Balance and Mobility in Comparison to Patient-Reported Outcomes—A Longitudinal Evaluation After Total Hip and Knee Arthroplasty
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Surgical Procedures and Rehabilitation Process
2.3. Clinical Assessments and Questionnaire
2.4. Statistical Analysis
3. Results
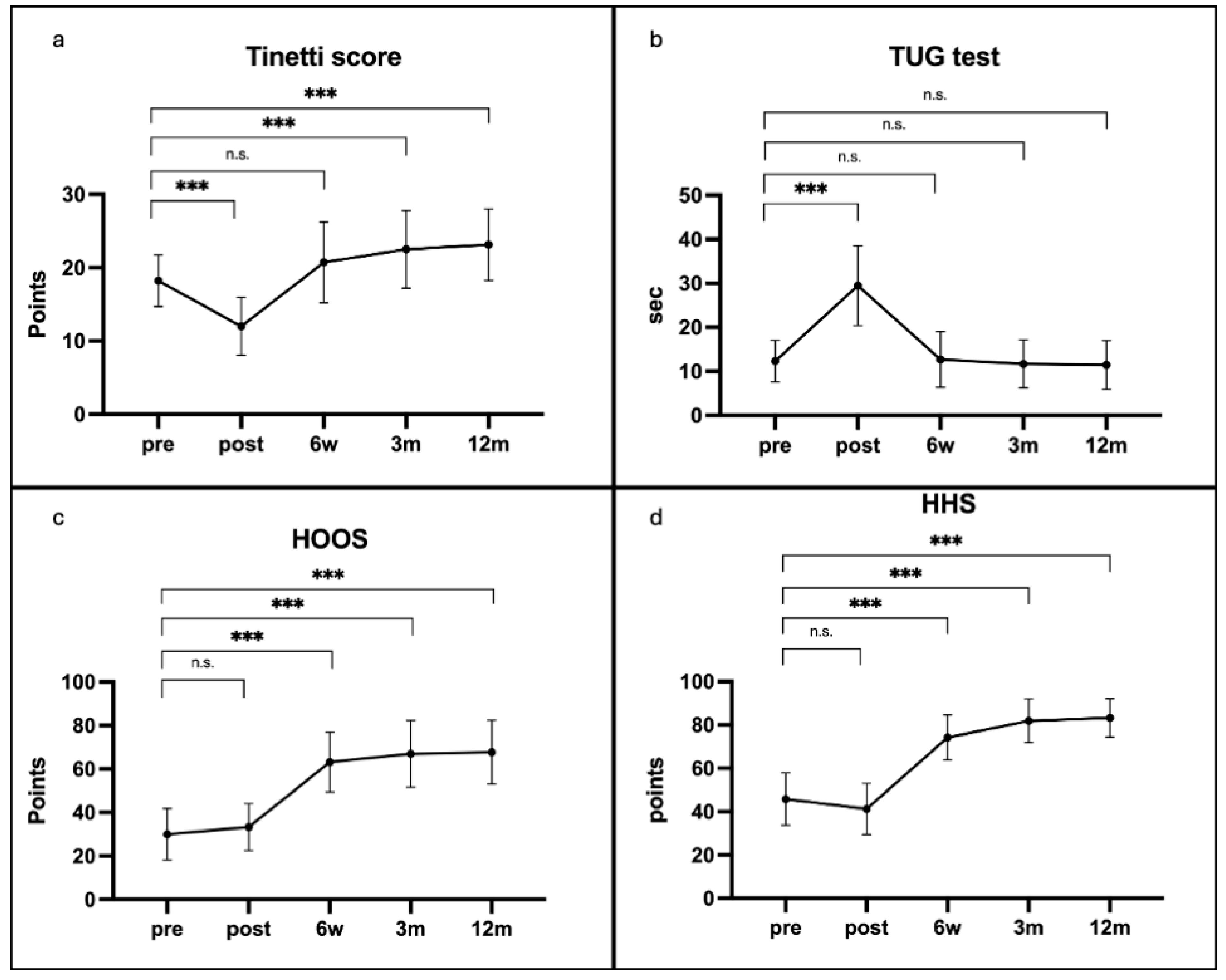
3.1. Functional Assessments and Patient-Reported Outcomes Following Total Hip Arthroplasty
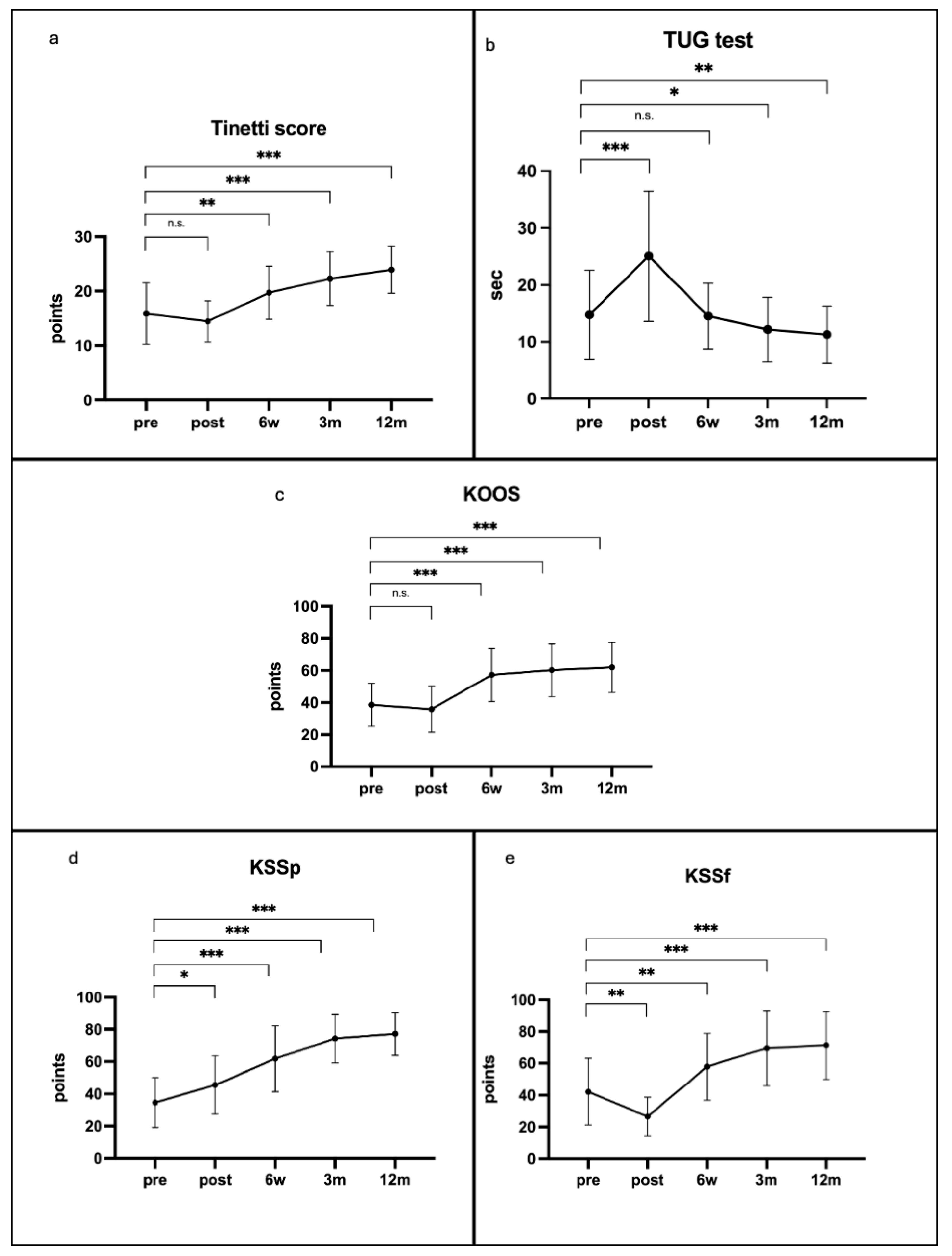
3.2. Functional Assessments and Patient-Reported Outcomes Following Total Knee Arthroplasty
3.3. Correlation of Functional Assessments and Patient-Reported Outcomes
3.4. Comparative Analysis of Outcomes Following Total Hip and Total Knee Arthroplasty
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HHS | Harris Hip Score |
| HOOS | Hip Disability and Osteoarthritis Outcome Score |
| KOOS | Knee Injury and Osteoarthritis Outcome Score |
| KSS | Knee Society Score |
| KSSf | Knee Society Score subscale for function |
| KSSp | Knee Society Score subscale for pain |
| n.s. | non-significant |
| POMA | Tinetti Performance-Oriented Mobility Assessment |
| PROMs | patient-reported outcome measures |
| SD | Standard deviation |
| THA | Total Hip Arthroplasty |
| TKA | Total Knee Arthroplasty |
| TUG | Timed Up and Go |
References
- Benedetti, M.G.; Di Martino, A.; Bonsanto, F.; Sommella, N.; Ciardulli, F.; Labanca, L. Balance and proprioception impairment, assessment tools, and rehabilitation training in patients with total hip arthroplasty: A systematic review. BMC Musculoskelet. Disord. 2021, 22, 1055. [Google Scholar] [CrossRef]
- Adamo, P.; Bolzoni, L.; Temporiti, F.; Gatti, R.; De Capitani, F.; Marino, G. Long-term gait analysis in patients after total knee arthroplasty: A systematic review and meta-analysis. Gait Posture 2024, 113, 75–98. [Google Scholar] [CrossRef]
- Yiannakopoulos, C.K.; Vlastos, I.; Kalinterakis, G.; Sachinis, N.P.; Gianzina, E.; Delis, S. Evaluation of gait recovery after total knee arthroplasty using wearable inertial sensors: A systematic review. Knee 2023, 41, 190–203. [Google Scholar] [CrossRef]
- Fukushima, K.; Uchiyama, K.; Takahira, N.; Takaso, M.; Matsunaga, A.; Fukuda, M.; Nanri, Y.; Shibuya, M.; Kamiya, K. The maximal gait speed is a simple and useful prognostic indicator for functional recovery after total hip arthroplasty. BMC Musculoskelet. Disord. 2020, 21, 84. [Google Scholar] [CrossRef]
