A Retrospective Study of Lumbar Disk Herniation: An Analysis of Clinical Cases and Treatment Plans
Abstract
1. Introduction
1.1. Conservative Management
1.2. Surgical Interventions
1.3. Comparative Value of Treatments
1.4. Objectives
2. Materials and Methods
2.1. Data Acquisition and Statistical Analysis
2.2. Standardized Conservative Treatment
3. Results
3.1. The Distribution of Patients Based on Gender
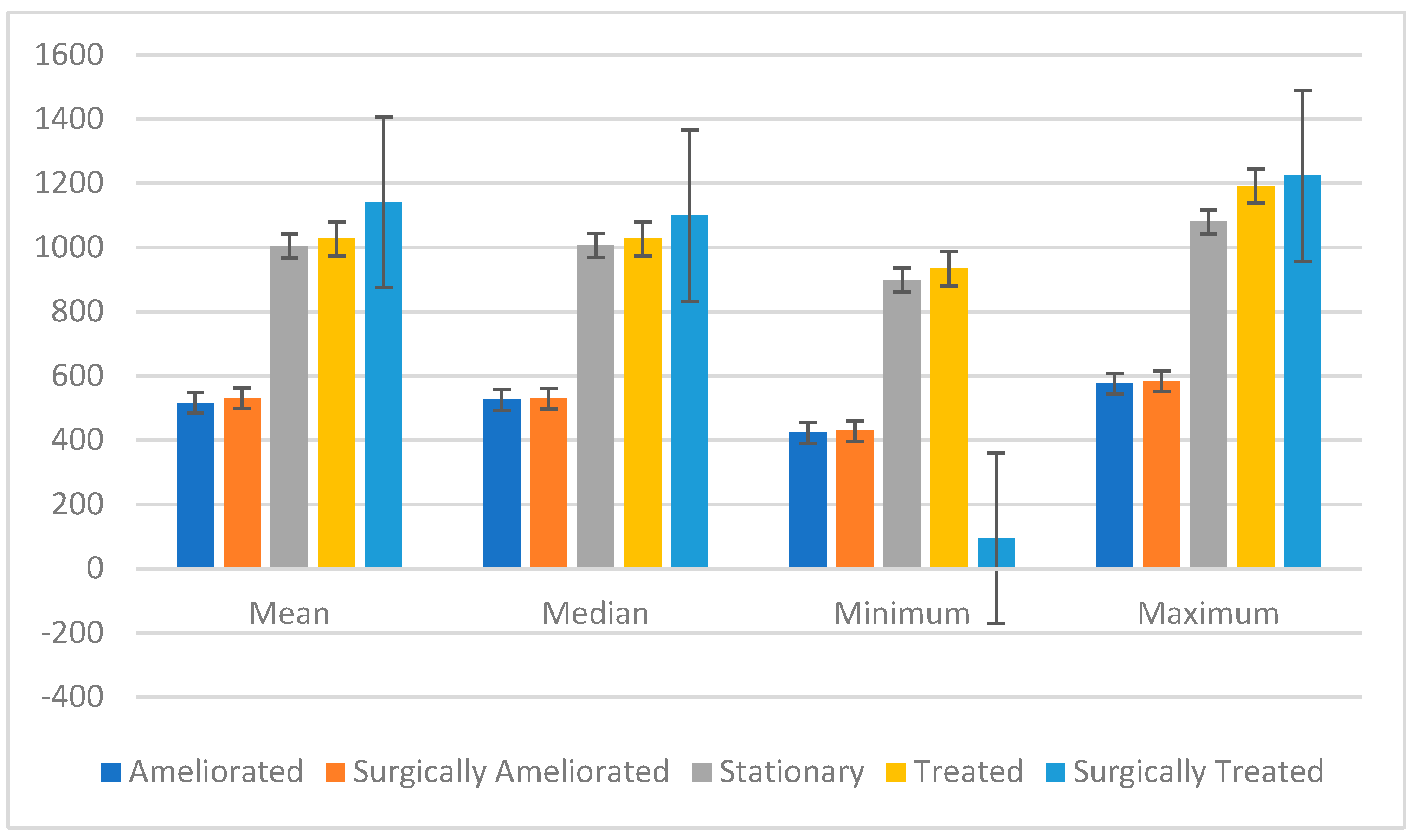
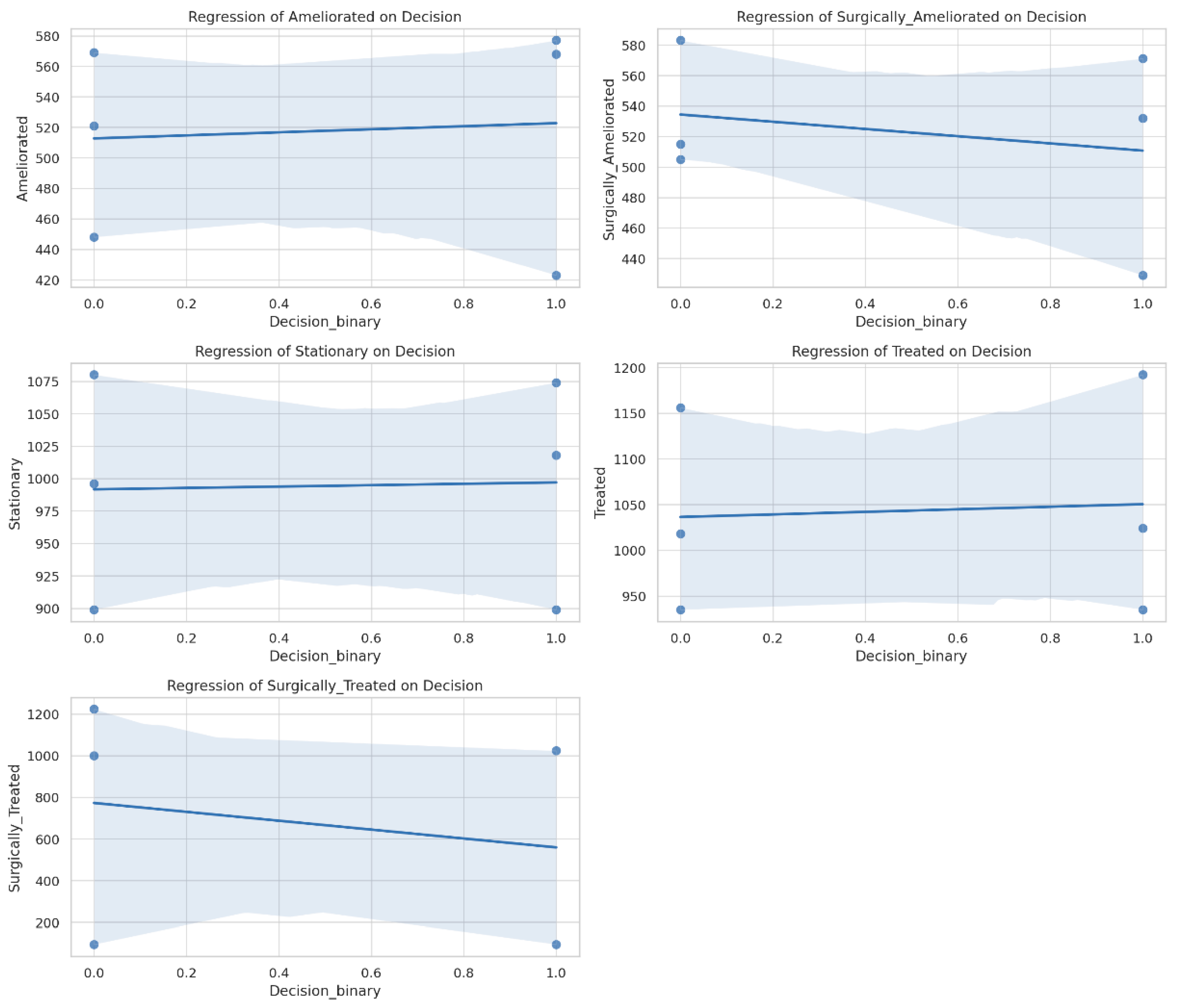
3.2. The Distribution of Patients Based on Treatment Methods and Outcomes
- (a)
- Spondylolisthesis (slippage of a vertebra from its normal position over the one below it)—12 cases in 2022, 14 cases in 2023, and 13 cases in 2024.
- (b)
- Vertebral trauma—6 cases in 2022 (five fractures and one fall-related injury), 5 cases in 2023 (one accident, one trauma, one fracture, and two fall-related injuries), and 12 cases in 2024 (three accidents, four traumatic injuries, three fractures, and two fall-related injuries).
