Use of Digital and Telemedicine Tools for Postoperative Pain Management at Home: A Scoping Review of Health Professionals’ Roles and Clinical Outcomes
Abstract
1. Introduction
2. Materials and Methods
- -
- What digital or telemedicine tools are used for managing postoperative pain at home?
- -
- What is the role of healthcare professionals?
- -
- What clinical outcomes result from the use of these interventions?
2.1. Databases Used and Search Strategy
2.2. Data Extraction
2.3. Study Selection
- -
- Addressed the use of digital or telemedicine tools for managing pain at home after surgical procedures;
- -
- Involved healthcare professionals in home monitoring and intervention processes;
- -
- Reported clinical outcomes resulting from the use of such tools, including data related to pain or treatment adherence;
- -
- Were published in English and dated between 2015 and 2025.
- -
- Did not focus on postoperative pain in patients;
- -
- Did not involve home monitoring;
- -
- Did not describe digital tools or telemedicine used in the interventions.
2.4. Screening Process
2.5. Quality Assessment and Risk of Bias
2.6. Data Synthesis
3. Results
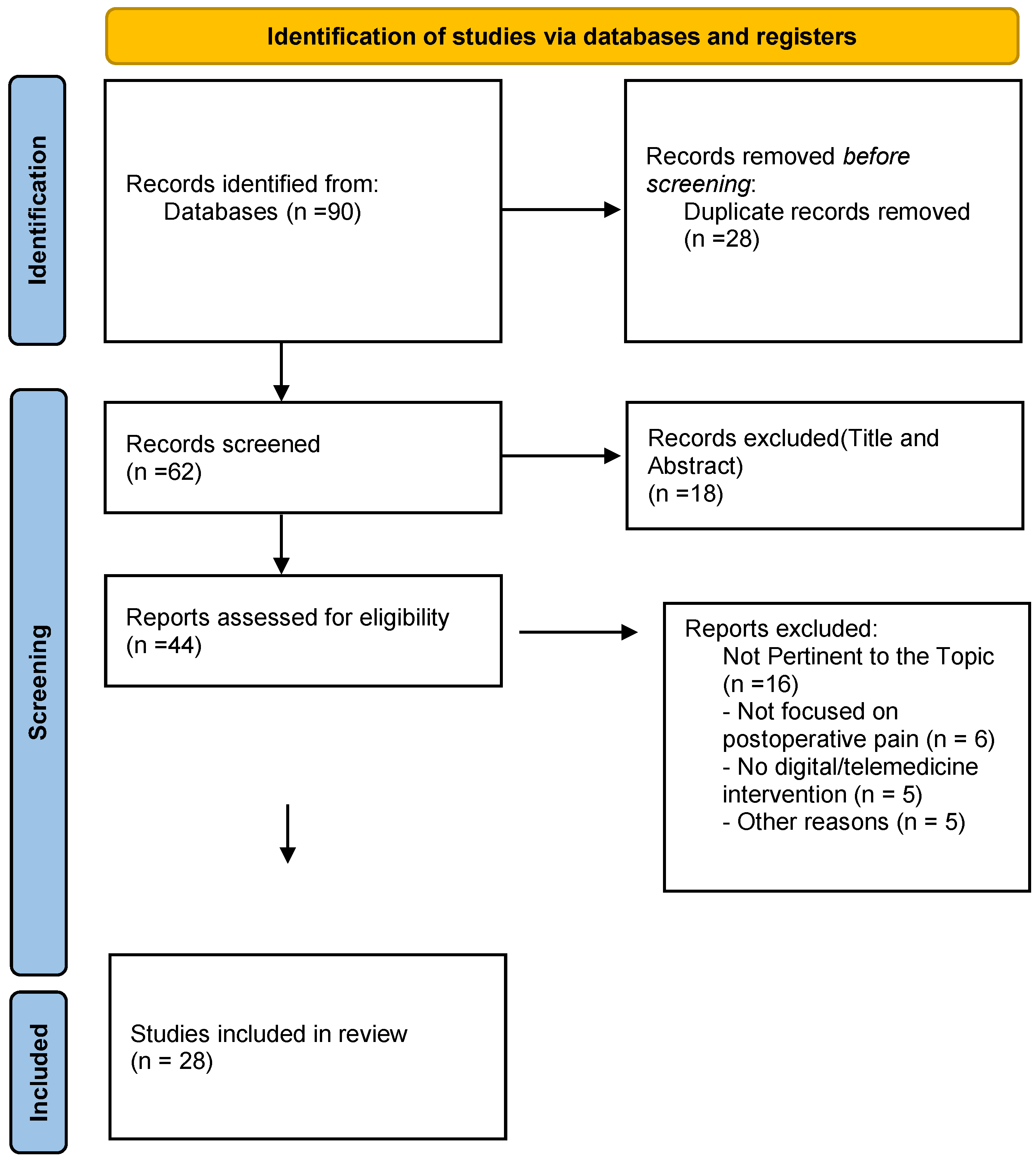
3.1. Selection of Studies
3.2. Main Results
- Digital Tools Used
- Role of Healthcare Professionals
- Clinical Outcomes
- Emerging Barriers
4. Discussion
4.1. Implications for Clinical Practice
4.2. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dahlberg, K.; Jaensson, M.; Nilsson, U. “Let the patient decide”—Person-centered postoperative follow-up contacts, initiated via a phone app after day surgery: Secondary analysis of a randomized controlled trial. Int. J. Surg. 2019, 61, 33–37. [Google Scholar] [CrossRef] [PubMed]
- McLemore, E.C.; Lee, L.; Hedrick, T.L.; Rashidi, L.; Askenasy, E.P.; Popowich, D.; Sylla, P. Same day discharge following elective, minimally invasive, colorectal surgery: A review of enhanced recovery protocols and early outcomes by the SAGES Colorectal Surgical Committee with recommendations regarding patient selection, remote monitoring, and successful implementation. Surg. Endosc. 2022, 36, 7898–7914. [Google Scholar] [CrossRef] [PubMed]
- Carlier, J.; Robin, F.; Pages, N.; Quinart, A.; Roy, M.; Pauchard, J.-C.; Quintana, I.; Nouette-Gaulain, K. Pain evaluation after day-surgery using a mobile phone application. Anaesth. Crit. Care Pain. Med. 2021, 40, 100879. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Chen, P.P.; Mok, M.H.T.; Chow, Y.F.; Chung, J.W.Y.; Law, A.C.B.; Lee, J.S.W.; Leung, E.M.F.; Tam, C.W.C. Typology of pain coping and associations with physical health, mental health, and pain profiles in Hong Kong Chinese older adults. Aging Ment. Health 2021, 25, 2169–2177. [Google Scholar] [CrossRef]
- Debono, B.; Bousquet, P.; Sabatier, P.; Plas, J.-Y.; Lescure, J.-P.; Hamel, O. Postoperative monitoring with a mobile application after ambulatory lumbar discectomy: An effective tool for spine surgeons. Eur. Spine J. 2016, 25, 3536–3542. [Google Scholar] [CrossRef]
- Rian, T.; Sand, K.; Skogvoll, E.; Klepstad, P.; Wik, T.S. A Web-Based Communication Tool for Postoperative Follow-up and Pain Assessment at Home After Primary Knee Arthroplasty: Feasibility and Usability Study. JMIR Form. Res. 2022, 6, e34543. [Google Scholar] [CrossRef]
- Gille, K.; Vermeulen, K.; Teunkens, A. Safety and follow-up systems after ambulatory peripheral nerve block: A narrative review. Acta Anaesthesiol. Belg. 2022, 73, 149–158. [Google Scholar] [CrossRef]
- Hofstad, J.K.; Klaksvik, J.; Klepstad, P.; Gjeilo, K.H.; Søballe, K.; Wik, T.S. Patient-reported outcomes the first thirty days after fast-track primary total hip arthroplasty. A prospective cohort study using a web-based registration tool for postoperative follow-up. Int. J. Orthop. Trauma. Nurs. 2024, 52, 101079. [Google Scholar] [CrossRef]