- Eckardt, A.; Mündermann, A.; Nüesch, C.; Clauss, M.; Stoffel, K.; Pagenstert, G.; Kaufmann, M.; Ilchmann, T.; Ismailidis, P. Functional assessment of total hip arthroplasty using inertial measurement units: Improvement in gait kinematics and association with patient-reported outcome measures. J. Orthop. Res. 2022, 41, 759–770. [Google Scholar] [CrossRef]
- Imagama, S.; Matsui, Y.; Arai, H.; Mizuno, T.; Takemura, M.; Fukui, J.; Watanabe, T.; Ishizuka, S. Comparison of gait analysis before and after unilateral total knee arthroplasty for knee osteoarthritis. J. Orthop. Surg. Res. 2024, 19, 506. [Google Scholar] [CrossRef]
- Hable, R.; Dimitrov, D.; Ramadanov, N.; Marinova-Kichikova, P.; Becker, R.; Lazaru, P.; Liu, K.; Ostojic, M. Risk Factors and Predictors for Functional Outcome and Complication Rate in Total Hip Arthroplasty through Minimally Invasive and Conventional Approaches: A Systematic Review and Meta-Regression Analysis of 41 Randomized Controlled Trials. J. Clin. Med. 2023, 12, 5895. [Google Scholar] [CrossRef]
- Stevens, M.; Bulstra, S.K.; Reininga, I.H.F.; Boerboom, A.L.; Meijer, M.F. Does Imageless Computer-assisted TKA Lead to Improved Rotational Alignment or Fewer Outliers? A Systematic Review. Clin. Orthop. Relat. Res. 2014, 472, 3124–3133. [Google Scholar] [CrossRef]
- Karpiński, R.; Krakowski, P.; Wilczyński, M.; Bieniek, M. Cemented vs. Cementless Fixation in Primary Knee Replacement: A Narrative Review. Materials 2024, 17, 1136. [Google Scholar] [CrossRef]
- Ricci, M.; Magnan, B.; Vecchini, E.; Tromponi, C.; Giannini, N.; Lamberti, D.; Dall'Oca, C. Evolution of TKA design. Acta Biomed. 2017, 88, 17–31. [Google Scholar]
- Crawford, D.A.; Lombardi, A.V., Jr.; Berend, K.R.; Huddleston, J.I., III; Peters, C.L.; DeHaan, A.; Zimmerman, E.K.; Duwelius, P.J. Early outcomes of primary total hip arthroplasty with use of a smartphone-based care platform: A prospective randomized controlled trial. Bone Jt. J. 2021, 103-b (Suppl. B), 91. [Google Scholar] [CrossRef] [PubMed]
- Ohmori, T.; Kabata, T.; Kajino, Y.; Inoue, D.; Kato, S.; Tsuchiya, H. Contralateral Lower-Limb Functional Status Before Total Hip Arthroplasty: An Important Indicator for Postoperative Gait Speed. J. Bone Jt. Surg. Am. 2021, 103, 1093. [Google Scholar] [CrossRef] [PubMed]
- Takahira, N.; Kusaba, A.; Watanabe, H.; Kondo, S.; Sekita, J. Identifying Deficits in Hip and Knee Muscle Strength on the Surgical and Nonsurgical Sides in Women up to 12 Months After Total Hip Arthroplasty. Phys. Ther. 2024, 104, pzae099. [Google Scholar] [CrossRef]