3.3. The Distribution of Patients Based on Comorbidities
4. Discussion
4.1. Comparison of Surgical and Non-Surgical Treatments
4.2. Risk Factors and Patient-Specific Outcomes
4.3. Limitations and Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amin, R.M.; Andrade, N.S.; Neuman, B.J. Lumbar Disc Herniation. Curr. Rev. Musculoskelet. Med. 2017, 10, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.S.; Xu, A.; Ansari, K.; Hardacker, K.; Anderson, G.; Alsoof, D.; Daniels, A.H. Lumbar Disc Herniation: Diagnosis and Management. Am. J. Med. 2023, 136, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Cioanca, O.; Lungu, I.-I.; Batir-Marin, D.; Lungu, A.; Marin, G.-A.; Huzum, R.; Stefanache, A.; Sekeroglu, N.; Hancianu, M. Modulating Polyphenol Activity with Metal Ions: Insights into Dermatological Applications. Pharmaceutics 2025, 17, 194. [Google Scholar] [CrossRef]
- Marinescu, M.A.; Guliciuc, M.; Maier, A.C.; Olaru, I.; Bogdan-Goroftei, R.-E.; Barbu, R.E.; Mihailov, R.; Lutenco, V.; Firescu, D. Diagnostic and Therapeutic Particularities of a Case Admitted for Low Back Pain and Sciatica. Electron. J. Gen. Med. 2025, 22, em630. [Google Scholar] [CrossRef]
- Deyo, R.A.; Mirza, S.K. Herniated Lumbar Intervertebral Disk. N. Engl. J. Med. 2016, 374, 1763–1772. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, K.H.; Kang, S.; Kim, D.H.; Kim, D.H.; Kim, B.R.; Kim, W.; Kim, J.H.; Do, K.H.; Do, J.G. Nonsurgical Treatments for Patients with Radicular Pain from Lumbosacral Disc Herniation. Spine J. 2019, 19, 1478–1489. [Google Scholar] [CrossRef]
- Wang, W.; Long, F.; Wu, X.; Li, S.; Lin, J. Clinical Efficacy of Mechanical Traction as Physical Therapy for Lumbar Disc Herniation: A Meta-Analysis. Comput. Math. Methods Med. 2022, 2022, 5670303. [Google Scholar] [CrossRef]
- Vanti, C.; Panizzolo, A.; Turone, L.; Guccione, A.A.; Violante, F.S.; Pillastrini, P.; Bertozzi, L. Effectiveness of Mechanical Traction for Lumbar Radiculopathy: A Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzaa231. [Google Scholar] [CrossRef]
- Cheng, Y.-H.; Hsu, C.-Y.; Lin, Y.-N. The Effect of Mechanical Traction on Low Back Pain in Patients with Herniated Intervertebral Disks: A Systemic Review and Meta-Analysis. Clin. Rehabil. 2020, 34, 13–22. [Google Scholar] [CrossRef]
- Gugliotta, M.; da Costa, B.R.; Dabis, E.; Theiler, R.; Jüni, P.; Reichenbach, S.; Landolt, H.; Hasler, P. Surgical versus Conservative Treatment for Lumbar Disc Herniation: A Prospective Cohort Study. BMJ Open 2016, 6, e012938. [Google Scholar] [CrossRef]
