BRIGHT-HD—A Brazilian Research Investigation on Public Health Gains Comparing Survival Rates Between Hemodialysis and Hemodiafiltration: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Outcomes
2.3. Statistical Analysis
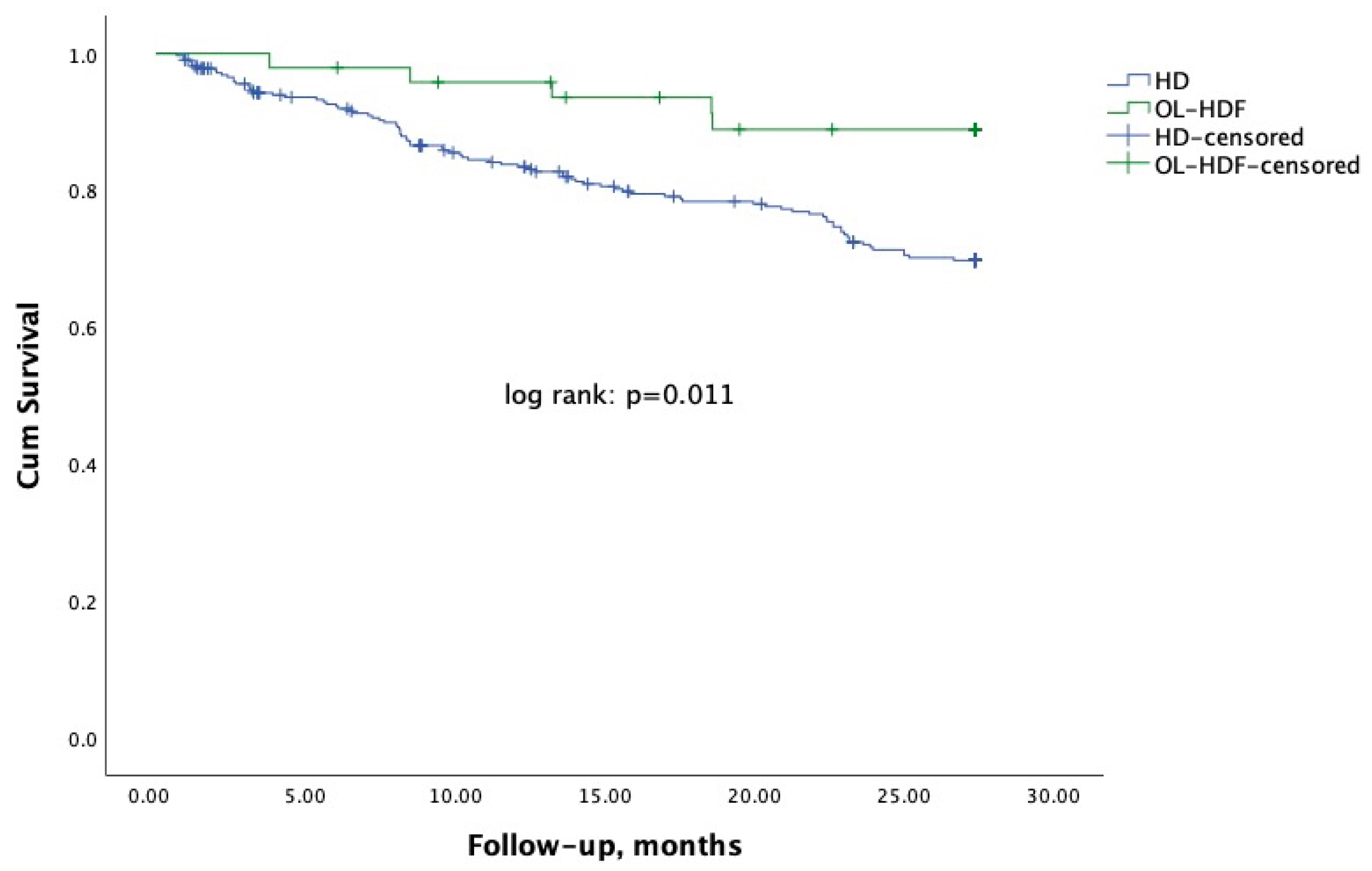
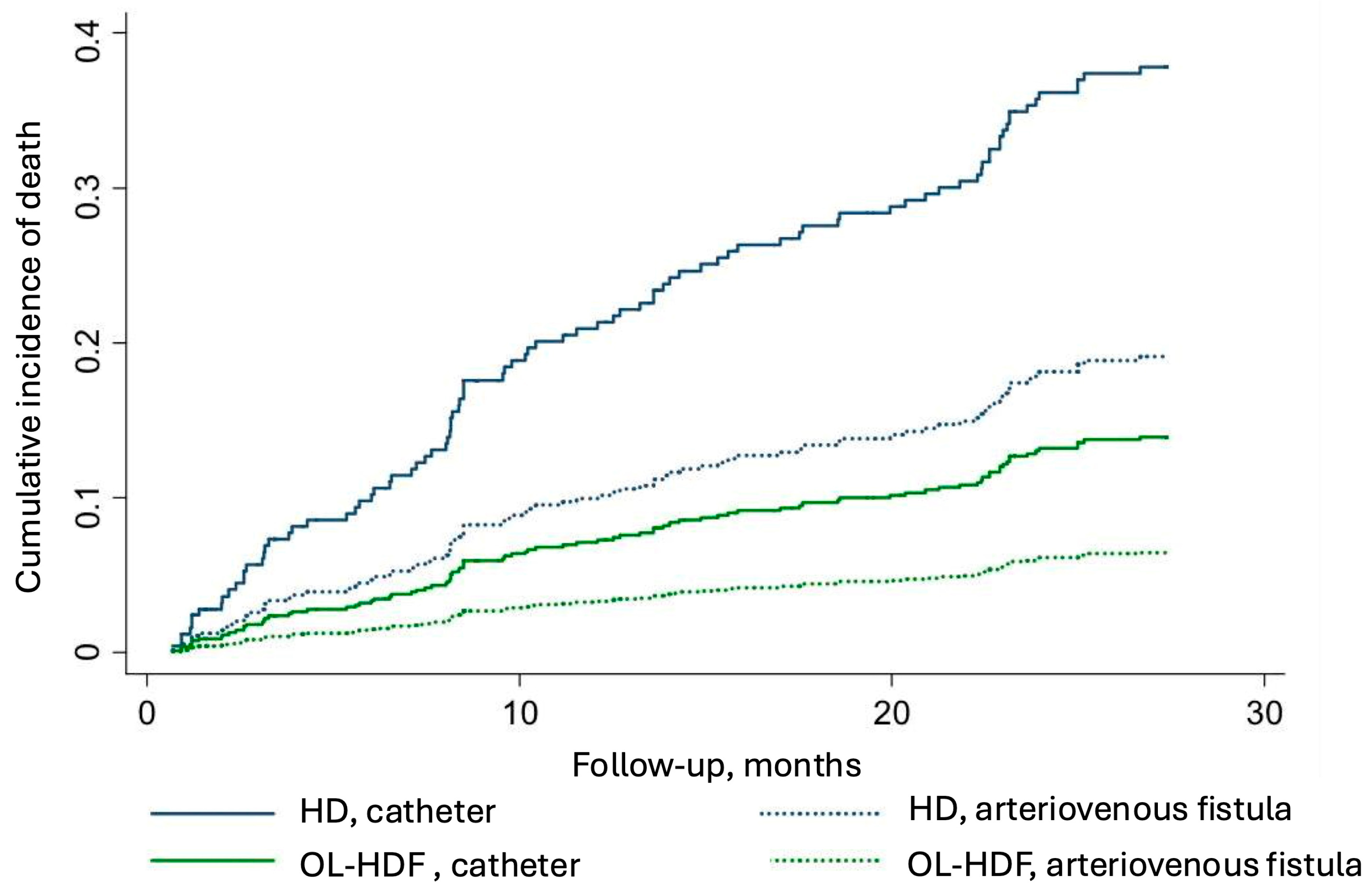
3. Results
4. Discussions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nerbass, F.B.; Lima, H.D.N.; Moura-Neto, J.A.; Lugon, J.R.; Sesso, R. Brazilian Dialysis Survey 2022. Braz. J. Nephrol. 2024, 46, e20230062. [Google Scholar] [CrossRef]
- Bello, A.K.; Okpechi, I.G.; Osman, M.A.; Cho, Y.; Htay, H.; Jha, V.; Wainstein, M.; Johnson, D.W. Epidemiology of haemodialysis outcomes. Nat. Rev. Nephrol. 2022, 18, 378–395. [Google Scholar] [CrossRef] [PubMed]
- Ok, E.; Asci, G.; Toz, H.; Ok, E.S.; Kircelli, F.; Yilmaz, M.; Hur, E.; Demirci, M.S.; Demirci, C.; Duman, S.; et al. Mortality and cardiovascular events in online haemodiafiltration (OL-HDF) compared with high-flux dialysis: Results from the Turkish OL-HDF Study. Nephrol. Dial. Transplant. 2013, 28, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Maduell, F.; Moreso, F.; Pons, M.; Ramos, R.; Mora-Macia, J.; Carreras, J.; Soler, J.; Torres, F.; Campistol, J.M.; Martinez-Castelao, A.; et al. High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J. Am. Soc. Nephrol. JASN 2013, 24, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Blankestijn, P.J.; Vernooij, R.W.M.; Hockham, C.; Strippoli, G.F.M.; Canaud, B.; Hegbrant, J.; Barth, C.; Covic, A.; Cromm, K.; Cucui, A.; et al. Effect of Hemodiafiltration or Hemodialysis on Mortality in Kidney Failure. N. Engl. J. Med. 2023, 389, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Sociedade Brasileira de Nefrologia. Censo Brasileiro de Diálise. Available online: http://censo-sbn.org.br/inicio?_gl=1*xyuvlm*_ga*NjkxMDIwMTguMTczMDIxNzY5OA..*_ga_E1HJB87YJ7*MTczMDIxNzY5OC4xLjAuMTczMDIxNzY5OC42MC4wLjA (accessed on 20 May 2025).
