Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty a Nationwide Analysis and the Case for Preoperative Screening
Abstract
1. Introduction
Research Question
2. Methods
2.1. Dataset
2.2. Patient Identification and Exclusions
2.3. Statistical Analyses and Propensity Score Matching
2.4. Comorbidity and Outcome Identification
2.5. Revision Surgery Analysis
2.6. Cost Analysis of Universal Preoperative Urine Opioid Screening
2.7. Ethical Aspects
3. Results
3.1. A Propensity Score-Matched Evaluation of Total Knee Arthroplasty Outcomes in Patients with Versus Without Opioid Use Disorder
3.2. Inpatient Outcomes Among Matched TKA Patients With and Without Opioid Use Disorder
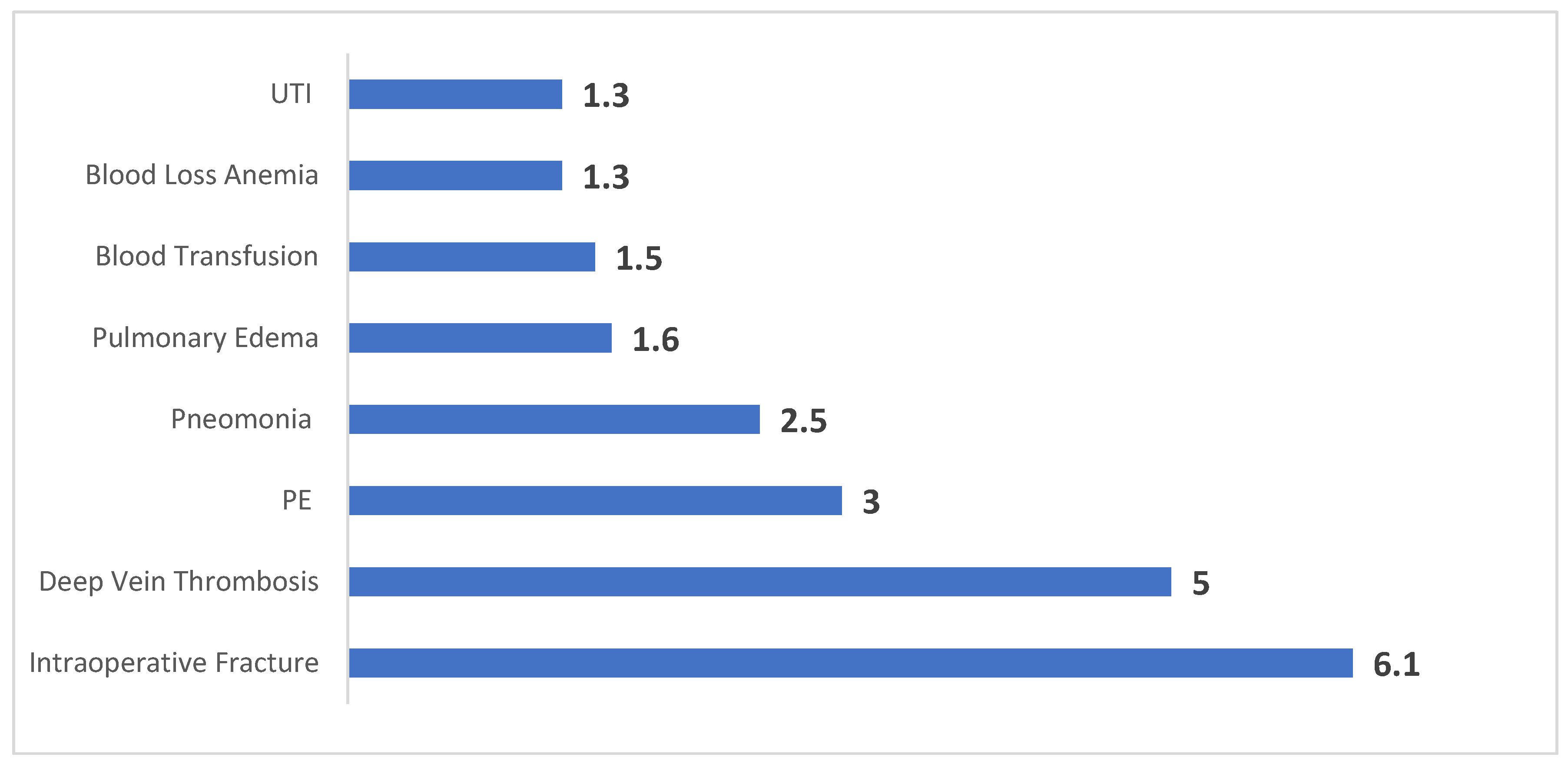
3.3. Elevated Postoperative Complications in Opioid Use Disorder Patients Undergoing TKA
3.4. Revision TKA Outcomes in Patients With and Without Opioid Use Disorder
3.5. Primary Reasons for Revision TKA Among Patients With and Without Opioid Use Disorder
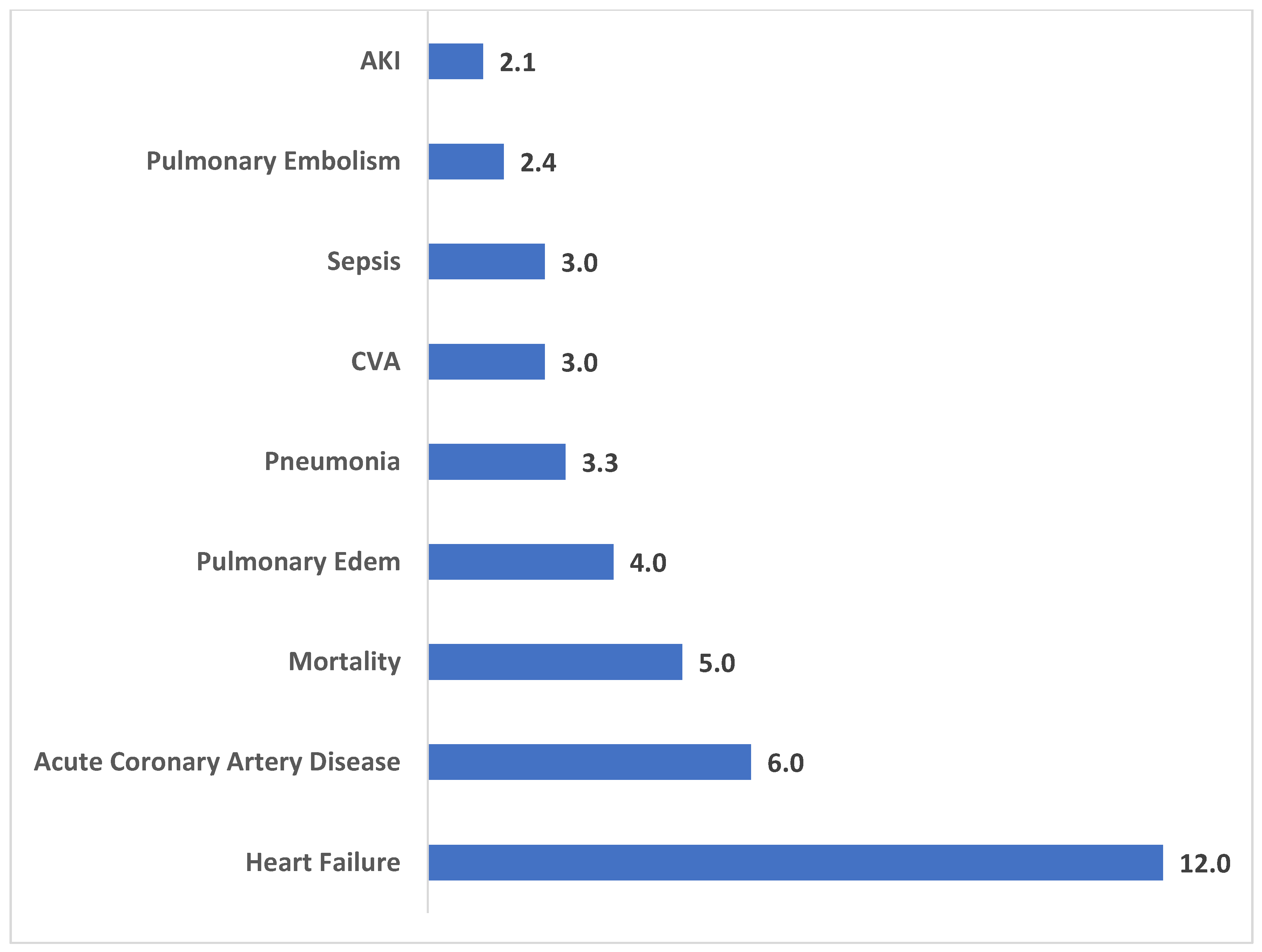
3.6. Postoperative Complications Following Revision TKA in Patients With and Without Opioid Use Disorder
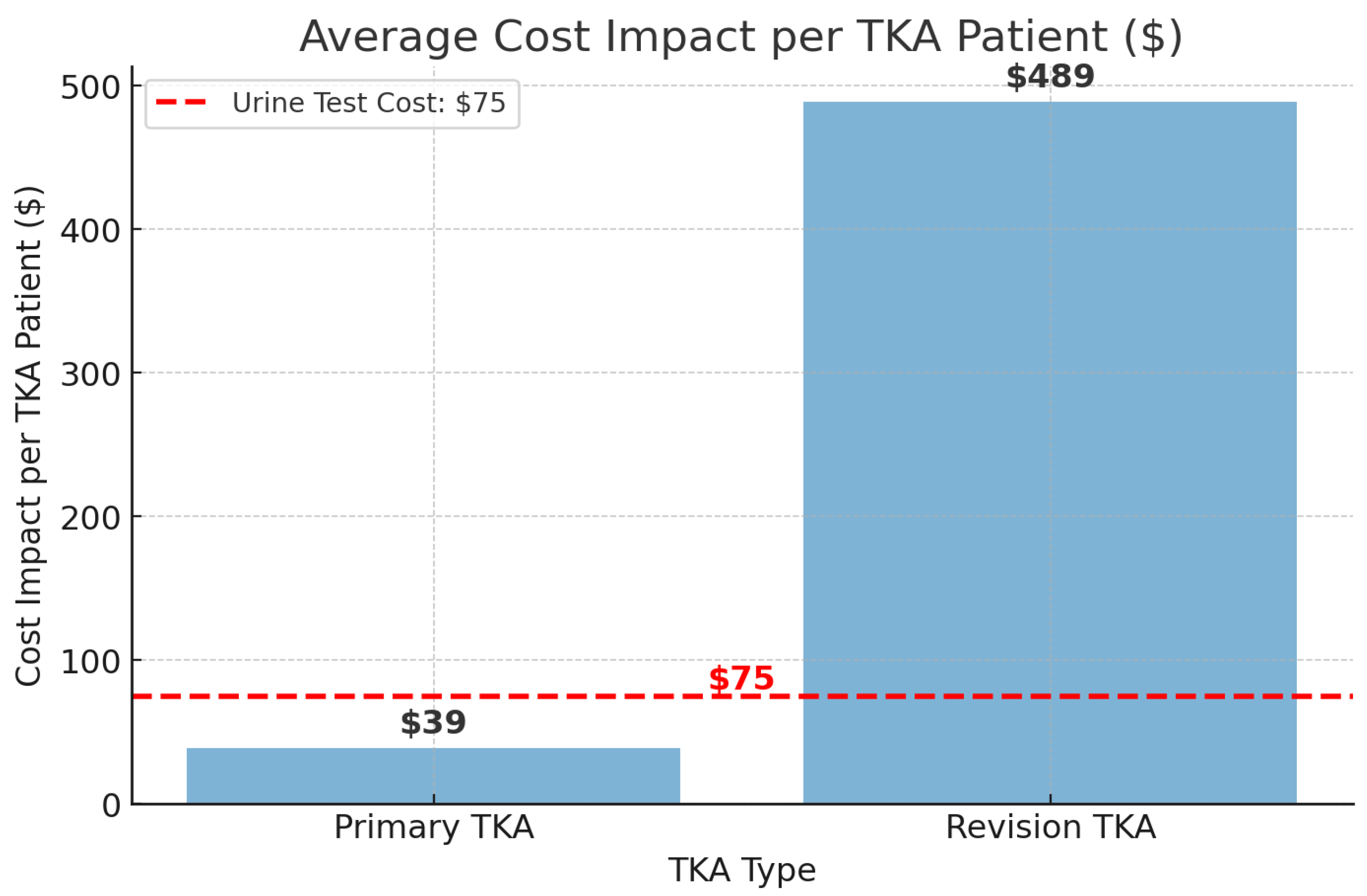
3.7. Cost Impact of Opioid Use Disorder on TKA and the Potential Savings of Preoperative Screening
4. Discussion
4.1. Key Findings and Clinical Implications
4.2. Under-Reporting of OUD in Preoperative Screening
4.3. Increased Postoperative Complications and Healthcare Costs
4.4. Increased Risk of Intraoperative Fracture
4.5. Reoperations and Extended Postoperative Outcomes
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AKI | Acute Kidney Injury |
| DVT | Deep Vein Thrombosis |
| HMO | Health Maintenance Organization |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LOS | Length of Stay |
| NIS | Nationwide Inpatient Sample |
| OUD | opioid use disorder |
| PE | Pulmonary Embolism |
| TKA | Total Knee Arthroplasty |
References