- Reiman, M.P.; Sylvain, J.; Loudon, J.K.; Goode, A. Return to Sport after Open and Microdiscectomy Surgery versus Conservative Treatment for Lumbar Disc Herniation: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2016, 50, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Saberi, H.; Isfahani, A.V. Higher Preoperative Oswestry Disability Index Is Associated with Better Surgical Outcome in Upper Lumbar Disc Herniations. Eur. Spine J. 2008, 17, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Werner, D.A.T.; Grotle, M.; Gulati, S.; Austevoll, I.M.; Lønne, G.; Nygaard, Ø.P.; Solberg, T.K. Criteria for Failure and Worsening after Surgery for Lumbar Disc Herniation: A Multicenter Observational Study Based on Data from the Norwegian Registry for Spine Surgery. Eur. Spine J. 2017, 26, 2650–2659. [Google Scholar] [CrossRef]
- Smith, N.; Masters, J.; Jensen, C.; Khan, A.; Sprowson, A. Systematic Review of Microendoscopic Discectomy for Lumbar Disc Herniation. Eur. Spine J. 2013, 22, 2458–2465. [Google Scholar] [CrossRef]
- Chen, B.-L.; Guo, J.-B.; Zhang, H.-W.; Zhang, Y.-J.; Zhu, Y.; Zhang, J.; Hu, H.-Y.; Zheng, Y.-L.; Wang, X.-Q. Surgical versus Non-Operative Treatment for Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2018, 32, 146–160. [Google Scholar] [CrossRef]
- Lurie, J.D.; Tosteson, T.D.; Tosteson, A.N.A.; Zhao, W.; Morgan, T.S.; Abdu, W.A.; Herkowitz, H.; Weinstein, J.N. Surgical Versus Nonoperative Treatment for Lumbar Disc Herniation: Eight-Year Results for the Spine Patient Outcomes Research Trial. Spine 2014, 39, 3. [Google Scholar] [CrossRef]
- Rickers, K.W.; Pedersen, P.H.; Tvedebrink, T.; Eiskjær, S.P. Comparison of Interventions for Lumbar Disc Herniation: A Systematic Review with Network Meta-Analysis. Spine J. 2021, 21, 1750–1762. [Google Scholar] [CrossRef]
- Zhao, X.; Chen, A.; Lou, X.; Zhang, Y. Comparison of Three Common Intervertebral Disc Discectomies in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis Based on Multiple Data. J. Clin. Med. 2022, 11, 6604. [Google Scholar] [CrossRef]
- Hahne, A.J.; Ford, J.J.; McMeeken, J.M. Conservative Management of Lumbar Disc Herniation with Associated Radiculopathy: A Systematic Review. Spine 2010, 35, E488. [Google Scholar] [CrossRef]
- Akagi, R.; Aoki, Y.; Ikeda, Y.; Nakajima, F.; Ohtori, S.; Takahashi, K.; Yamagata, M. Comparison of Early and Late Surgical Intervention for Lumbar Disc Herniation: Is Earlier Better? J. Orthop. Sci. 2010, 15, 294–298. [Google Scholar] [CrossRef]
- Lilly, D.T.; Davison, M.A.; Eldridge, C.M.; Singh, R.; Montgomery, E.Y.; Bagley, C.; Adogwa, O. An Assessment of Nonoperative Management Strategies in a Herniated Lumbar Disc Population: Successes Versus Failures. Glob. Spine J. 2021, 11, 1054–1063. [Google Scholar] [CrossRef] [PubMed]
- El Melhat, A.M.; Youssef, A.S.A.; Zebdawi, M.R.; Hafez, M.A.; Khalil, L.H.; Harrison, D.E. Non-Surgical Approaches to the Management of Lumbar Disc Herniation Associated with Radiculopathy: A Narrative Review. J. Clin. Med. 2024, 13, 974. [Google Scholar] [CrossRef] [PubMed]