- Hansen, J.B.; Sørensen, J.F.L.; Glassou, E.N.; Homilius, M.; Hansen, T.B. Reducing patient–staff contact in fast-track total hip arthroplasty has no effect on patient-reported out-comes, but decreases satisfaction amongst patients with self-perceived complications: Analysis of 211 patients. Acta Orthop. 2022, 93, 264–270. [Google Scholar] [CrossRef]
- Azzellino, G.; Ginaldi, L.; De Martinis, M. Renew the Nursing Profession to Attract New Forces and Be Increasingly Inclusive and Attentive to Diversity. J. Adv. Nurs. 2024. early view. [Google Scholar] [CrossRef]
- Azzellino, G.; De Martinis, M. Territorial reorganization, telemedicine and operative centres: Challenges and opportunities for the nursing profession. J. Clin. Nurs. 2024, 33, 4518–4519. [Google Scholar] [CrossRef] [PubMed]
- Azzellino, G.; Dante, A.; Petrucci, C.; Caponnetto, V.; Aitella, E.; Lancia, L.; Ginaldi, L.; De Martinis, M. Intention to leave and missed nursing care: A scoping review. Int. J. Nurs. Stud. Adv. 2025, 8, 100312. [Google Scholar] [CrossRef] [PubMed]
- Tran-McCaslin, M.; Basam, M.; Rudikoff, A.; Thuraisingham, D.; McLemore, E.C. Reduced Opioid Use and Prescribing in a Same Day Discharge Pilot Enhanced Recovery Program for Elective Minimally Invasive Colorectal Surgical Procedures During the COVID-19 Pandemic. Am. Surg. 2022, 88, 2572–2578. [Google Scholar] [CrossRef] [PubMed]
- Wood, M.D.; West, N.C.; Sreepada, R.S.; Loftsgard, K.C.; Petersen, L.; Robillard, J.M.; Page, P.; Ridgway, R.; Chadha, N.K.; Portales-Casamar, E.; et al. Identifying Risk Factors, Patient-Reported Experience and Outcome Measures, and Data Capture Tools for an Individualized Pain Prediction Tool in Pediatrics: Focus Group Study. JMIR Perioper. Med. 2022, 5, e42341. [Google Scholar] [CrossRef]
- Wildemeersch, D.; D’Hondt, M.; Bernaerts, L.; Mertens, P.; Saldien, V.; Hendriks, J.M.; Walcarius, A.-S.; Sterkens, L.; Hans, G.H. Implementation of an Enhanced Recovery Pathway for Minimally Invasive Pectus Surgery: A Population-Based Cohort Study Evaluating Short- and Long-Term Outcomes Using eHealth Technology. JMIR Perioper. Med. 2018, 1, e10996. [Google Scholar] [CrossRef]
- Anthony, C.A.; Lawler, E.A.; Ward, C.M.; Lin, I.C.; Shah, A.S. Use of an Automated Mobile Phone Messaging Robot in Postoperative Patient Monitoring. Telemed. J. E Health 2018, 24, 61–66. [Google Scholar] [CrossRef]
- Glauser, G.; Ali, Z.S.; Gardiner, D.; Ramayya, A.G.; Pessoa, R.; Grady, M.S.; Welch, W.C.; Zager, E.L.; Sim, E.; Haughey, V.; et al. Assessing the utility of an IoS application in the perioperative care of spine surgery patients: The NeuroPath Pilot study. Mhealth 2019, 5, 40. [Google Scholar] [CrossRef]
- Pickens, R.; Cochran, A.; Tezber, K.; Berry, R.; Bhattacharya, E.; Koo, D.; King, L.; Iannitti, D.A.; Martinie, J.B.; Baker, E.H.; et al. Using a mobile application for real-time collection of patient-reported outcomes in hepatopancreatobiliary surgery within an ERASò pathway. Am. Surg. 2019, 85, 909–917. [Google Scholar] [CrossRef]
- Nilsson, U.; Jaensson, M.; Dahlberg, K.; Hugelius, K. Postoperative Recovery After General and Regional Anesthesia in Patients Undergoing Day Surgery: A Mixed Methods Study. J. Perianesth Nurs. 2019, 34, 517–528. [Google Scholar] [CrossRef]
- Highland, K.B.; Tran, J.; Edwards, H.; Bedocs, P.; Suen, J.; Buckenmaier, C.C. Feasibility of App-Based Postsurgical Assessment of Pain, Pain Impact, and Regional Anesthesia Effects: A Pilot Randomized Controlled Trial. Pain Med. 2019, 20, 1592–1599. [Google Scholar] [CrossRef]