- Somerville, L.; Lanting, B.; Hunter, S.W.; Omana, H.; Adebero, T. Effectiveness of prehabilitation on outcomes following total knee and hip arthroplasty for osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Disabil. Rehabil. 2024, 46, 5771–5790. [Google Scholar] [CrossRef]
- Smith, P.N.; Coulter, C.L.; Neeman, T.M.; Scarvell, J.M. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: A systematic review. J. Physiother. 2013, 59, 219–226. [Google Scholar] [CrossRef]
- Matheis, C.; Stöggl, T. Strength and mobilization training within the first week following total hip arthroplasty. J. Bodyw. Mov. Ther. 2018, 22, 519–527. [Google Scholar] [CrossRef]
- Richardson, S.; Podsiadlo, D. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Nijboer, H.; Delbaere, K.; Stevens, M.; Hoogland, J.; Annegarn, J.; Brodie, M.A.; Rispens, S.M.; Spina, G.; Saporito, S. Remote timed up and go evaluation from activities of daily living reveals changing mobility after surgery. Physiol. Meas. 2019, 40, 035004. [Google Scholar] [CrossRef]
- Nguyen, J.; Argento, G.; McInerney, D.; Wuest, O.; Guttenberg, M. Does the Timed-Up-and-Go Test Predict Length of Stay After Total Hip Arthroplasty? A Retrospective Study. HSS J. 2023, 20, 182–186. [Google Scholar] [CrossRef]
- Lee, B.-H.; An, J.; Son, Y.-W. Effect of Combined Kinematic Chain Exercise on Physical Function, Balance Ability, and Gait in Patients with Total Knee Arthroplasty: A Single-Blind Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 3524. [Google Scholar] [CrossRef]
- Kopke, S.; Meyer, G. The Tinetti test: Babylon in geriatric assessment. Z. Gerontol. Geriatr. 2006, 39, 288. [Google Scholar] [CrossRef] [PubMed]
- Scura, D.; Munakomi, S. Tinetti Gait and Balance Test. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Guo, C.; Li, S.; Jia, S.; Wang, J.; Wang, P.; Wang, X.; Si, Y. The prediction model of fall risk for the elderly based on gait analysis. BMC Public Health 2024, 24, 2206. [Google Scholar] [CrossRef]
- Aquino, J.-P.; Guize, L.; Manckoundia, P.; Buatois, S.; Jégo, B.; Thomas, F.; Benetos, A. Impact of clinical, psychological, and social factors on decreased Tinetti test score in community-living elderly subjects: A prospective study with two-year follow-up. BMC Public Health 2008, 14, CR316–CR322. [Google Scholar]
- Cipriany-Dacko, L.M.; Innerst, D.; Johannsen, J.; Rude, V. Interrater reliability of the tinetti balance scores in novice and experienced physical therapy clinicians. Arch. Phys. Med. Rehabil. 1997, 78, 1160–1164. [Google Scholar] [CrossRef]
- Tarihci Cakmak, E.; Yaliman, A.; Torna, G.; Sen, E.I. The effectiveness of bodyweight-supported treadmill training in stroke patients: Randomized controlled trial. Neurol. Sci. 2024, 45, 3277. [Google Scholar] [CrossRef]