- da Rocha, E.P.; Kojima, C.A.; Modelli de Andrade, L.G.; Costa, D.M.; Magalhaes, A.O.; Rocha, W.F.; de Vasconcelos Junior, L.N.; Rosa, M.G.; Wagner Martins, C.S. Comparing Survival Outcomes between Hemodialysis and Hemodiafiltration Using Real-World Data from Brazil. J. Clin. Med. 2024, 13, 594. [Google Scholar] [CrossRef] [PubMed]
- Barra, A.B.L.; Roque-da-Silva, A.P.; Canziani, M.E.F.; Lugon, J.R.; Strogoff-de-Matos, J.P. Characteristics and predictors of mortality on haemodialysis in Brazil: A cohort of 5,081 incident patients. BMC Nephrol. 2022, 23, 77. [Google Scholar] [CrossRef] [PubMed]
- Canziani, M.E.F.; Strogoff-de-Matos, J.P.; Guedes, M.; Barra, A.B.L.; Canhada, S.; Carvalho, L.; Gemente, D.; Poli-de-Figueiredo, C.E.; Pecoits-Filho, R. High volume online hemodiafiltration: A global perspective and the Brazilian experience. Braz. J. Nephrol. 2024, 46, e20230104. [Google Scholar] [CrossRef]
- Larkin, J.W.; Han, M.; Han, H.; Guedes, M.H.; Goncalves, P.B.; Poli-de-Figueiredo, C.E.; Cuvello-Neto, A.L.; Barra, A.B.L.; de Moraes, T.P.; Usvyat, L.A.; et al. Impact of hemodialysis and post-dialysis period on granular activity levels. BMC Nephrol. 2020, 21, 197. [Google Scholar] [CrossRef] [PubMed]
- do Nascimento Lima, H.; Monarrez-Espino, J.; Nerbass, F.B.; Moura-Neto, J.A.; Sesso, R.; Lugon, J.R.; Brazilian Dialysis Register Investigators. Comparison of 1-year survival between patients initiating chronic hemodialysis under public and private health insurance: Register-based data analysis from Brazil. Int. Urol. Nephrol. 2024, 56, 3013–3022. [Google Scholar] [CrossRef]
