Comparative Arthroscopic Rotator Cuff Repair Outcomes Associated with Continuous Interscalene Block vs. Bolus Interscalene Block with Intravenous Dexmedetomidine: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Intraoperative Management and Surgical Technique
2.3. Interscalene Brachial Plexus Block Technique
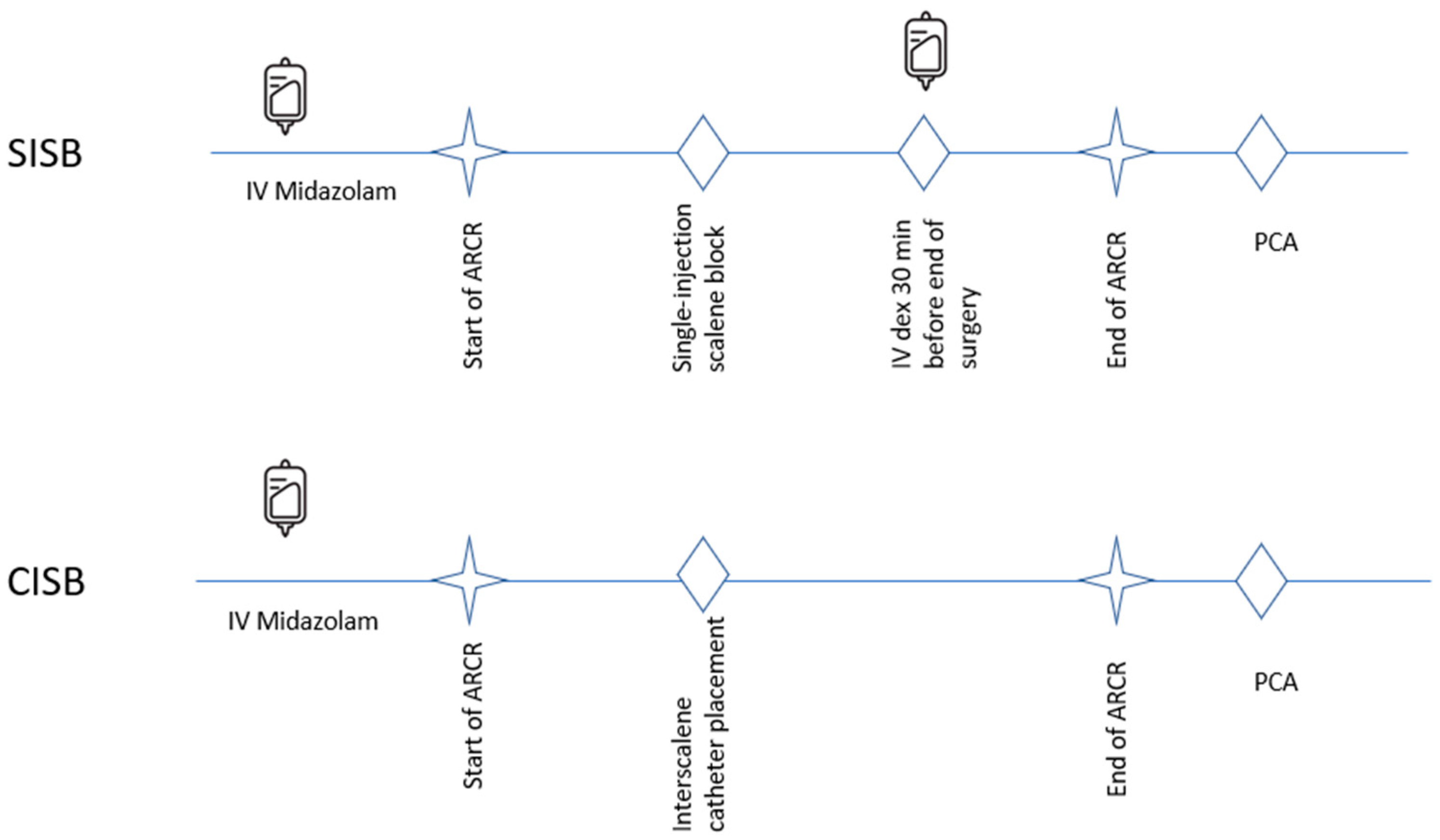
2.4. Continuous Interscalene Block Versus Single-Injection Interscalene Block with IV Dexmedetomidine
2.5. Patient Evaluations
2.6. Postoperative Management and Rehabilitation Protocol
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ARCR | Arthroscopic rotator cuff repair |
| CISB | Continuous interscalene block |
| IBPBB | Interscalene brachial plexus bolus blockade |
| IV | Intravenous |
| PCA | Patient-controlled analgesia |
| POD | Postoperative day |
| ROM | Range of motion |
| SISB | Single-injection interscalene block with intravenous dexmedetomidine |
| UCLA | University of California, Los Angeles |
| VAS | Visual analog scale |
References
- Ensor, K.L.; Kwon, Y.W.; Dibeneditto, M.R.; Zuckerman, J.D.; Rokito, A.S. The rising incidence of rotator cuff repairs. J. Shoulder Elb. Surg. 2013, 22, 1628–1632. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.; Cooper, C.; Campbell, M.K.; Rees, J.; Moser, J.; Beard, D.J.; Fitzpatrick, R.; Gray, A.; Dawson, J.; Murphy, J.; et al. Effectiveness of open and arthroscopic rotator cuff repair (UKUFF): A randomised controlled trial. Bone Jt. J. 2017, 99-B, 107–115. [Google Scholar] [CrossRef]
- Biz, C.; Vinanti, G.B.; Rossato, A.; Arnaldi, E.; Aldehheri, R. Prospective study of three surgical procedures for long head biceps tendinopathy associated with rotator cuff tears. Muscles Ligaments Tendons J. 2012, 2, 133–136. [Google Scholar] [PubMed]
- Swaika, S.; Parta, N.; Chattopadhyay, S.; Bisui, B.; Banarjee, S.S.; Chattarjee, S. Acomparative study of the efficacy of intravenous paracetamol and dexmedetomidine on perioperative hemodynamics and post-operative analgesia for patients undergoing laparoscopic cholecystectomy. Anesth. Essays Res. 2013, 7, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Toma, O.; Persoon, B.; Zahn, E.P.; Van de Velde, M.; Joshi, G.P.; PROSPECT Working Group Collaborators. PROSPECT guideline for rotator cuff repair surgery: Systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2019, 74, 1320–1331. [Google Scholar] [CrossRef]