- Singh, M.; Harary, J.; Schilling, P.L.; Moschetti, W.E. Patient Satisfaction Is Nearly 90% After Total Knee Arthroplasty; We Are Better Than We Were. J. Arthroplast. 2025, 40, 1521–1525.e1. [Google Scholar] [CrossRef] [PubMed]
- Christensen, T.H.; Rondon, A.J.; Vasquez, V.; Parvizi, J. Opioid Use During Hospitalization Following Total Knee Arthroplasty: Trends in Consumption from 2016 to 2021. J. Arthroplast. 2023, 38, S26–S31. [Google Scholar] [CrossRef] [PubMed]
- Moghadam, S.A.G.; Norouzi, M.; Vafaei, A.; Riazi, S.; Ghodraty, M.R. Comparing Apotel and Remifentanil for Multimodal Patient-Controlled Analgesia in Postoperative Pain Management Following Total Knee Arthroplasty Surgery: A Randomized Controlled Trial. Anesthesiol. Pain Med. 2024, 14, e141975. [Google Scholar] [CrossRef]
- Koh, H.J.; Park, J.; Lee, D.H.; Park, J.S. Does Central Sensitization Affect Hyperalgesia After Staged Bilateral Total Knee Arthroplasty? A Randomized Controlled Trial. J. Int. Med. Res. 2020, 48, 0300060520938934. [Google Scholar] [CrossRef]
- Liu, N.; Xu, Y.; Wang, Q.; Zhang, M.; Zhang, Z. Combining Various Acupuncture Therapies with Multimodal Analgesia to Enhance Postoperative Pain Management Following Total Knee Arthroplasty: A Network Meta-Analysis of Randomized Controlled Trials. Front. Neurol. 2024, 15, 1361037. [Google Scholar] [CrossRef]
- Wixson, R.L.; Johnson, A.R.; Orozco, F.R.; Davis, K.E.; Colman, M.W. Pain and Opioid Use Following Total Knee Arthroplasty: Psycho-Social Factors Are More Predictive Than Pharmacogenomics. J. Arthroplast. 2024, 39, 1214–1219. [Google Scholar] [CrossRef]
- Kaidi, A.C.; Fritz, B.T.; Malpani, R.; Brundage, T.S.; Jella, T.K.; Sochacki, K.R.; Hevesi, M.; Barlow, D.R. Opioid Prescription Consumption Patterns After Total Joint Arthroplasty in Chronic Opioid Users Versus Opioid Naive Patients. JAAOS Glob. Res. Rev. 2020, 4, e20. [Google Scholar] [CrossRef]