- Kane, L.T.; Thakar, O.; Jamgochian, G.; Lazarus, M.D.; Abboud, J.A.; Namdari, S.; Horneff, J.G. The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J. Shoulder Elb. Surg. 2020, 29, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Loring, M.; Kabelac, Z.; Munir, U.; Yue, S.; Ephraim, H.Y.; Rahul, H.; Isaacson, K.B.; Griffith, L.G.; Katabi, D. Novel Technology to Capture Objective Data from Patients’ Recovery from Laparoscopic Endometriosis Surgery. J. Minim. Invasive Gynecol. 2021, 28, 325–331. [Google Scholar] [CrossRef]
- McGillion, M.H.; Parlow, J.; Borges, F.K.; Marcucci, M.; Jacka, M.; Adili, A.; Lalu, M.M.; Ouellette, C.; Bird, M.; Ofori, S.; et al. Post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: Randomised controlled trial. BMJ 2021, 374, n2209. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Yang, Y.; Shentu, Y.; Ding, Z.; Zhou, Q.; Tan, Q.; Luo, Q. Remote monitoring of patient recovery following lung cancer surgery: A messenger application approach. J. Thorac. Dis. 2021, 13, 1162–1171. [Google Scholar] [CrossRef]
- Tiozzo, E.; Biagioli, V.; Brancaccio, M.; Ricci, R.; Marchetti, A.; Dall’oglio, I.; Gawronski, O.; Bonanni, F.; Piga, S.; Celesti, L.; et al. Using an App to monitor postoperative pain at home in pediatric patients. J. Child. Health Care 2021, 25, 212–224. [Google Scholar] [CrossRef]
- Walrave, Y.; Carles, M.; Evain, J.N.; Ikonomoff, T.; Marie, A.; Ludot, H.; Bourdaud, N.; Kern, D.; Lejus-Bourdeau, C.; Orliaguet, G.; et al. A follow-up of pain reported by children undergoing outpatient surgery using a smartphone application: AlgoDARPEF multicenter descriptive prospective study. Pain 2022, 163, 2224–2231. [Google Scholar] [CrossRef] [PubMed]
- Thiel, B.; Godfried, M.B.; van Emst, M.E.; Vernooij, L.M.; van Vliet, L.M.; Rumke, E.; van Dongen, R.T.M.; Gerrits, W.; Koopman, J.S.H.A.; Kalkman, C.J. Quality of recovery after day care surgery with app-controlled remote monitoring: Study protocol for a randomized controlled trial. Trials 2023, 24, 102. [Google Scholar] [CrossRef]
- Morgan, J.K.; Rawlins, C.R.; Walther, S.K.; Harvey, A.; O’Donnell, A.; Greene, M.; Schmidt, T.G. A Mobile App for Postoperative Pain Management Among Older Veterans Undergoing Total Knee Arthroplasty: Mixed Methods Feasibility and Acceptability Pilot Study. JMIR Perioper. Med. 2023, 6, e50116. [Google Scholar] [CrossRef]
- Weiss, K.; Weiss, K.; Abimbola, O.; Abimbola, O.; Mueller, D.; Mueller, D.; Basak, R.; Basak, R.; Basch, E.; Basch, E.; et al. Feasibility, Acceptability, and Outcomes of a Mobile Health Tool for Radical Cystectomy Recovery. J. Urol. 2024, 211, 266–275. [Google Scholar] [CrossRef]
- Levit, T.; Grzela, P.; Lavoie, D.C.; Wang, L.; Agarwal, A.; Couban, R.J.; Shanthanna, H. The Effectiveness of Virtual and Augmented Reality in Surgical Pain Management: A Systematic Review of Randomized Controlled Trials. Anesth. Analg. 2024, 140, 1388–1400. [Google Scholar] [CrossRef]
- Vitale, S.; Fábregas Blanco, M.I.; Ricós Bugeda, P.; Turró, R.T.; Fernández Fernández, H.; Reñé de Antonio, E. Feasibility and acceptability of an app for monitoring acute postoperative pain in major outpatient surgery. Rev. Esp. Anestesiol. Reanim. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Brintz, C.E.; Kelly, E.C.; Polser, G.; Rhoten, B.A.; Pearce, M.F.; Coronado, R.A.; O’donnell, R.; Block, S.; Priest, A.; Gupta, R.; et al. Feasibility, Acceptability and Modification of a Post-surgical Telehealth Mindfulness-Based Intervention to Enhance Recovery After Lumbar Spine Surgery: A Prospective Intervention Study. Glob. Adv. Integr. Med. Health 2025, 14, 27536130251344843. [Google Scholar] [CrossRef] [PubMed]