- Shimia, M.; Babaei-Ghazani, A.; Sadat, B.; Habibi, B.; Habibzadeh, A. Risk Factors of Recurrent Lumbar Disk Herniation. Asian J. Neurosurg. 2022, 8, 93–96. [Google Scholar] [CrossRef]
- Shin, B.-J. Risk Factors for Recurrent Lumbar Disc Herniations. Asian Spine J. 2014, 8, 211–215. [Google Scholar] [CrossRef]
- Li, Z.; Yang, H.; Liu, M.; Lu, M.; Chu, J.; Hou, S.; Hou, T. Clinical Characteristics and Risk Factors of Recurrent Lumbar Disk Herniation: A Retrospective Analysis of Three Hundred Twenty-One Cases. Spine 2018, 43, 1463. [Google Scholar] [CrossRef]
- Neculăeș, M.; Hernandez-Lucas, P.; Lucaci, P. Implications of Stabilometric Assessment in Determining Functional Deficits in Patients with Severe Knee Osteoarthritis: Observational Study. J. Clin. Med. 2024, 13, 3181. [Google Scholar] [CrossRef]
- Duceac, M.; Gutu, C.; Eva, L.; Dabija, M.G.; Calin, G.; Duceac, L.D.; Ciupilan, C.; Voinescu, D.C. 666 Retrospective Study of Lumbar Disc Herniation in a Hospital in North-Eastern Romania. Balneo PRM Res. J. 2024, 15. [Google Scholar] [CrossRef]
- De Simone, M.; Choucha, A.; Ciaglia, E.; Conti, V.; Pecoraro, G.; Santurro, A.; Puca, A.A.; Cascella, M.; Iaconetta, G. Discogenic Low Back Pain: Anatomic and Pathophysiologic Characterization, Clinical Evaluation, Biomarkers, AI, and Treatment Options. J. Clin. Med. 2024, 13, 5915. [Google Scholar] [CrossRef]
- Scrofani, R.; De Simone, M.; Migliorini, F.; Amoroso, E.; Maffulli, N.; Narciso, N.; Iaconetta, G. Spontaneous Resolution of Symptomatic Synovial Cysts of the Lumbar Spine: A Comprehensive Review with Two Illustrative Cases. Medicina 2024, 60, 1115. [Google Scholar] [CrossRef]
- Choucha, A.; Travaglini, F.; De Simone, M.; Evin, M.; Farah, K.; Fuentes, S. The Da Vinci Robot, a Promising yet Underused Minimally Invasive Tool for Spine Surgery: A Scoping Review of Its Current Role and Limits. Neurochirurgie 2025, 71, 101624. [Google Scholar] [CrossRef]
- Arts, M.P.; Kuršumović, A.; Miller, L.E.; Wolfs, J.F.; Perrin, J.M.; Van de Kelft, E.; Heidecke, V. Comparison of Treatments for Lumbar Disc Herniation: Systematic Review with Network Meta-Analysis. Medicine 2019, 98, e14410. [Google Scholar] [CrossRef] [PubMed]
- Abdu, R.W.; Abdu, W.A.; Pearson, A.M.; Zhao, W.; Lurie, J.D.; Weinstein, J.N. Reoperation for Recurrent Intervertebral Disc Herniation in the Spine Patient Outcomes Research Trial: Analysis of Rate, Risk Factors, and Outcome. Spine 2017, 42, 1106. [Google Scholar] [CrossRef] [PubMed]
- Blamoutier, A. Surgical Discectomy for Lumbar Disc Herniation: Surgical Techniques. Orthop. Traumatol. Surg. Res. 2013, 99, S187–S196. [Google Scholar] [CrossRef]