- Raynaud-Simon, A.; Laurent, L.; Koskas, P.; Lilamand, M.; Sebbagh, M.; Lacaille, S.; Estrada, J. Tinetti balance performance is associated with mortality in older adults with late-onset Parkinson’s disease: A longitudinal study. BMC Geriatr. 2023, 23, 54. [Google Scholar] [CrossRef]
- Roos, E.M.; Lohmander, L.S. The Knee injury and Osteoarthritis Outcome Score (KOOS): From joint injury to osteoarthritis. Health Qual. Life Outcomes 2003, 1, 64. [Google Scholar] [CrossRef]
- Nilsdotter, A.K.; Roos, E.M.; Lohmander, L.S.; Klässbo, M. Hip disability and osteoarthritis outcome score (HOOS)–validity and responsiveness in total hip replacement. BMC Musculoskelet. Disord. 2003, 4, 10. [Google Scholar] [CrossRef]
- Felson, D.T.; Crossley, K.M.; Roos, E.M.; Collins, N.J.; Misra, D. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. 2011, 63 (Suppl. S11), S208–S228. [Google Scholar] [CrossRef]
- Smulders, K.; Busch, V.; Keijsers, N.; Geurts, A.; Smolders, J.; Boekesteijn, R. Objective monitoring of functional recovery after total knee and hip arthroplasty using sensor-derived gait measures. PeerJ 2022, 10, e14054. [Google Scholar] [CrossRef]
- Kahlenberg, C.A.; Cross, M.B.; Nwachukwu, B.U.; Schairer, W.W.; Steinhaus, M.E. Patient Satisfaction Reporting After Total Hip Arthroplasty: A Systematic Review. Orthopedics 2017, 40, e400–e404. [Google Scholar] [CrossRef] [PubMed]
- Canovas, F.; Dagneaux, L. Quality of life after total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2018, 104, S41–S46. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. S1), S31. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Rai, S.; Zhang, Q.; Hong, P.; Li, Y.; Chen, Y.; Li, J. Enhanced recovery after surgery in patients after hip and knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2023, 100, 159–173. [Google Scholar] [CrossRef]
- Haddad, F.S.; Ronca, F.; Kayani, B.; Magan, A.; Radhakrishnan, G.; Baawa-Ameyaw, J. Time for return to sport following total knee arthroplasty: A meta-analysis. Arch. Orthop. Trauma Surg. 2021, 142, 3427–3436. [Google Scholar] [CrossRef]
- Wu, J.-Q.; Mao, L.-B. Efficacy of exercise for improving functional outcomes for patients undergoing total hip arthroplasty: A meta-analysis. Medicine 2019, 98, e14591. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, Z.; Xin, W.; Li, A. Preoperative intravenous glucocorticoids can decrease acute pain and postoperative nausea and vomiting after total hip arthroplasty: A PRISMA-compliant meta-analysis. Medicine 2017, 96, e8804. [Google Scholar] [CrossRef]