- Chen, H.P.; Shen, S.J.; Tsai, H.I.; Kao, S.C.; Yu, H.P. Effects of interscalene nerve block for postoperative pain management in patients after shoulder surgery. Biomed. Res. Int. 2015, 2015, 902745. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Kim, T.; Kwon, Y.S.; Kang, H. Intra-operative effect of interscalene brachial plexus block to arthroscopic rotator cuff repair surgery. Int. Orthop. 2019, 43, 2117–2124. [Google Scholar] [CrossRef]
- Salviz, E.A.; Xu, D.; Frulla, A.; Kwofie, K.; Shastri, U.; Chen, J.; Shariat, A.N.; Littwin, S.; Lin, E.; Choi, J.; et al. Continuous interscalene block in patients having outpatient rotator cuff repair surgery: A prospective randomized trial. Anesth. Analg. 2013, 117, 1485–1492. [Google Scholar] [CrossRef]
- Abdallah, F.W.; Halper, S.H.; Aoyama, K.; Brull, R. Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth. Analg. 2015, 120, 1114–1129. [Google Scholar] [CrossRef]
- Fredrickson, M.J.; Ball, C.M.; Dalgleish, A.J. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg. Anesth. Pain Med. 2010, 35, 28–33. [Google Scholar] [CrossRef]
- Li, C.; Qu, J. Efficacy of dexmedetomidine for pain management in knee arthroscopy: A systematic review and meta-analysis. Medicine 2017, 96, e7938. [Google Scholar] [CrossRef]
- Terres, M.T.; Machado Assis, M.L.; Lombardi, R.A.; Balthazar da Silveira, C.; Amaral, S. Adding dexmedetomidine to intra-articular local anesthetics results in prolonged analgesia after knee arthroscopy: A systematic review and meta-analysis. Arthroscopy 2024, 41, 1061–1069. [Google Scholar] [CrossRef]
- Kang, R.A.; Jeong, J.S.; Yoo, J.C.; Lee, J.H.; Choi, S.J.; Gwak, M.S.; Hahm, T.S.; Huh, J.; Ko, J.S. Effective dose of intravenous dexmedetomidine to prolong the analgesic duration of interscalene brachial plexus block: A single-center, prospective, double-blind, randomized controlled trial. Reg. Anesth. Pain Med. 2018, 43, 488–495. [Google Scholar] [CrossRef]
- Hughes, M.S.; Matava, M.J.; Wright, R.W.; Brophy, R.H.; Smith, M.V. Interscalene brachial plexus block for arthroscopic shoulder surgery: A systematic review. J. Bone Jt. Surg. Am. 2013, 95, 1318–1324. [Google Scholar] [CrossRef]
- Kelly, B.C.; Constantinescu, D.S.; Vap, A.R. Arthroscopic and open or mini-open rotator cuff repair trends and complication rates among American Board of Orthopaedic Surgeons Part II Examinees (2007–2017). Arthroscopy 2019, 35, 3019–3024. [Google Scholar] [CrossRef]
- Moore, D.D.; Maerz, T.; Anderson, K. Shoulder surgeons’ perceptions of interscalene nerve blocks and a review of complications rates in the literature. Phys. Sportsmed. 2013, 41, 77–84. [Google Scholar] [CrossRef]