- Miwa, S.; Yokogawa, A.; Kobayashi, T.; Nishimura, T.; Igarashi, K.; Inatani, H.; Tsuchiya, H. Risk Factors of Recurrent Lumbar Disk Herniation: A Single Center Study and Review of the Literature. Clin. Spine Surg. 2015, 28, E265. [Google Scholar] [CrossRef]
- Plesea-Condratovici, A.; Plesea-Condratovici, C.; Rosoga, N.; Nedelcu, N. Efficacy and Tolerability of a Novel Food Supplement (Turbofer (R)) Containing Microencapsulated Iron in Liposomal Form, in Female Iron Deficiency Anaemia. Prog. Nutr. 2015, 17, 214–219. [Google Scholar]
- Delgado-López, P.D.; Rodríguez-Salazar, A.; Martín-Alonso, J.; Martín-Velasco, V. Lumbar Disc Herniation: Natural History, Role of Physical Examination, Timing of Surgery, Treatment Options and Conflicts of Interests. Neurocirugía 2017, 28, 124–134. [Google Scholar] [CrossRef]
- Hoffeld, K.; Lenz, M.; Egenolf, P.; Weber, M.; Heck, V.; Eysel, P.; Scheyerer, M.J. Patient-Related Risk Factors and Lifestyle Factors for Lumbar Degenerative Disc Disease: A Systematic Review. Neurochirurgie 2023, 69, 101482. [Google Scholar] [CrossRef]
- Wang, H.; Wang, T.; Wang, Q.; Ding, W. Incidence and Risk Factors of Persistent Low Back Pain Following Posterior Decompression and Instrumented Fusion for Lumbar Disk Herniation. J. Pain. Res. 2017, 10, 1019–1025. [Google Scholar] [CrossRef]
- Wilson Zingg, R.; Kendall, R. Obesity, Vascular Disease, and Lumbar Disk Degeneration: Associations of Comorbidities in Low Back Pain. PMR 2017, 9, 398–402. [Google Scholar] [CrossRef]
- Lambrechts, M.J.; Pitchford, C.; Hogan, D.; Li, J.; Fogarty, C.; Rawat, S.; Leary, E.V.; Cook, J.L.; Choma, T.J. Lumbar Spine Intervertebral Disc Desiccation Is Associated with Medical Comorbidities Linked to Systemic Inflammation. Arch. Orthop. Trauma. Surg. 2023, 143, 1143–1153. [Google Scholar] [CrossRef]
- Branisteanu, D.C.; Moraru, A.D.; Maranduca, M.A.; Branisteanu, D.E.; Stoleriu, G.; Branisteanu, C.I.; Balta, F. Intraocular Pressure Changes during and after Silicone Oil Endotamponade (Review). Exp. Ther. Med. 2020, 20, 204. [Google Scholar] [CrossRef] [PubMed]
- Grierosu, C.; Mihai, C.; Lungu, I.I.; Calin, G.; Stefanache, A.; Vasiliu, M.P.; Ivona, D. Stress-Induced Variability in Local Anesthesia Response: Exploring Implications for Dental Anesthetic Management. Rom. J. Oral. Rehabil. 2024, 16, 608–617. [Google Scholar] [CrossRef]
- Inoue, M.; Sainoh, T.; Kojima, A.; Yamagata, M.; Morinaga, T.; Mannoji, C.; Ataka, H.; Yamashita, M.; Takahashi, H.; Saito, J. Efficacy and Safety of Condoliase Disc Administration as a New Treatment for Lumbar Disc Herniation. Spine Surg. Relat. Res. 2022, 6, 31–37. [Google Scholar] [CrossRef]