- Cleeland, C.S.; Wang, X.S.; Shi, Q.; Mendoza, T.R.; Wright, S.L.; Berry, M.D.; Malveaux, D.; Shah, P.K.; Gning, I.; Hofstetter, W.L.; et al. Automated symptom alerts reduce postoperative symptom severity after cancer surgery: A randomized controlled clinical trial. J. Clin. Oncol. 2011, 29, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Azzellino, G.; Aitella, E.; Passamonti, M.; Ginaldi, L.; De Martinis, M. Protected discharge and combined interventions: A viable path to reduce hospital readmissions. Eur. J. Intern. Med. 2025. [Google Scholar] [CrossRef]
|
Author/ Year | Country | Study Type |
Main Theme | Population | Key Findings | Research Gaps |
|---|---|---|---|---|---|---|
| Debono et al., 2016 [5] | France | Prospective observational study | Home monitoring with mobile app after outpatient lumbar discectomy, with automatic alert based on pain and other symptoms. | 60 patients undergoing outpatient lumbar discectomy | 31.7% activated alarms, mainly for postoperative pain (72.4%). The app allowed timely contact with clinicians, optimized pain management and avoided improper access. High patient satisfaction and good usability | Pilot study design; need for RCTs to compare efficacy versus traditional follow-up. |
| Wildemeersch et al., 2018 [15] | Belgium | Prospective cohort study with retrospective comparison | Creating an Enhanced Recovery Pathway (ERP) with eHealth technologies for postoperative pain monitoring. | 29 adolescents underwent minimally invasive thoracic surgery for pectus | The use of a digital platform with telemonitoring devices has allowed for good long-term and home-based pain control. In addition, the platform allowed for early identification of persistent pain. High satisfaction and good adherence. | Small sample size; low adherence; single-center study; need for large-scale RCTs |
| Anthony et al., 2018 [16] | U.S.A. | Prospective study | Using an automated mobile phone messaging robot for postoperative patient monitoring | 47 patients undergoing orthopaedic surgery (monitored for 7 days) | The use of the messaging robot has improved postoperative monitoring, facilitating communication between patients and healthcare professionals. |
Monocentric study Small sample To be tested in larger populations and in different settings |
| Dahlberg et al., 2019 [1] | Sweden | Secondary analysis of multicenter RCT | Personalized postoperative follow-up via app (RAPP) with call activation by the patient. | 494 adult patients undergoing outpatient surgery (intervention group). | 17% of patients-initiated contact via the app, mainly for pain. Patients who requested contact had worse postoperative recovery. The app allows effective, personalized follow-up. | Limited data, missing demographic and clinical variables |
| Glauser et al., 2019 [17] | U.S.A. | Prospective pilot study | Introduction of NeuroPath mobile app to monitor postoperative phase of patients undergoing spontaneous surgery, with ERAS principles. | 30 patients undergoing elective spine surgery. | Discharged patients used the app regularly and showed improvements in pain reduction, increased physical activity, and a tendency to discontinue opioids. The app allows real-time therapy monitoring, with active patient involvement. |
Small sample size Low adherence to digital tool. Need for user training on interface Need for large-scale studies on clinical outcomes |
| Pickens et al., 2019 [18] | U.S.A. | Prospective pilot study | Use of a mobile application for the real-time collection of Patient-Reported Outcomes (PRO) in hepatopancreatobiliary surgery within an ERAS® pathway | 122 patients monitored for 30 days post-discharge | App adoption was 93% (114/122). Patients completed 62% of the PROs on quality of life, postoperative pain, nausea, opioid use, and adherence to ERAS® pathway elements. During post-discharge follow-up, 12 patients reported that the app prevented a hospital call and 3 reported avoiding an emergency room visit. | Pilot study with limited generalizability; single-center study; need for larger confirmatory trials |
