Differences in Spinal Posture and Movement Between Adult Females with Anorexia Nervosa and Age- and Sex-Matched Normal-Weight Controls
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.3. Data Processing
2.4. Statistical Analysis
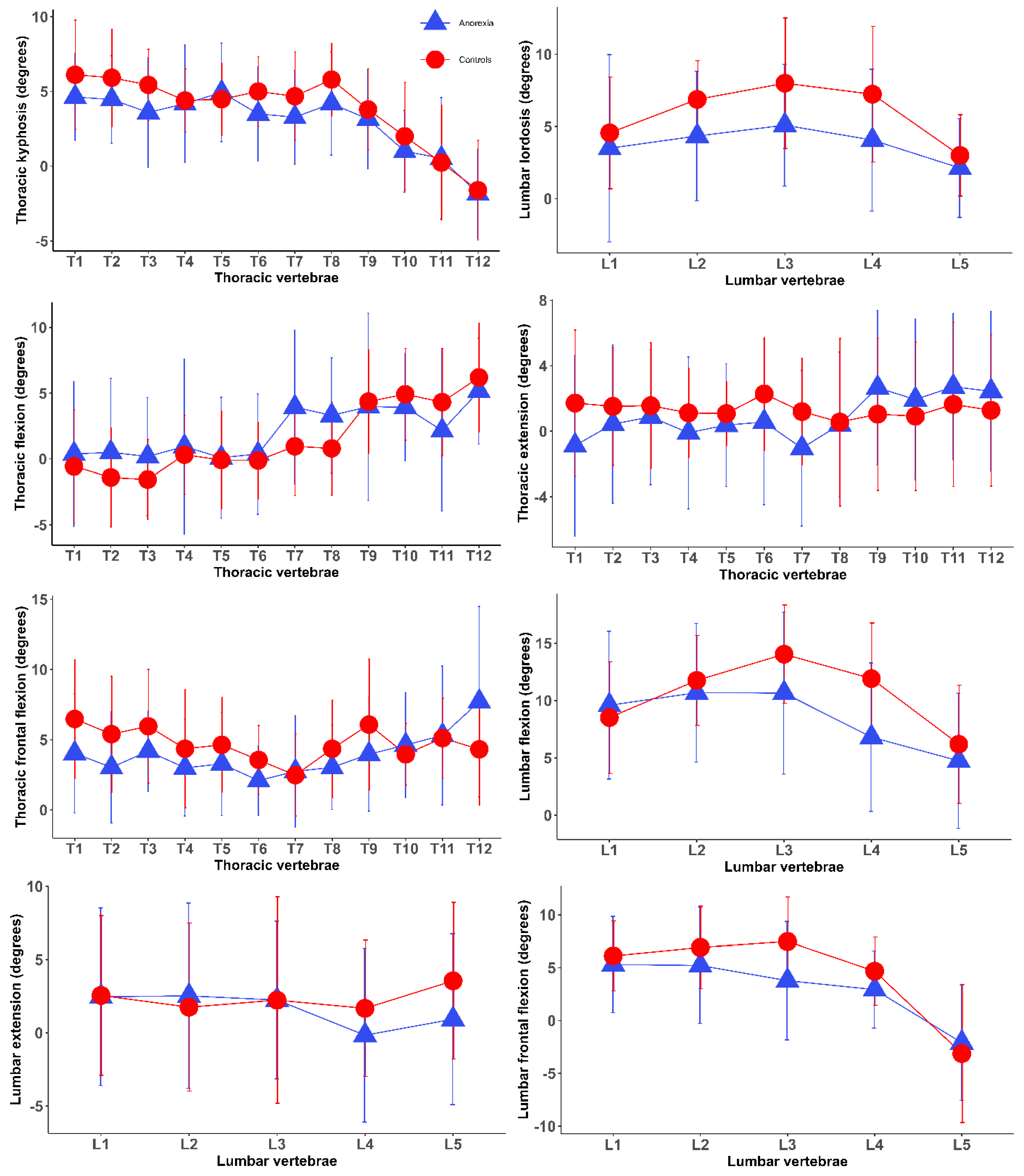
3. Results
Relationships Between Anorexia Nervosa Characteristics and Spinal Posture and Movements
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van Hoeken, D.; Hoek, H.W. Review of the burden of eating disorders: Mortality, disability, costs, quality of life, and family burden. Curr. Opin. Psychiatry 2020, 33, 521–527. [Google Scholar] [CrossRef] [PubMed]
- van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, A.A.; Gordon, C.M. Skeletal complications of eating disorders. Metab. Clin. Exp. 2015, 64, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Rosas Pereira, A.; Costa, M.; Costa, G.G.; Carvalho, A.S. Anorexia Nervosa and Osteoporosis: A Possible Complication to Remember. Cureus 2024, 16, e52670. [Google Scholar] [CrossRef]
- Minano Garrido, E.; Di Lodovico, L.; Dicembre, M.; Duquesnoy, M.; Ohanyan, H.; Melchior, J.C.; Hanachi, M. Evaluation of muscle-skeletal strength and peak expiratory flow in severely malnourished inpatients with anorexia nervosa: A pilot study. Nutrition 2021, 85, 111133. [Google Scholar] [CrossRef]
- Schmerler, J.; Chiu, A.K.; Agarwal, A.R.; Kreulen, R.T.; Srikumaran, U.; Best, M.J. Increased prevalence of lower extremity soft tissue injuries and surgeries in patients with anorexia nervosa and bulimia nervosa. Phys. Sportsmed. 2024, 52, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Rosa-Caldwell, M.E.; Eddy, K.T.; Rutkove, S.B.; Breithaupt, L. Anorexia nervosa and muscle health: A systematic review of our current understanding and future recommendations for study. Int. J. Eat. Disord. 2023, 56, 483–500. [Google Scholar] [CrossRef]
- Minano-Garrido, E.J.; Catalan-Matamoros, D.; Gómez-Conesa, A. Physical Therapy Interventions in Patients with Anorexia Nervosa: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13921. [Google Scholar] [CrossRef]
- Kolnes, L.J. Embodying the body in anorexia nervosa--a physiotherapeutic approach. J. Bodyw. Mov. Ther. 2012, 16, 281–288. [Google Scholar] [CrossRef]