- Xiong, Z.; Yi, P.; Zhang, L.; Ma, H.; Li, W.; Tan, M. Efficacy and Safety of Modified Duhuo Jisheng Decoction in the Treatment of Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2020, 2020, 2381462. [Google Scholar] [CrossRef]
- Sun, K.; Liu, R. Genetic Predisposition of BMP7 Polymorphisms to Lumbar Disk Herniation in the Chinese Han Population. Cell Cycle 2024, 23, 466–477. [Google Scholar] [CrossRef]
- Doraisamy, R.; Ramaswami, K.; Shanmugam, J.; Subramanian, R.; Sivashankaran, B. Genetic Risk Factors for Lumbar Disc Disease. Clin. Anat. 2021, 34, 51–56. [Google Scholar] [CrossRef]
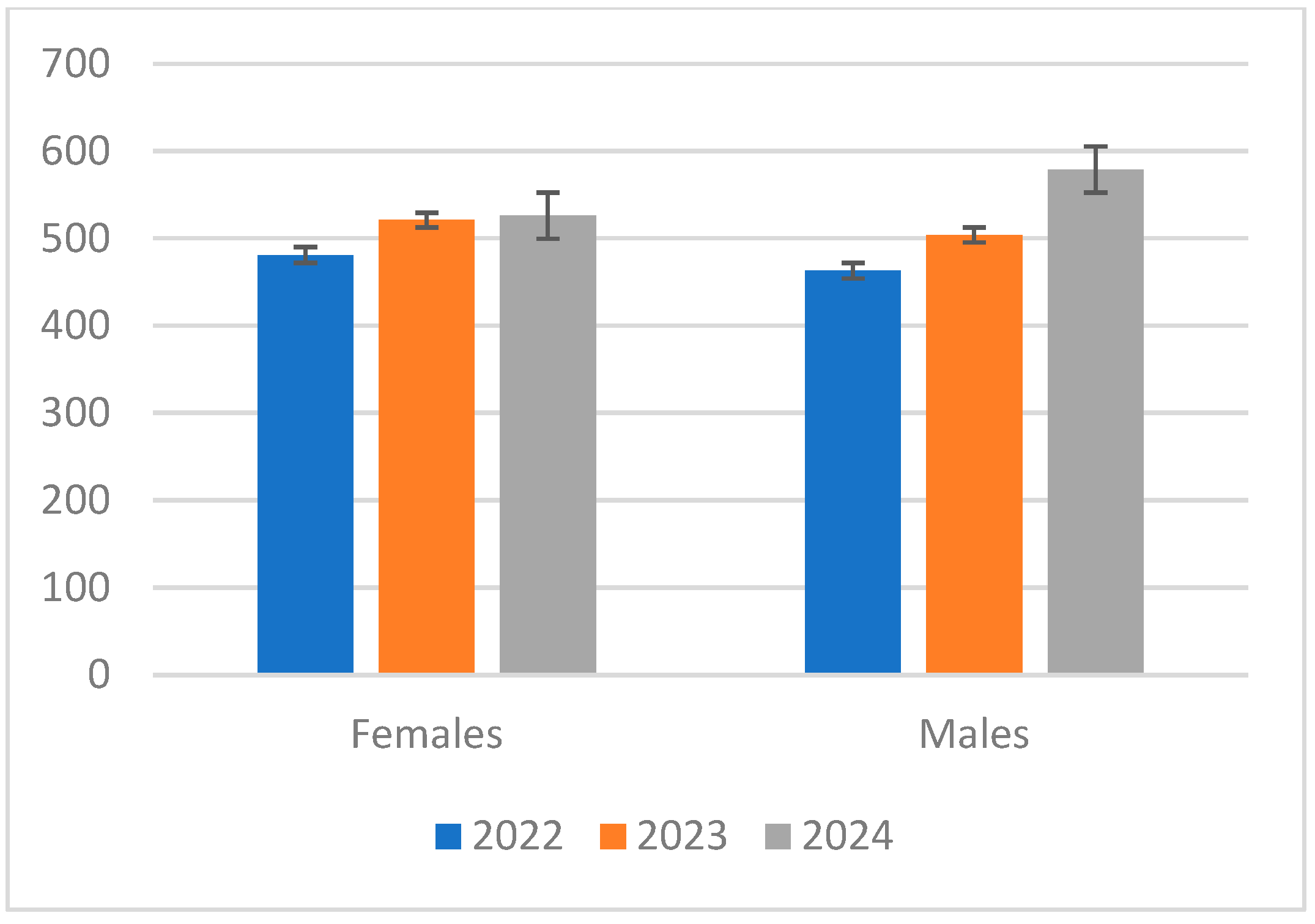


| Year | Females | Males | Mean (Females) | Mean (Males) | SD (Females) | SD (Males) |
|---|---|---|---|---|---|---|
| 2022 | 481 | 463 | 509.33 | 515.33 | 20.13 | 54.53 |
| 2023 | 521 | 504 | 509.33 | 515.33 | 20.13 | 54.53 |
| 2024 | 526 | 579 | 509.33 | 515.33 | 20.13 | 54.53 |
| Year | Decision | Ameliorated | Surgically Ameliorated | Stationary | Treated | Surgically Treated |
|---|---|---|---|---|---|---|
| 2022 | YES | 423 | 429 | 899 | 935 | 95 |
| NO | 521 | 515 | 899 | 935 | 95 | |
| 2023 | YES | 568 | 532 | 1074 | 1192 | 1023 |
| NO | 448 | 505 | 996 | 1018 | 999 | |
| 2024 | YES | 577 | 571 | 1018 | 1024 | - |
| NO | 569 | 583 | 1080 | 1156 | 1223 |
| Category | Mean | Median | Minimum | Maximum | Standard Deviation | Range | Coef (Decision) | p-Value | 95% Confidence Interval |
|---|---|---|---|---|---|---|---|---|---|
| Ameliorated | 516.33 | 525.5 | 423 | 577 | 9.98 | 154 | +10.00 | 0.878 | [−159.5, 179.5] |
| Surgically Ameliorated | 529.5 | 529 | 429 | 583 | 22.91 | 154 | −23.67 | 0.654 | [−159.5, 112.2] |
| Stationary | 1004.75 | 1006.5 | 899 | 1080 | 123.72 | 181 | +5.33 | 0.946 | [−198.6, 209.3] |
| Treated | 1027.25 | 1027 | 935 | 1192 | 118.49 | 257 | +14.00 | 0.895 | [−261.3, 289.3] |
| Surgically Treated | 1141 | 1099 | 95 | 1223 | 509.27 | 1128 | −213.33 | 0.730 | [−2007.2, 1580.6] |
| Diagnosis | 2022 Cases | 2023 Cases | 2024 Cases |
|---|---|---|---|
| Hypertension (HTA) | 144 | 353 | 355 |
| Cardiovascular diseases (including HTA) | 296 | 421 | 446 |
| Neurological disorders | 671 | 634 | 880 |
| Diabetes mellitus | 109 | 99 | 120 |
| Digestive diseases | 48 | 31 | 35 |
| Obesity | 142 | 137 | 131 |
| Osteoarticular diseases (including osteoporosis) | 89 | 60 | 99 |
| Tumor diseases | 38 | 25 | 47 |
| Hepatobiliary diseases | 47 | 62 | 50 |
| Endocrine diseases | 46 | 42 | 14 |
| Respiratory diseases | 42 | 41 | 63 |
| Kidney diseases | 21 | 22 | 137 |
| Other diseases | 26 | 79 | 102 |
| SARS-CoV-2 | 3 | 32 | 1 |
| Diagnosis | Mean Cases | Median Cases | Standard Deviation | Q1 (25th Percentile) | Q3 (75th Percentile) | p-Value | 95% Confidence Interval |
|---|---|---|---|---|---|---|---|