- Hyland, S.J.; Brockhaus, K.K.; Vincent, W.R.; Spence, N.Z.; Lucki, M.M.; Howkins, M.J.; Cleary, R.K. Perioperative Pain Management and Opioid Stewardship: A Practical Guide. Healthcare 2021, 9, 333. [Google Scholar] [CrossRef]
- Smith, S.R.; Hooten, W.M.; Hanson, A.C.; Warner, D.O. Impact of Preoperative Opioid Use on Total Knee Arthroplasty Outcomes. J. Bone Jt. Surg. Am. 2017, 99, 803–808. [Google Scholar] [CrossRef]
- Blevins Peratikos, M.; Tippens, K.M.; Kelley, T.C.; Edwards, P.K.; Barnes, C.L. Effect of Preoperative Opioid Use on Adverse Outcomes, Medical Spending, and Persistent Opioid Use Following Elective Total Joint Arthroplasty in the United States: A Large Retrospective Cohort Study of Administrative Claims Data. Pain Med. 2020, 21, 521–531. [Google Scholar] [CrossRef]
- Jain, N.; Brock, J.L.; Malik, A.T.; Phillips, F.M.; Khan, S.N. Prediction of Complications, Readmission, and Revision Surgery Based on Duration of Preoperative Opioid Use: Analysis of Major Joint Replacement and Lumbar Fusion. J. Bone Jt. Surg. Am. 2019, 101, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, K.; Shover, C.L.; Andrews, C.M.; Bohnert, A.S.B.; Brandeau, M.L.; Caulkins, J.P.; Chen, J.H.; Cuéllar, M.-F.; Hurd, Y.L.; Juurlink, D.N.; et al. Responding to the Opioid Crisis in North America and Beyond: Recommendations of the Stanford–Lancet Commission. Lancet 2022, 399, 555–604. [Google Scholar] [CrossRef] [PubMed]
- González-Roz, A.; Martínez-Loredo, V.; Aston, E.R.; Metrik, J.; Murphy, J.; Balodis, I.; Secades-Villa, R.; Belisario, K.; MacKillop, J. The Opioid Epidemic: A Worldwide Exploratory Study Using the WHO Pharmacovigilance Database. Addiction 2023, 118, 771–775. [Google Scholar] [CrossRef]
- Yeo, Y.; Johnson, R.; Heng, C. The Public Health Approach to the Worsening Opioid Crisis in the United States Calls for Harm Reduction Strategies to Mitigate the Harm from Opioid Addiction and Overdose Deaths. Mil. Med. 2022, 187, 244–247. [Google Scholar] [CrossRef]