- Quesnel, D.A.; Cooper, M.; Fernandez-Del-Valle, M.; Reilly, A.; Calogero, R.M. Medical and physiological complications of exercise for individuals with an eating disorder: A narrative review. J. Eat. Disord. 2023, 11, 3. [Google Scholar] [CrossRef]
- Bayartai, M.E.; Luomajoki, H.; Tringali, G.; De Micheli, R.; Abbruzzese, L.; Sartorio, A. Differences in spinal posture and mobility between adults with obesity and normal weight individuals. Sci. Rep. 2023, 13, 13409. [Google Scholar] [CrossRef] [PubMed]
- Bayartai, M.E.; Luomajoki, H.; Tringali, G.; De Micheli, R.; Grugni, G.; Sartorio, A. Differences in spinal postures and mobility among adults with Prader-Willi syndrome, essential obesity, and normal-weight individuals. Front. Endocrinol. 2023, 14, 1235030. [Google Scholar] [CrossRef] [PubMed]
- Livanelioglu, A.; Kaya, F.; Nabiyev, V.; Demirkiran, G.; Fırat, T. The validity and reliability of “Spinal Mouse” assessment of spinal curvatures in the frontal plane in pediatric adolescent idiopathic thoraco-lumbar curves. Eur. Spine J. 2016, 25, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef]
- Bayartai, M.E.; Schaer, C.E.; Luomajoki, H.; Tringali, G.; De Micheli, R.; Sartorio, A. Differences in spinal posture and mobility between children/adolescents with obesity and age-matched normal-weight individuals. Sci. Rep. 2022, 12, 15570. [Google Scholar] [CrossRef]
- Kellis, E.; Adamou, G.; Tzilios, G.; Emmanouilidou, M. Reliability of spinal range of motion in healthy boys using a skin-surface device. J. Manip. Physiol. Ther. 2008, 31, 570–576. [Google Scholar] [CrossRef]
- Nouh, M.R. Imaging of the spine: Where do we stand? World J. Radiol. 2019, 11, 55–61. [Google Scholar] [CrossRef]
- Guermazi, M.; Ghroubi, S.; Kassis, M.; Jaziri, O.; Keskes, H.; Kessomtini, W.; Ben Hammouda, I.; Elleuch, M.H. Validity and reliability of Spinal Mouse to assess lumbar flexion. Ann. Readapt. Med. Phys. 2006, 49, 172–177. [Google Scholar] [CrossRef]
- Lukaski, H.C. Methods for the assessment of human body composition: Traditional and new. Am. J. Clin. Nutr. 1987, 46, 537–556. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Hasegawa, K. Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur. Spine J. 2016, 25, 3630–3637. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Length, R. emmeans: Estimated Marginal Means, aka Least-Squares Means, R package version 1.6.3.; CRAN: Windhoek, Namibia, 2021.