- Hill, M.; Tichý, M.; Janatová, M.; Otáhal, J.; Krejčí, M.; Nechlebová, E.; Kajzar, J. Performance of Homebalance Test in an Assessment of Standing Balance in Elderly Adults. Physiol. Res. 2022, 71, 305–315. [Google Scholar] [CrossRef]
- Nagai, K.; Nakagawa, N.; Masuhara, K.; Tagomori, K.; Miura, N.; Ikutomo, H. Gait Abnormality Predicts Falls in Women After Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 3215–3219. [Google Scholar] [CrossRef]
- Nof, L.; Fulk, G.; Echternach, J.; Canbek, J. Test-Retest Reliability and Construct Validity of the Tinetti Performance-Oriented Mobility Assessment in People with Stroke. J. Neurol. Phys. Ther. 2013, 37, 14–19. [Google Scholar] [CrossRef]
- Rivolta, M.W.; Aktaruzzaman; Rizzo, G.; Lafortuna, C.L.; Ferrarin, M.; Bovi, G.; Bonardi, D.R.; Caspani, A.; Sassi, R. Evaluation of the Tinetti score and fall risk assessment via accelerometry-based movement analysis. Artif. Intell. Med. 2019, 95, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Smolen, J.S.; Radner, H.; Ernst, M.; Binder, A.; Stamm, T.; Köller, M.; Böhler, C. Rheumatoid arthritis and falls: The influence of disease activity. Rheumatology 2012, 51, 2051–2057. [Google Scholar] [CrossRef]
- Wallis, J.A.; Henderson, K.G.; Snowdon, D.A. Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: A systematic review and meta-analysis. Physiotherapy 2018, 104, 25–35. [Google Scholar] [CrossRef]
- Nelissen, R.G.H.H.; Vlieland, T.P.M.V.; Reijman, M.; Groot, L.; Onstenk, R.; Kaptein, B.L.; Kaptijn, H.H.; Vehmeijer, S.B.W.; Verdegaal, S.H.M.; Latijnhouwers, D.A.J.M.; et al. Recovery and the use of postoperative physical therapy after total hip or knee replacement. BMC Musculoskelet. Disord. 2022, 23, 666. [Google Scholar] [CrossRef]
- Richards, J.A.; Williams, M.D.; Gupta, N.A.; Kitchen, J.M.; Whitaker, J.E.; Smith, L.S.; Malkani, A.L. No difference in PROMs between robotic-assisted CR versus PS total knee arthroplasty: A preliminary study. J. Robot. Surg. 2022, 16, 1209–1217. [Google Scholar] [CrossRef]
- Riddle, D.L.; Patel, N.K.; Goldman, A.H.; Abraham, V.M.; Reiter, C.R. Patient reported outcome measures (PROMs) as primary and secondary outcomes in total hip and knee arthroplasty randomized controlled trials: A systematic review. Arch. Orthop. Trauma Surg. 2024, 144, 2257–2266. [Google Scholar] [CrossRef]