- Li, H.J.; Liu, S.; Geng, Z.Y.; Li, X.Y. Adding dexmedetomidine to morphine-based analgesia reduces early postoperative nausea in patients undergoing gynecological laparoscopic surgery: A randomized controlled trial. BMC Anesthesiol. 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, A.; Meyer-FrieBem, C.H.; Reichl, S.U.; Zahn, P.K.; Pogatzki-Zahn, E.M. Is intraoperative dexmedetomidine a new option for postoperative pain treatment? A meta-analysis of randomized controlled trials. Pain 2013, 154, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Gerlach, A.T.; Murphy, C.V.; Jones, G.M.; Cook, C.H. The relationship between dexmedetomidine dosing and hypotension. J. Trauma Acute Care Surg. 2012, 72, 799. [Google Scholar] [CrossRef]
- Li, Z.; Li, C.; Zhang, M. Effect of dexmedetomidine on hemodynamics in patients undergoing hysterectomy: A meta-analysis and systematic review. J. Int. Med. Res. 2021, 49, 3000605211039809. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A.; Hough, K.A.; Tsui, B.Y.; Ibinson, J.W.; Gold, M.S.; Gebhart, G.F. Neurotoxicity of adjuvants used in perineural anesthesia and analgesia in comparison with ropivacaine. Reg. Anesth. Pain Med. 2011, 36, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Borgeat, A.; Aguirre, J.; Curt, A. Case scenario: Neurologic complication after continuous interscalene block. Anesthesiology 2010, 112, 742–745. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.M.; Gray, A.T. Functional deficits after intraneural injection during interscalene block. Reg. Anesth. Pain Med. 2010, 35, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Byeon, G.J.; Shin, S.W.; Yoon, J.U.; Kim, E.J.; Baek, S.H.; Ri, H.S. Infusion methods for continuous interscalene brachial plexus block for postoperative pain control after arthroscopic rotator cuff repair. Korean J. Pain 2015, 28, 210–216. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kim, S.H.; So, K.Y.; Kim, D.J. Effects of interscalene brachial plexus block to intra-operative hemodynamics and postoperative pain for arthroscopic shoulder surgery. Korean J. Anesthesiol. 2012, 62, 30–34. [Google Scholar] [CrossRef]


| Postoperative Time (h) | Visual Analog Scale Score | ||
|---|---|---|---|
| SISB Group (n = 33) | CISB Group (n = 28) | p Value | |
| 2 | 1.6 ± 5.0 | 2.7 ± 4.5 | 0.716 |
| 12 | 5.8 ± 2.5 | 6.2 ± 2.1 | 0.618 |
| 36 | 4.5 ± 2.5 | 4.5 ± 2.2 | 0.940 |
| SISB Group (n = 33) | CISB Group (n = 28) | p Value | |
|---|---|---|---|
| Sleep disturbance due to pain | |||
| POD 1 | 14 (42.4%) | 18 (64.3%) | 0.148 |