| Hypertension (HTA) | 284 | 318.5 | 87.11 | 179 | 335.75 | 0.030 | [67.6, 500.4] |
| Cardiovascular diseases (including HTA) | 387.67 | 404.33 | 57.31 | 318.92 | 412.67 | 0.007 | [245.3, 530.0] |
| Neurological disorders | 728.33 | 699.67 | 94.67 | 643.25 | 714 | 0.006 | [493.2, 963.5] |
| Diabetes Mellitus | 109.33 | 109.17 | 7.43 | 101.5 | 109.25 | 0.002 | [90.9, 127.8] |
| Digestive diseases | 38 | 36.5 | 6.32 | 32 | 37.25 | 0.009 | [22.3, 53.7] |
| Obesity | 136.67 | 136.83 | 3.9 | 132.42 | 136.92 | 0.0003 | [127.0, 146.4] |
| Osteoarticular diseases (including osteoporosis) | 82.67 | 85.83 | 14.39 | 65.67 | 87.42 | 0.010 | [46.9, 118.4] |
| Tumor diseases | 36.67 | 37.33 | 7.83 | 27.92 | 37.67 | 0.015 | [17.2, 56.1] |
| Hepatobiliary diseases | 53 | 51.5 | 5.65 | 47.75 | 52.25 | 0.004 | [39.0, 67.0] |
| Endocrine diseases | 34 | 38 | 12.46 | 19 | 40 | 0.042 | [3.0, 64.9] |
| Respiratory diseases | 48.67 | 45.33 | 8.91 | 41.25 | 47 | 0.011 | [26.5, 70.8] |
| Kidney diseases | 60 | 41 | 47.91 | 26.75 | 53.96 | 0.162 (not significant) | [−59.0, 179.0] |
| Other diseases | 69 | 74 | 27.65 | 37.99 | 76.5 | 0.050 (barely significant) | [0.3, 137.7] |
| SARS-CoV-2 | 12 | 7.5 | 12.43 | 4.13 | 12.22 | 0.236 (not significant) | [−18.9, 42.9] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duceac, M.; Guțu, C.; Pleșea-Condratovici, A.; Duceac, L.D.; Eva, L.; Dabija, M.G.; Elkan, E.-M.; Miftode, A.M.; Stefanache, A.; Dabija, V.-A.; et al. A Retrospective Study of Lumbar Disk Herniation: An Analysis of Clinical Cases and Treatment Plans. J. Clin. Med. 2025, 14, 3952. https://doi.org/10.3390/jcm14113952
Duceac M, Guțu C, Pleșea-Condratovici A, Duceac LD, Eva L, Dabija MG, Elkan E-M, Miftode AM, Stefanache A, Dabija V-A, et al. A Retrospective Study of Lumbar Disk Herniation: An Analysis of Clinical Cases and Treatment Plans. Journal of Clinical Medicine. 2025; 14(11):3952. https://doi.org/10.3390/jcm14113952
Chicago/Turabian StyleDuceac (Covrig), Mădălina, Cristian Guțu, Alina Pleșea-Condratovici, Letiția Doina Duceac, Lucian Eva, Marius Gabriel Dabija, Eva-Maria Elkan, Alina Monica Miftode, Alina Stefanache, Vlad-Andrei Dabija, and et al. 2025. "A Retrospective Study of Lumbar Disk Herniation: An Analysis of Clinical Cases and Treatment Plans" Journal of Clinical Medicine 14, no. 11: 3952. https://doi.org/10.3390/jcm14113952
APA StyleDuceac, M., Guțu, C., Pleșea-Condratovici, A., Duceac, L. D., Eva, L., Dabija, M. G., Elkan, E.-M., Miftode, A. M., Stefanache, A., Dabija, V.-A., Calin, G., & Voinescu, D. C. (2025). A Retrospective Study of Lumbar Disk Herniation: An Analysis of Clinical Cases and Treatment Plans. Journal of Clinical Medicine, 14(11), 3952. https://doi.org/10.3390/jcm14113952




.jpg)