- Dervin, G.; Wood, K.; Au, K.; Beaulé, P.E.; Poitras, S. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: Are both performance and comorbidity measures useful? Int. Orthop. 2018, 42, 2295–2300. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, H.; Si, Y.; Shen, H.; Liu, J.; Lu, L.; Zhang, H.; Zhang, S.; Yu, D.; Luo, X.; et al. A Prospective Randomized Controlled Trial Assessing the Impact of Preoperative Combined with Postoperative Progressive Resistance Training on Muscle Strength, Gait, Balance and Function in Patients Undergoing Total Hip Arthroplasty. Clin. Interv. Aging 2024, 19, 745–760. [Google Scholar] [CrossRef]


| THA | TKA | THA vs. TKA | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | p-Value | Mean | SD | p-Value | p-Value | ||
| Tinetti | preop | 18.23 | (3.52) | 15.90 | (5.66) | n.s. | ||
| postop | 12.00 | (3.94) | *** | 14.48 | (3.78) | n.s. | n.s. | |
| 6 weeks | 20.73 | (5.52) | n.s. | 19.71 | (4.87) | ** | n.s. | |
| 3 months | 22.50 | (5.29) | *** | 22.33 | (4.94) | *** | n.s. | |
| 12 months | 23.14 | (4.89) | *** | 23.95 | (4.34) | *** | n.s. | |
| TUG | preop | 12.31 | (4.70) | 14.77 | (7.81) | n.s. | ||
| postop | 29.46 | (9.08) | *** | 25.07 | (11.45) | *** | n.s. | |
| 6 weeks | 12.71 | (6.34) | n.s. | 14.53 | (5.83) | n.s. | n.s. | |
| 3 months | 11.70 | (5.42) | n.s. | 12.21 | (5.65) | * | n.s. | |
| 12 months | 11.47 | (5.50) | n.s. | 11.30 | (4.97) | ** | n.s. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vertesich, K.; Staats, K.; Schneider, E.; Willegger, M.; Windhager, R.; Böhler, C. Balance and Mobility in Comparison to Patient-Reported Outcomes—A Longitudinal Evaluation After Total Hip and Knee Arthroplasty. J. Clin. Med. 2025, 14, 4135. https://doi.org/10.3390/jcm14124135
Vertesich K, Staats K, Schneider E, Willegger M, Windhager R, Böhler C. Balance and Mobility in Comparison to Patient-Reported Outcomes—A Longitudinal Evaluation After Total Hip and Knee Arthroplasty. Journal of Clinical Medicine. 2025; 14(12):4135. https://doi.org/10.3390/jcm14124135
Chicago/Turabian StyleVertesich, Klemens, Kevin Staats, Eleonora Schneider, Madeleine Willegger, Reinhard Windhager, and Christoph Böhler. 2025. "Balance and Mobility in Comparison to Patient-Reported Outcomes—A Longitudinal Evaluation After Total Hip and Knee Arthroplasty" Journal of Clinical Medicine 14, no. 12: 4135. https://doi.org/10.3390/jcm14124135
APA StyleVertesich, K., Staats, K., Schneider, E., Willegger, M., Windhager, R., & Böhler, C. (2025). Balance and Mobility in Comparison to Patient-Reported Outcomes—A Longitudinal Evaluation After Total Hip and Knee Arthroplasty. Journal of Clinical Medicine, 14(12), 4135. https://doi.org/10.3390/jcm14124135