- Krawczyk, N.; Rivera, B.D.; Jent, V.; Keyes, K.M.; Jones, C.M.; Cerdá, M. Has the Treatment Gap for Opioid Use Disorder Narrowed in the U.S.?: A Yearly Assessment from 2010 to 2019. Int. J. Drug Policy 2022, 110, 103786. [Google Scholar] [CrossRef]
- Wilson, J.M.; Hannon, C.P.; Fillingham, Y.A.; Della Valle, C.J. Preoperative Opioid Use Is a Risk Factor for Complication and Increased Healthcare Utilization Following Revision Total Knee Arthroplasty. Knee 2020, 27, 1121–1127. [Google Scholar] [CrossRef]
- Kim, K.; Bhave, A.; Geller, J.A. Preoperative Chronic Opioid Use and Its Effects on Total Knee Arthroplasty Outcomes. J. Knee Surg. 2020, 33, 306–313. [Google Scholar] [CrossRef]
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef]
- Maman, D.; Fournier, L.; Steinfeld, Y.; Berkovich, Y. Etiology, Outcomes, and Complications of Total Hip Arthroplasty in Younger Patients: A Nationwide Big Data Analysis. J. Clin. Med. 2024, 13, 4535. [Google Scholar] [CrossRef]
- Pagan, D.N.; Hernandez, V.H.; Reddy, G.B.; D’Apuzzo, M.R. Chronic Opioid Use Independently Increases Complications and Resource Utilization After Primary Total Joint Arthroplasty. J. Arthroplast. 2023, 38, 1004–1009. [Google Scholar] [CrossRef]
- Bogler, O.; Incze, M.A. Endocrine Adverse Effects of Long-Term Opioid Use. JAMA Intern. Med. 2024, 184, 831–832. [Google Scholar] [CrossRef] [PubMed]
- Karavitaki, N.; Boguszewski, C.L.; Colao, A.; Cundy, T.; Danese, M.D.; Fleseriu, M.; Gadelha, M.R.; Ghigo, E.; Shalet, S.M.; Veldhuis, J.D. Exogenous Opioids and the Human Endocrine System: An Endocrine Society Scientific Statement. Endocr. Rev. 2024, 45, 773–794. [Google Scholar] [CrossRef] [PubMed]
- Shichman, I.; Roof, M.; Askew, N.; Nherera, L.; Rozell, J.C.; Seyler, T.M.; Schwarzkopf, R. Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040–2060. JBJS Open Access 2023, 8, e22.00112. [Google Scholar] [CrossRef]