| POD 2 | 19 (57.6%) | 18 (64.3%) | 0.786 |
| Anesthesia-related hypotension | 4 (12.1%) | 6 (21.4%) | 0.490 |
| Sensory disturbance | |||
| POD 1 | 1 (3.0%) | 3 (10.7%) | 0.434 |
| POD 2 | 0 (0.0%) | 3 (10.7%) | 0.715 |
| Nausea or vomiting | |||
| POD 1 | 1 (3.0%) | 3 (10.7%) | 0.241 |
| POD 2 | 0 (0.0%) | 3 (10.7%) | 0.226 |
| Preoperative | 3 Months Postoperative | 6 Months Postoperative | ||||
|---|---|---|---|---|---|---|
| Evaluation | SISB Group (n = 33) | CISB Group (n = 28) | SISB Group (n = 33) | CISB Group (n = 28) | SISB Group (n = 33) | CISB Group (n = 28) |
| UCLA | 18.4 ± 4.5 | 19.1 ± 3.9 | 26.4 ± 5.1 <0.0001 a | 25.2 ± 4.1 <0.0001 a | 30.3 ± 3.5 <0.0001 b 0.00030 c | 31.3 ± 3.8 <0.0001 b 0.0001 c |
| Constant | 43.3 ± 15.0 | 40.5 ± 15.2 | 79.3 ± 14.4 <0.0001 a | 74.3 ± 12.2 <0.0001 a | 87.6 ± 9.7 <0.0001 b 0.1042 c | 88.3 ± 10.2 <0.0001 b 0.0011 c |
| ROM: FF (degrees) | 170.0 ± 7.5 | 167.5 ± 5.9 | 175.7 ± 5.3 0.0009 a | 173.4 ± 4.9 0.0019 a | 178.2 ± 4.5 <0.0001 b 0.4745 | 177.1 ± 5.3 <0.0001 b 0.1480 |
| ROM: ABD (degrees) | 160.0 ± 6.4 | 165.0 ± 6.4 | 170.2 ± 5.8 <0.0001 a | 169.8 ± 5.1 0.0254 a | 177.6 ± 5.8 <0.0001 a <0.0001 b | 175.3 ± 4.7 <0.0001 a 0.0059 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, S.-M.; Lee, A.; Choi, S. Comparative Arthroscopic Rotator Cuff Repair Outcomes Associated with Continuous Interscalene Block vs. Bolus Interscalene Block with Intravenous Dexmedetomidine: A Retrospective Cohort Study. J. Clin. Med. 2025, 14, 3882. https://doi.org/10.3390/jcm14113882
Yoon S-M, Lee A, Choi S. Comparative Arthroscopic Rotator Cuff Repair Outcomes Associated with Continuous Interscalene Block vs. Bolus Interscalene Block with Intravenous Dexmedetomidine: A Retrospective Cohort Study. Journal of Clinical Medicine. 2025; 14(11):3882. https://doi.org/10.3390/jcm14113882
Chicago/Turabian StyleYoon, Seong-Meen, Aeryoung Lee, and Sungwook Choi. 2025. "Comparative Arthroscopic Rotator Cuff Repair Outcomes Associated with Continuous Interscalene Block vs. Bolus Interscalene Block with Intravenous Dexmedetomidine: A Retrospective Cohort Study" Journal of Clinical Medicine 14, no. 11: 3882. https://doi.org/10.3390/jcm14113882
APA StyleYoon, S.-M., Lee, A., & Choi, S. (2025). Comparative Arthroscopic Rotator Cuff Repair Outcomes Associated with Continuous Interscalene Block vs. Bolus Interscalene Block with Intravenous Dexmedetomidine: A Retrospective Cohort Study. Journal of Clinical Medicine, 14(11), 3882. https://doi.org/10.3390/jcm14113882