- Misra, M.; Aggarwal, A.; Miller, K.K.; Almazan, C.; Worley, M.; Soyka, L.A.; Herzog, D.B.; Klibanski, A. Effects of anorexia nervosa on clinical, hematologic, biochemical, and bone density parameters in community-dwelling adolescent girls. Pediatrics 2004, 114, 1574–1583. [Google Scholar] [CrossRef] [PubMed]
- Faje, A.T.; Karim, L.; Taylor, A.; Lee, H.; Miller, K.K.; Mendes, N.; Meenaghan, E.; Goldstein, M.A.; Bouxsein, M.L.; Misra, M.; et al. Adolescent Girls With Anorexia Nervosa Have Impaired Cortical and Trabecular Microarchitecture and Lower Estimated Bone Strength at the Distal Radius. J. Clin. Endocrinol. Metab. 2013, 98, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
- Castillo, E.R.; Lieberman, D.E. Shock attenuation in the human lumbar spine during walking and running. J. Exp. Biol. 2018, 221, 177949. [Google Scholar] [CrossRef] [PubMed]
- Barrey, C.; Roussouly, P.; Le Huec, J.C.; D’Acunzi, G.; Perrin, G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur. Spine J. 2013, 22 (Suppl. 6), S834–S841. [Google Scholar] [CrossRef]
- Probst, M.; Majeweski, M.L.; Albertsen, M.N.; Catalan-Matamoros, D.; Danielsen, M.; De Herdt, A.; Duskova Zakova, H.; Fabricius, S.; Joern, C.; Kjölstad, G.; et al. Physiotherapy for patients with anorexia nervosa. Adv. Eat. Disord. 2013, 1, 224–238. [Google Scholar] [CrossRef]
- Lu, D.C.; Chou, D. Flatback syndrome. Neurosurg. Clin. N. Am. 2007, 18, 289–294. [Google Scholar] [CrossRef]
- Sadler, S.G.; Spink, M.J.; Ho, A.; De Jonge, X.J.; Chuter, V.H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 2017, 18, 179. [Google Scholar] [CrossRef]
- Bruno, A.G.; Anderson, D.E.; D’Agostino, J.; Bouxsein, M.L. The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J. Bone Min. Res. 2012, 27, 2144–2151. [Google Scholar] [CrossRef]

| Variables | Individuals with Anorexia Nervosa (n = 32) | Normal-Weight Controls (n = 25) | p-Value |
|---|---|---|---|
| Age (years) | 27.7 (9.9) | 27.5 (9.3) | 0.83 W |
| Weight (kg) | 37.1 (5.6) | 62.8 (6.6) | <0.0001 W |
| Height (cm) | 161.2 (6.7) | 167.0 (6.4) | 0.82 W |
| BMI (kg/m2) | 14.3 (1.8) | 22.5 (2.2) | 0.002 W |
| Fat mass (kg) | 4.1 (1.9) | 15.6 (5.7) | <0.0001 W |
| Fat-free mass (%) | 89.2 (4.9) | 75.2 (8.9) | <0.0001 W |
| Variables | Anorexia Nervosa n = 32 | Normal-Weight Controls n = 25 | Differences in Spinal Posture and Mobility (95% CI) | p-Value | ||
|---|---|---|---|---|---|---|
| EMM | SE | EMM | SE | |||
| Spinal postures | ||||||
| Thoracic kyphosis (Th1-12) | 37.5 | 2.1 | 46.3 | 2.3 | −8.8 (−15.2 to −2.4) | 0.007 * |
| Lumbar lordosis | 19.1 | 1.9 | 29.6 | 2.2 | −10.5 (−16.5 to −4.6) | 0.0008 * |
| Sacral kyphosis | 13.0 | 1.6 | 15.6 | 1.8 | −2.6 (−7.5 to 2.3) | 0.28 |
| Pelvic incidence | 54.5 | 3.6 | 60.4 | 4.1 | −5.9 (−16.9 to 5.1) | 0.29 |
| Posture of each individual spinal segment | ||||||
| T1/2 | 4.6 | 0.5 | 6.1 | 0.6 | −1.5 (−3.3 to 0.3) | 0.09 |
| T2/3 | 4.5 | 0.5 | 5.9 | 0.6 | −1.4 (−3.1 to 0.2) | 0.08 |
| T3/4 | 3.6 | 0.6 | 5.4 | 0.6 | −1.8 (−3.5 to −0.1) | 0.03 * |