| Nilsson et al., 2019 [19] | Sweden | Mixed methods study (RCT + interviews) | Comparison between general anesthesia (GA) and regional anesthesia (RA) on the quality of postoperative recovery, assessed by mobile app (RAPP) and SwQoR questionnaire | 401 patient’s outpatient surgery (quantitative), 20 patients (qualitative) | Pain from the surgical wound was the most frequent. The mobile app allows daily follow-up at home for 14 days. The quality of recovery was worse in patients with GA. |
Swedish sample only. It turns out that not all patients used the technology. |
|
Highland et al., 2019 [20] | U.S.A. | Pilot Randomized Controlled Trial | Feasibility of app-based monitoring of postoperative pain and anesthesia effects | 50 adult patients | The mCare app was feasible for postoperative assessment. Nurses reported higher satisfaction with the app compared to standard telephone follow-up methods. | Need for larger studies, long-term efficacy, and broader applicability |
| Kane et al., 2020 [21] | U.S.A. | Prospective RCT | Postoperative follow-up via telemedicine after arthroscopic rotator cuff repair. |
58 patients (28 with telemedicine follow-up, 30 with face-to-face follow -up) | No difference in pain scores between the groups at 2, 6 and 12 weeks. Patients in the telehealth group showed greater preference for this model, with less time spent and fewer working hours lost. Pain was monitored with VAS at each visit. | Monocentric design, short follow-up, limited generalizability due to inclusion of only tech-accessible patients. |
| Loring et al., 2021 [22] | U.S.A. | Prospective cohort pilot study | Using a non-contact wireless radio sensor (“Emerald”) to collect objective data on sleep quality and correlation with postoperative pain after laparoscopy for endometriosis. | Patients over the age of 18 with regular and independent sleep patterns and who are scheduled for laparoscopy for the diagnosis and treatment of suspected endometriosis. | The sensor collected objective physiological data for 10 weeks. There was a positive correlation between time to deep sleep and self-reported pain the following day. The device allowed for noninvasive and continuous monitoring of recovery. |
Very limited sample size. Need for larger cohorts |
| Carlier et al., 2021 [3] | France | Monocentric retrospective observational study | Postoperative pain monitoring after ambulatory surgery via mobile app. | 1691 adult and pediatric patients. | The app enabled personalized follow-up, early symptom detection, and targeted clinical interventions. High patient adherence and satisfaction. |
Questionnaires not validated. Sample limited to 5 specialties. Lack of data on the functional and social impact of pain |
| McGillion et al., 2021 [23] | Canada | Multicenter RCT | Integrated post-discharge remote monitoring with telemedicine to reduce complications and manage symptoms, including pain. | 905 adults ≥40 years discharged after non-elective surgery | The remote monitoring group reported less pain on days 7, 15, and 30. The system detected and corrected more errors in analgesic management. The intervention was well accepted and improved clinical follow-up at home. | Pain was not the primary outcome. |
| Cheng et al., 2021 [24] | China | Single-centre prospective observational study | Remote monitoring via app (WeChat) of post-operative symptoms after lung cancer surgery | 826 patients undergoing lung surgery; 589 with at least 3 answers to questionnaires | The app allowed the monitoring of pain up to 12 weeks. Pain decreased from 4.1 to 2.2. Factors associated with increased pain: female sex, age >60, thoracotomy, operating time >90 min, drainage >7 days. High adherence to the programme, and effective data collection without staff overload | Exclusion of patients without smartphone or family support. |