- Bali, B.; Wise, J.L.; Batki, S.L.; Cohn, T.J.; Kanaya, A.M.; Wiebe, D.J.; Flanagan, C.A. Assessing Men with Opioid Use Disorder for Testosterone Deficiency after the Development of Symptoms. J. Addict. Dis. 2024, 43, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Xing, D.; Dong, S.; Lin, J. The Primary Total Knee Arthroplasty: A Global Analysis. J. Orthop. Surg. Res. 2020, 15, 190. [Google Scholar] [CrossRef]
| Clinical Variable | No Opioid Use Disorder | Opioid Use Disorder | p-Value |
|---|---|---|---|
| Total Procedures | 2,502,314 (99.5%) | 11,785 (0.5%) | - |
| Mean Patient Age (years) | 66.8 | 61.3 | <0.001 |
| Female Sex (%) | 61.6 | 60.6 | 0.034 |
| Insurance Type—Medicare (%) | 57.1 | 54.4 | <0.001 |
| Insurance Type—Medicaid (%) | 4.2 | 15.1 | |
| Insurance Type—Private/HMO (%) | 35.1 | 26.1 | |
| Insurance Type—Self-pay (%) | 0.5 | 0.3 | |
| Insurance Type—No Charge (%) | 0 | 0 | |
| Insurance Type—Other (%) | 3.1 | 4.0 | |
| Hypertensive Disease (%) | 59.6 | 57.1 | <0.001 |
| Lipid Metabolism Disorders (%) | 46.7 | 38.5 | <0.001 |
| Sleep Apnea Syndrome (%) | 13.2 | 16.5 | <0.001 |
| Chronic Blood Loss Anemia (%) | 5.8 | 7.7 | <0.001 |
| Alcohol Use Disorder (%) | 0.9 | 4.8 | <0.001 |
| Fragility Fracture Risk (Osteoporosis) (%) | 4.0 | 4.5 | <0.001 |
| Parkinsonian Syndromes (%) | 0.6 | 0.6 | 0.825 |
| Neurocognitive Disorders (%) | 0.2 | 0.2 | 0.978 |
| Renal Dysfunction (%) | 6.9 | 10.0 | <0.001 |
| Congestive Cardiac Failure (%) | 1.2 | 2.0 | <0.001 |
| Chronic Pulmonary Disease (%) | 5.9 | 14.7 | <0.001 |
| Prior Myocardial Infarction (%) | 3.1 | 3.8 | <0.001 |
| Diabetes (any type) (%) | 21.7 | 22.5 | 0.022 |
| Hepatic Dysfunction (%) | 1.2 | 4.3 | <0.001 |
| Fibromyalgia Diagnosis (%) | 2.7 | 11.2 | <0.001 |
| Endocrine—Thyroid Disorders (%) | 17.9 | 18.4 | 0.825 |