- Barra, A.B.L.; Silva, A.; Canziani, M.E.F.; Lugon, J.R.; Matos, J.P.S. Survival in hemodialysis in Brazil according to the source of payment for the treatment: Public Healthcare System (SUS) versus private insurance. Braz. J. Nephrol. 2023, 45, 302–309. [Google Scholar] [CrossRef]
- Aquino, H.B.S.; Canziani, M.E.F.; Barra, A.B.L.; Roque-da-Silva, A.P.; Strogoff-de-Matos, J.P.; Dalboni, M.A.; Moyses, R.M.A.; Elias, R.M. PTH may predict early mortality in incident patients on hemodialysis: Results from a large cohort. Int. Urol. Nephrol. 2025, 57, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Roetker, N.S.; Gilbertson, D.T.; Weinhandl, E.D. A Brief Introduction to Competing Risks in the Context of Kidney Disease Epidemiology. Kidney360 2022, 3, 740–743. [Google Scholar] [CrossRef] [PubMed]
- Al-Wahsh, H.; Tangri, N.; Quinn, R.; Liu, P.; Ferguson Ms, T.; Fiocco, M.; Lam Md, M.N.N.; Tonelli, M.; Ravani, P. Accounting for the Competing Risk of Death to Predict Kidney Failure in Adults With Stage 4 Chronic Kidney Disease. JAMA Netw. Open 2021, 4, e219225. [Google Scholar] [CrossRef] [PubMed]
- Di Iorio, B.; Di Micco, L.; Bruzzese, D.; Nardone, L.; Russo, L.; Formisano, P.; D’Esposito, V.; Russo, D. Ultrapure dialysis water obtained with additional ultrafilter may reduce inflammation in patients on hemodialysis. J. Nephrol. 2017, 30, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, T.; Nakai, S.; Masakane, I.; Watanabe, Y.; Iseki, K.; Tsubakihara, Y.; Akizawa, T. Dialysis fluid endotoxin level and mortality in maintenance hemodialysis: A nationwide cohort study. Am. J. Kidney Dis. 2015, 65, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Wasse, H.; Speckman, R.A.; McClellan, W.M. Arteriovenous fistula use is associated with lower cardiovascular mortality compared with catheter use among ESRD patients. Semin. Dial. 2008, 21, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Pisoni, R.L.; Arrington, C.J.; Albert, J.M.; Ethier, J.; Kimata, N.; Krishnan, M.; Rayner, H.C.; Saito, A.; Sands, J.J.; Saran, R.; et al. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: An instrumental variable analysis. Am. J. Kidney Dis. 2009, 53, 475–491. [Google Scholar] [CrossRef] [PubMed]
- Lyu, B.; Chan, M.R.; Yevzlin, A.S.; Gardezi, A.; Astor, B.C. Arteriovenous Access Type and Risk of Mortality, Hospitalization, and Sepsis Among Elderly Hemodialysis Patients: A Target Trial Emulation Approach. Am. J. Kidney Dis. 2022, 79, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am. J. Kidney Dis. 2020, 75, S1–S164. [Google Scholar] [CrossRef] [PubMed]
| Variable | HD N = 321 | OL-HDF N = 48 | p |
|---|---|---|---|
| Age, years | 60 ± 14 | 61 ± 14 | 0.676 |
| White race, n (%) | 212 (66.0) | 32 (66.7) | 0.932 |
| Men, n (%) | 176 (54.8) | 30 (62.5) | 0.318 |
| Arteriovenous fistula, n (%) | 152 (47.4) | 21 (43.8) | 0.641 |
| Diabetes, n (%) | 175 (54.5) | 14 (29.2) | 0.001 |
| Dialysis frequency/week, % | <0.001 | ||
| Three times | 94.1 | 66.7 | |
| Four or more times | 5.9 | 33.3 | |
| Dialysis vintage, months | 75.1 (33.4, 156.0) | 35.3 (6.2, 68.2) | <0.001 |
| Week dialysis duration, h | 11.2 ± 1.8 | 10.5 ± 1.6 | 0.006 |
| Univariate Model | Initial Multivariate Model | Final Multivariate Model | ||||
|---|---|---|---|---|---|---|
| Crude HR (IC 95%) | p | Adjusted HR (IC 95%) | p | Adjusted HR (IC 95%) | p | |
| HD—reference | 0.33 (0.13–0.81) | 0.015 | 0.32 (0.13–0.81) | 0.015 | 0.32 (0.13–0.77) | 0.011 |
| Age, years | 1.01 (1.00–1.03) | 0.104 | 1.01 (0.99–1.03) | 0.234 | - | - |
| Diabetes | 1.47 (0.97–2.23) | 0.068 | 1.36 (0.88–2.09) | 0.167 | - | - |