| Tiozzo et al., 2021 [25] | Italy | Prospective comparative study | Using a mobile application to monitor postoperative pain at home in pediatric patients | 487 pediatric patients | Forty-four percent of participants reported pain in the first 24 h after surgery, while 22% reported pain between the first and fifth days. The use of the app facilitated pain assessment, allowing healthcare professionals to actively involve pediatric patients and their parents in pain management at home. | Need for long-term evaluation of app effectiveness |
| Walrave et al., 2022 [26] | France | Multicenter prospective descriptive study | Use of a smartphone application for monitoring postoperative pain in children undergoing ambulatory surgery | Children undergoing outpatient surgery | The application has provided the opportunity to effectively monitor postoperative pain at home, improving communication between patients and healthcare professionals. | Need for long-term evaluation, limited generalizability |
|
Rian et al., 2022 [6] | Norway | Usability and feasibility sub-study within RCT | Web-based tools (Eir) for pain assessment and home follow-up. | Patients undergoing total knee replacement (aged 32–78 years) |
Most patients found the system easy to use and intuitive. The interface was accessible even to patients with limited technological skills. Most participants used the system without requiring technical support. The difficulties encountered were mainly related to the internet connection or login. The tool allowed for valid clinical follow-up with effective, constant, and precise recording of symptoms and use of analgesics, providing useful data for clinical practice and research. The system has proven itself in home monitoring of patients after hospital discharge. Older patients and those who did not have an electronic device had greater difficulty. Therefore, technological experience had a greater impact than the complexity of the tool itself. | Small sample size; feasibility sub-study; low digital literacy; barriers in older adults; infrastructure limitations. |
| Wood et al., 2022 [14] | Canada | Qualitative study | Identification of risk factors for postoperative pain and selection of digital tools for monitoring and data collection. | 22 participants (clinicians and caregivers of operated children) | Five key domains were identified: demographics, psychosocial, clinical, PREMs, and PROMs. The study also defined functional requirements and delivery modalities (e.g., electronic and repeated instruments). A data collection system was designed for future personalized predictive models. | Small sample size; lack of quantitative data. |
|
Tran-McCaslin et al., 2022 [13] | U.S.A. | Retrospective observational study on pilot program | Same-day discharge (SDD) program with remote monitoring via daily phone calls for postoperative pain control and opioid use after minimally invasive colorectal surgery | 37 patients selected for good health and elective colorectal surgery | Patients used less opioids than expected, despite reporting moderate pain in the first few days. The intervention led to a reduction in opioid prescriptions (from 40 to 10 tablets). Daily telephone calls allowed continuous clinical monitoring, including pain assessment and instructions on multimodal therapy. |
Small, highly selected sample Limited to telephone-based monitoring Need for further studies to support generalizability |