| Clinical Variable | No Opioid Use Disorder | Opioid Use Disorder | p-Value |
|---|---|---|---|
| Total Procedures | 11,785 | 11,785 | - |
| Mean Patient Age (years) | 61.3 | 61.3 | p = 0.59 |
| Female Sex (%) | 61.1 | 60.6 | p = 0.51 |
| Insurance Type—Medicare (%) | 54.8 | 54.4 | p = 0.91 |
| Insurance Type—Medicaid (%) | 14.7 | 15.1 | |
| Insurance Type—Private/HMO (%) | 26.3 | 26.1 | |
| Insurance Type—Self-pay (%) | 0.3 | 0.3 | |
| Insurance Type—No Charge (%) | 0 | 0 | |
| Insurance Type—Other (%) | 3.9 | 4 | |
| Hypertensive Disease (%) | 57.7 | 57.1 | p = 0.36 |
| Lipid Metabolism Disorders (%) | 37.8 | 38.5 | p = 0.28 |
| Sleep Apnea Syndrome (%) | 16.5 | 16.5 | p = 0.93 |
| Chronic Blood Loss Anemia (%) | 7.7 | 7.7 | p = 0.99 |
| Alcohol Use Disorder (%) | 4 | 4.8 | p = 0.20 |
| Fragility Fracture Risk (Osteoporosis) (%) | 4.5 | 4.5 | p = 1 |
| Parkinsonian Syndromes (%) | 0.6 | 0.6 | p = 0.86 |
| Neurocognitive Disorders (%) | 0.2 | 0.2 | p = 1 |
| Renal Dysfunction (%) | 9.6 | 10 | p = 0.33 |
| Congestive Cardiac Failure (%) | 1.8 | 2 | p = 0.46 |
| Chronic Pulmonary Disease (%) | 13.9 | 14.7 | p = 0.08 |
| Prior Myocardial Infarction (%) | 3.4 | 3.8 | p = 0.12 |
| Diabetes (any type) (%) | 23.2 | 22.5 | p = 0.16 |
| Hepatic Dysfunction (%) | 3.8 | 4.3 | p = 0.38 |
| Fibromyalgia Diagnosis (%) | 10.4 | 11.2 | p = 0.10 |
| Endocrine—Thyroid Disorders (%) | 17.9 | 18.4 | p = 0.07 |
| No Opioid Use Disorder | Opioid Use Disorder | p Value | |
|---|---|---|---|
| Mean LOS in days | 2.5 (S.D 1.0) | 2.8 (S.D 3.0) | p < 0.001 |
| mean charges in $ | 60,984 (S.D 36,232) | 68,687 (S.D 41472) | p < 0.001 |
| Revision Surgery | No Opioid Use Disorder | Opioid Use Disorder | Significance |
|---|---|---|---|
| Total numbers | 220,215 (98.6%) | 3030 (1.4%) | |
| Age at Revision (Years) | 65.4 (Std Deviation 10.4) | 59.6 (Std Deviation 10.2) | p = 0.016 |
| Total charges (USD) | 97,346 (Std Deviation 76,718) | 132,257 (Std Deviation 413,396) | p < 0.001 |