| T4/5 | 4.2 | 0.6 | 4.4 | 0.6 | −0.2 (−1.9 to 1.5) | 0.78 |
| T5/6 | 4.9 | 0.5 | 4.5 | 0.6 | 0.4 (−1.1 to 2.0) | 0.55 |
| T6/7 | 3.5 | 0.5 | 5.0 | 0.6 | −1.5 (−3.0 to 0.1) | 0.05 |
| T7/8 | 3.3 | 0.5 | 4.7 | 0.6 | −1.4 (−3.0 to 0.2) | 0.08 |
| T8/9 | 4.2 | 0.5 | 5.8 | 0.6 | −1.6 (−3.2 to 0.01) | 0.05 |
| T9/10 | 3.2 | 0.5 | 3.8 | 0.6 | −0.6 (−2.3 to 1.0) | 0.44 |
| T10/11 | 1.0 | 0.6 | 2.0 | 0.6 | −1.0 (−2.7 to 0.7) | 0.24 |
| T11/12 | 0.5 | 0.7 | 0.2 | 0.8 | 0.3 (−1.8 to 2.4) | 0.79 |
| T12/L1 | 1.8 | 0.5 | 1.6 | 0.6 | 0.2 (−1.4 to 1.9) | 0.79 |
| L1/2 | 3.5 | 0.9 | 4.6 | 1.1 | −1.1 (−4.0 to 1.9) | 0.47 |
| L2/3 | 4.4 | 0.7 | 6.9 | 0.8 | −2.5 (−4.6 to −0.5) | 0.01 * |
| L3/4 | 5.1 | 0.7 | 8.0 | 0.8 | −2.9 (−5.2 to −0.5) | 0.01 * |
| L4/5 | 4.1 | 0.8 | 7.2 | 0.9 | −3.1 (−5.8 to −0.5) | 0.02 * |
| L5/S1 | 2.1 | 0.5 | 3.0 | 0.6 | −0.9 (−2.6 to 0.8) | 0.31 |
| Spinal mobility | ||||||
| Thoracic (°) | ||||||
| Flexion | 26.4 | 2.0 | 18.1 | 2.2 | 8.4 (2.1 to 14.4) | 0.009 * |
| Extension | 14.4 | 3.2 | 16.0 | 3.6 | −1.6 (−11.4 to 8.2) | 0.75 |
| Lateral flexion | 41.1 | 6.9 | 61.4 | 6.9 | −20.4 (−40.6 to −0.1) | 0.37 |
| Lumbar (°) | ||||||
| Flexion | 45.4 | 2.6 | 52.5 | 2.9 | −7.1 (−15.0 to 0.8) | 0.08 |
| Extension | 7.0 | 2.5 | 11.8 | 2.9 | −4.8 (−12.4 to 2.9) | 0.22 |
| Lateral flexion | 16.9 | 2.0 | 22.1 | 2.2 | −5.2 (−11.2 to 0.9) | 0.09 |
| Hip mobility | ||||||
| Hip (°) | ||||||
| Flexion | 44.8 | 3.3 | 49.1 | 3.7 | −4.3 (−14.1 to 5.5) | 0.38 |
| Extension | 4.3 | 2.1 | 7.8 | 2.4 | −3.5 (−10.1 to 2.9) | 0.28 |
| Lumbar-to-hip ratio | 0.5 | 0.02 | 0.5 | 0.03 | −0.01 (−0.08 to 0.08) | 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bayartai, M.-E.; Tringali, G.; Micheli, R.D.; Bondesan, A.; Ventura, E.; Abbruzzese, L.; Sartorio, A. Differences in Spinal Posture and Movement Between Adult Females with Anorexia Nervosa and Age- and Sex-Matched Normal-Weight Controls. J. Clin. Med. 2025, 14, 3723. https://doi.org/10.3390/jcm14113723
Bayartai M-E, Tringali G, Micheli RD, Bondesan A, Ventura E, Abbruzzese L, Sartorio A. Differences in Spinal Posture and Movement Between Adult Females with Anorexia Nervosa and Age- and Sex-Matched Normal-Weight Controls. Journal of Clinical Medicine. 2025; 14(11):3723. https://doi.org/10.3390/jcm14113723
Chicago/Turabian StyleBayartai, Munkh-Erdene, Gabriella Tringali, Roberta De Micheli, Adele Bondesan, Enrica Ventura, Laura Abbruzzese, and Alessandro Sartorio. 2025. "Differences in Spinal Posture and Movement Between Adult Females with Anorexia Nervosa and Age- and Sex-Matched Normal-Weight Controls" Journal of Clinical Medicine 14, no. 11: 3723. https://doi.org/10.3390/jcm14113723
APA StyleBayartai, M.-E., Tringali, G., Micheli, R. D., Bondesan, A., Ventura, E., Abbruzzese, L., & Sartorio, A. (2025). Differences in Spinal Posture and Movement Between Adult Females with Anorexia Nervosa and Age- and Sex-Matched Normal-Weight Controls. Journal of Clinical Medicine, 14(11), 3723. https://doi.org/10.3390/jcm14113723