| Hansen et al., 2022 [9] | Denmark | Retrospective comparative observational study | Reducing patient-operator contact in the fast-track after total hip replacement and impact on patient-reported outcomes, including pain | Patients undergoing THA in three different fast-track pathways (with various levels of clinical contact, including telephone follow-ups) | The reduction of patient-staff contact (e.g., replacement by phone calls) did not affect self-reported postoperative pain or mobility. Satisfaction remained high. | Single-centre study |
|
Gille et al., 2022 [7] | Belgium | Narrative revision of literature | Postoperative follow-up systems after peripheral nerve blocks in ambulatory surgery, with a focus on digital instruments | 67 articles included, selected from international databases (Scopus, Embase, MEDLINE) | Patients receiving peripheral nerve blocks may experience moderate to severe pain up to 78% on the first postoperative day. Telephone follow- up has high rates of loss to follow-up (up to 50%). Digital systems (automated SMS, apps, video visits) improve response rates and detection of adverse events, including pain and neurological complications. | Few studies assess the impact on outcomes such as pain or readmissions. |
| McLemore et al., 2022 [2] | U.S.A., Canada, France | Multi-centre narrative review with clinical experiences | Digital follow-up and same-day discharge after minimally invasive colorectal surgery with pain monitoring | Patients undergoing minimally invasive colorectal surgery (multi-centre experience) | Pain was managed and monitored at home using NRS scales. Digital technologies (apps, video calls, phone calls) enabled active and timely follow-up. Reduced opioid use and high patient satisfaction were observed. | Need to validate effectiveness and sustainability of the model in larger populations. |
| Thiel et al., 2023 [27] | The Netherlands | Unblinded multi-centre RCT protocol | Remote monitoring of postoperative recovery via app after day surgery | 310 adult patients undergoing outpatient surgery in three Dutch hospitals | The app allows daily recording of pain and nausea; in case of need, the patient is contacted by healthcare professionals trained in empathic communication. An improvement in the quality of perceived recovery, measured by QoR-15 on day 7, is assumed. |
Study still ongoing. No definitive clinical results available. Excluding elderly patients or those with low digital literacy. |
| Morgan et al., 2023 [28] | U.S.A. | Mixed Methods Feasibility and Acceptability Pilot Study | Use of a mobile app (CPMRx) for postoperative pain management and monitoring of opioid use at home |
10 elderly patients with an average age of 68 8 years |
The mobile app was easily used by participants and was considered useful for postoperative pain management. The commitment to using the app, despite the age, was high. No problems emerged in using the technology. It emerged that the app could help personalize and optimize pain treatment, especially with the consumption of opioid drugs. The app provides tools for therapeutic education and supports patients in the decision before taking drugs, promoting a more conscious and safe use. The app collects data and therefore can offer clinically relevant information to improve pain management and therapy, preventing risks related to the use of opioids. | Small sample, low diversity, need for broader settings |
| Weiss et al., 2024 [29] | U.S.A | Prospective observational study | Using a mobile digital health tool for monitoring and support during post-operative recovery after radical cystectomy. | Adult patients undergoing radical cystectomy | The app was found to be accessible and easy to use, well accepted by patients, and useful for daily symptom monitoring, including postoperative pain. It facilitated communication, educational support, and symptom management at home | Small sample size; lack of RCTs; unclear impact on clinical outcomes and long-term pain |