| Arteriovenous fistula | 0.46 (0.29–0.71) | <0.001 | 0.46 (0.29–0.72) | 0.001 | 0.45 (0.29–0.69) | <0.001 |
| Hours on dialysis/week | 0.95 (0.87–1.05) | 0.339 | 0.93 (0.85–1.03) | 0.177 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luciano, E.P.; Chang, J.; Arantes, E.C.S.; Cordeiro, A.; Reis, S.F.S.; Andrade, D.V.; Rocha, W.F.; Magalhães, A.O.; Borges, C.M.; Elias, R.M. BRIGHT-HD—A Brazilian Research Investigation on Public Health Gains Comparing Survival Rates Between Hemodialysis and Hemodiafiltration: An Observational Study. J. Clin. Med. 2025, 14, 3981. https://doi.org/10.3390/jcm14113981
Luciano EP, Chang J, Arantes ECS, Cordeiro A, Reis SFS, Andrade DV, Rocha WF, Magalhães AO, Borges CM, Elias RM. BRIGHT-HD—A Brazilian Research Investigation on Public Health Gains Comparing Survival Rates Between Hemodialysis and Hemodiafiltration: An Observational Study. Journal of Clinical Medicine. 2025; 14(11):3981. https://doi.org/10.3390/jcm14113981
Chicago/Turabian StyleLuciano, Eduardo P., João Chang, Elaine C. S. Arantes, Aline Cordeiro, Sandra F. S. Reis, Douglas V. Andrade, Whelington F. Rocha, Andrea O. Magalhães, Cynthia M. Borges, and Rosilene M. Elias. 2025. "BRIGHT-HD—A Brazilian Research Investigation on Public Health Gains Comparing Survival Rates Between Hemodialysis and Hemodiafiltration: An Observational Study" Journal of Clinical Medicine 14, no. 11: 3981. https://doi.org/10.3390/jcm14113981
APA StyleLuciano, E. P., Chang, J., Arantes, E. C. S., Cordeiro, A., Reis, S. F. S., Andrade, D. V., Rocha, W. F., Magalhães, A. O., Borges, C. M., & Elias, R. M. (2025). BRIGHT-HD—A Brazilian Research Investigation on Public Health Gains Comparing Survival Rates Between Hemodialysis and Hemodiafiltration: An Observational Study. Journal of Clinical Medicine, 14(11), 3981. https://doi.org/10.3390/jcm14113981





