M = 122 | Medication adherence: 50.8% | Sex, unemployed occupational status, insufficient knowledge about the disease, poor self-efficacy |
| F = 244 | Medication adherence: 46.7% | ||||
| Moreno et al. [36] | Ischemic heart disease | 503 | M = 252 | M and F at 12 months:
| Overall: HF, peripheral artery disease, stroke, CKD, previous AMI, AF, DM, hypertension, hyperlipidemia, depression, active smoking, burden of family care. |
| F = 251 | |||||
| Consolazio et al. [37] | Hypertension | 232,507 | M = 128,808 | Medication adherence: 82.29% | M: Older age |
| F = 103,699 | Medication adherence: 80% | F: Younger age | |||
| Goodwin et al. [38] | Ischemic heart disease | 151 | M = 105 | Adherence to physical exercise: 68.6% | Overall, the predictors of non-exercise are: older age, female sex, Hispanic ethnicity, worse perceived physical health, higher burden of comorbidities, higher CVR, and history of HF |
| F = 46 | Adherence to physical exercise: 41.3% | ||||
| Hyun et al. [39] | Ischemic heart disease | 8761 | M = 6244 |
| Overall: Previous AMI, HF, stroke, peripheral artery disease, dyslipidemia, DM, hypertension, active smoking, and CKD |
| F = 2517 |
| ||||
| Peersen et al. [40] | Ischemic heart disease | 1101 | M = 872 | Adherence to physical activity: 42.7% | Overall: Smoking, low consumption of fruits and vegetables, obesity, depression, and low scores in the physical component of quality of life. Non-modifiable factors: Female sex, low educational level, AMI as an index event, and ≥1 previous coronary event. |
| F = 229 | Adherence to physical activity: 31.5% | ||||
| Haung et al. [41] | Hypertension | 410 | M = 96 |
| In general, in both sexes: being younger, living alone, less education, having a low family income, and residing in a rural area |
| F = 314 |
| ||||
| Wawruch et al. [42] | Peripheral artery disease | 8330 | M = 3433 | Medication adherence: 70.9% | In general, for both sexes: Patients starting atorvastatin or rosuvastatin therapy, being a new statin user, having hypercholesterolemia, depression, anxiety disorders, being female, receiving an increased co-pay (covered medications), and having a mild–moderate intensity of treatment |
| F = 4897 | Medication adherence: 59.6% | ||||
| Setny et al. [43] | Ischemic heart disease | 1236 | M = 882 |
| M: Active smoking and overweight. |
| F = 354 |
| F: Higher burden of risk factors (59% had 3 or more CVRF), central obesity, passive smoking in young females; almost twice as many of them had a reduced glomerular filtration rate and high anxiety. | |||
| Mahtta et al. [44] | Ischemic heart disease | 484,134 | M = 471,319 |
| M: Higher prevalence of hypertension, DM, ischemic heart disease, AMI |
| F = 12,815 |
| F: Higher levels of LDL and HDL, as well as higher burden of disease (which means a higher cost of medical care compared to males) | |||
| Hojskov et al. [45] | Ischemic heart disease | 152 | M = 132 |
| Of both sexes: obesity, diabetes and antidiabetic therapy, use of beta-blockers, lower educational level |
| F = 20 |
| ||||
| Ritchey et al. [46] | Ischemic heart disease | 366,103 | M = 207,911 |
| Adults 65–74 years old, dual eligible (receive financial aid) |
| F = 158,192 |
| ||||
| Rea et al. [47] | Hypertension | 60,529 | M = 30,860 |
| M: DM and respiratory diseases |
| F = 29,666 |
| F: Antidepressant use, cancer | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno, G.; Moreno-Ferreiro, B.; Pérez-Ingidua, C.; Vicente-Galán, M.J.; Gimeno-Hernán, V.; Orgaz-Rivas, E.; González-Sanavia, M.J.; Rivas-Paterna, A.B.; Pacheco del Cerro, E.; Meneses-Monroy, A. Influence of Sex on Therapeutic Adherence in Cardiovascular Diseases: A Scoping Review. J. Clin. Med. 2025, 14, 4253. https://doi.org/10.3390/jcm14124253
Moreno G, Moreno-Ferreiro B, Pérez-Ingidua C, Vicente-Galán MJ, Gimeno-Hernán V, Orgaz-Rivas E, González-Sanavia MJ, Rivas-Paterna AB, Pacheco del Cerro E, Meneses-Monroy A. Influence of Sex on Therapeutic Adherence in Cardiovascular Diseases: A Scoping Review. Journal of Clinical Medicine. 2025; 14(12):4253. https://doi.org/10.3390/jcm14124253
Chicago/Turabian StyleMoreno, Guillermo, Blanca Moreno-Ferreiro, Carla Pérez-Ingidua, María Jesús Vicente-Galán, Verónica Gimeno-Hernán, Elena Orgaz-Rivas, María José González-Sanavia, Ana Belén Rivas-Paterna, Enrique Pacheco del Cerro, and Alfonso Meneses-Monroy. 2025. "Influence of Sex on Therapeutic Adherence in Cardiovascular Diseases: A Scoping Review" Journal of Clinical Medicine 14, no. 12: 4253. https://doi.org/10.3390/jcm14124253
APA StyleMoreno, G., Moreno-Ferreiro, B., Pérez-Ingidua, C., Vicente-Galán, M. J., Gimeno-Hernán, V., Orgaz-Rivas, E., González-Sanavia, M. J., Rivas-Paterna, A. B., Pacheco del Cerro, E., & Meneses-Monroy, A. (2025). Influence of Sex on Therapeutic Adherence in Cardiovascular Diseases: A Scoping Review. Journal of Clinical Medicine, 14(12), 4253. https://doi.org/10.3390/jcm14124253