| Hofstad et al., 2024 [8] | Norway | Prospective cohort study | Home follow-up via a web-based digital tool (EIR) to monitor pain and quality of life in the 30 days after total hip arthroplasty via a web-based digital tool (EIR) | 82 adult patients undergoing elective primary THA | Pain and quality of life remain critical in the first week after discharge but progressively improve. After 30 days, 32% of patients are still using opioids. The use of the web-based tool has allowed continuous monitoring, with high adherence. | Single-center study; exclusion of patients with poor digital skills or no home connection |
| Levit et al., 2024 [30] | Not-available | Systematic review of RCTs | Effectiveness of virtual (VR) and augmented reality (AR) in surgical pain management | Patients undergoing various surgeries | VR/AR have shown a significant reduction in postoperative pain in several studies, with decreased analgesic use and increased patient satisfaction. | Need for RCTs with larger samples and VR/AR protocol standardization |
| Vitale et al. (2025) [31] | Spain | Single-centre prospective observational study | Mobile app for monitoring acute postoperative pain in major outpatient surgery | Patients undergoing major outpatient surgery (exact number not reported in abstract) | The app was found to be feasible and acceptable. It allowed real-time monitoring of acute postoperative pain. High prevalence of moderate-to-severe pain and low satisfaction with analgesic treatment were observed, suggesting suboptimal pain control and the need for better guideline adherence. | Single centre; no control group; low satisfaction with analgesia despite technological support |
| Brintz et al. (2025) [32] | USA | Prospective intervention study | Telehealth-delivered mindfulness-based intervention post-lumbar spine surgery | Patients recovering from lumbar spine surgery (sample size not specified in summary) | The intervention was feasible and well accepted. Participants showed clinically meaningful improvements in pain intensity and disability at 3 months. Modifications to content and delivery were made based on patient feedback. | No control group; results may not be generalizable beyond lumbar spine surgery; sample size not reported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azzellino, G.; Aitella, E.; Ginaldi, L.; Vagnarelli, P.; De Martinis, M. Use of Digital and Telemedicine Tools for Postoperative Pain Management at Home: A Scoping Review of Health Professionals’ Roles and Clinical Outcomes. J. Clin. Med. 2025, 14, 4009. https://doi.org/10.3390/jcm14114009
Azzellino G, Aitella E, Ginaldi L, Vagnarelli P, De Martinis M. Use of Digital and Telemedicine Tools for Postoperative Pain Management at Home: A Scoping Review of Health Professionals’ Roles and Clinical Outcomes. Journal of Clinical Medicine. 2025; 14(11):4009. https://doi.org/10.3390/jcm14114009
Chicago/Turabian StyleAzzellino, Gianluca, Ernesto Aitella, Lia Ginaldi, Patrizia Vagnarelli, and Massimo De Martinis. 2025. "Use of Digital and Telemedicine Tools for Postoperative Pain Management at Home: A Scoping Review of Health Professionals’ Roles and Clinical Outcomes" Journal of Clinical Medicine 14, no. 11: 4009. https://doi.org/10.3390/jcm14114009
APA StyleAzzellino, G., Aitella, E., Ginaldi, L., Vagnarelli, P., & De Martinis, M. (2025). Use of Digital and Telemedicine Tools for Postoperative Pain Management at Home: A Scoping Review of Health Professionals’ Roles and Clinical Outcomes. Journal of Clinical Medicine, 14(11), 4009. https://doi.org/10.3390/jcm14114009