| Length of stay (Days) | 3.1 (Std Deviation 2.8) | 4.4 (Std Deviation 5.2) | p < 0.001 |
| Etiology for Revision | No Opioid Use Disorder | Opioid Use Disorder | |
|---|---|---|---|
| Infection | 22.1% | 32.3% | p < 0.001 |
| Mechanical Loosening | 23.0% | 19.0% | |
| Pain | 7.4% | 5.6% | |
| Instability of Prosthesis | 12.1% | 10.1% | |
| Wear of Articular Surface | 2.1% | 1.5% | |
| Periprosthetic Fracture | 0.9% | 0.2% | |
| Fibrosis due to Prosthetic | 0.9% | 0.7% | |
| Broken Prosthesis | 1.1% | 0.7% | |
| Wound complication | 0.4% | 0.3% | |
| Mechanical Complication | 9.5% | 8.9% | |
| Other/Unspecified | 20.6% | 20.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen Nissan, E.; Berkovich, Y.; Maman, D.; Yonai, Y.; Steinfeld, Y.; Berkovich, Y. Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty a Nationwide Analysis and the Case for Preoperative Screening. J. Clin. Med. 2025, 14, 3832. https://doi.org/10.3390/jcm14113832
Cohen Nissan E, Berkovich Y, Maman D, Yonai Y, Steinfeld Y, Berkovich Y. Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty a Nationwide Analysis and the Case for Preoperative Screening. Journal of Clinical Medicine. 2025; 14(11):3832. https://doi.org/10.3390/jcm14113832
Chicago/Turabian StyleCohen Nissan, Ela, Yaara Berkovich, David Maman, Yaniv Yonai, Yaniv Steinfeld, and Yaron Berkovich. 2025. "Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty a Nationwide Analysis and the Case for Preoperative Screening" Journal of Clinical Medicine 14, no. 11: 3832. https://doi.org/10.3390/jcm14113832
APA StyleCohen Nissan, E., Berkovich, Y., Maman, D., Yonai, Y., Steinfeld, Y., & Berkovich, Y. (2025). Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty a Nationwide Analysis and the Case for Preoperative Screening. Journal of Clinical Medicine, 14(11), 3832. https://doi.org/10.3390/jcm14113832






