Diagnostic Efficiency of Endometrial Sampling Methods and Risk Factors for Endometrial Carcinoma and Precursor Lesions in Premenopausal Women
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACOG | American College of Obstetricians and Gynecologists |
| AUB | abnormal uterine bleeding |
| AUC | area under the curve |
| BMI | body mass index |
| DM | diabetes mellitus |
| D&C | dilatation and curettage |
| EIN | endometrioid intraepithelial neoplasia |
| HT | hypertension |
| IARC | International Agency for Research on Cancer |
| NPV | negative predictive value |
| OR | odds ratio |
| PPV | positive predictive value |
| ROC | receiver operating characteristic |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Seebacher, V.; Schmid, M.; Polterauer, S.; Hefler-Frischmuth, K.; Leipold, H.; Concin, N.; Reinthaller, A.; Hefler, L. The presence of postmenopausal bleeding as prognostic parameter in patients with endometrial cancer: A retrospective multi-center study. BMC Cancer 2009, 9, 460. [Google Scholar] [CrossRef]
- Nees, L.K.; Heublein, S.; Steinmacher, S.; Juhasz-Böss, I.; Brucker, S.; Tempfer, C.B.; Wallwiene, M. Endometrial hyperplasia as a risk factor of endometrial cancer. Arch. Gynecol. Obstet. 2022, 306, 407–421. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, S.G. Problems in the differential diagnosis of endometrial hyperplasia and carcinoma. Mod. Pathol. 2000, 13, 309–327. [Google Scholar] [CrossRef]
- Soslow, R.A. Problems with the current diagnostic approach to complex atypical endometrial hyperplasia. Cancer 2006, 106, 729–731. [Google Scholar] [CrossRef]
- Shutter, J.; Wright, T.C., Jr. Prevalence of underlying adenocarcinoma in women with atypical endometrial hyperplasia. Int. J. Gynecol. Pathol. 2005, 24, 313–318. [Google Scholar] [CrossRef]
- Valenzuela, P.; Sanz, J.M.; Keller, J. Atypical endometrial hyperplasia: Grounds for possible misdiagnosis of endometrial adenocarcinoma. Gynecol. Obstet. Investig. 2003, 56, 163–167. [Google Scholar] [CrossRef]
- Lacey, J.V., Jr.; Sherman, M.E.; Rush, B.B.; Ronnett, B.M.; Ioffe, O.B.; Duggan, M.A.; Glass, A.G.; Richesson, D.A.; Chatterjee, N.; Langholz, B. Absolute risk of endometrial carcinoma during 20-year follow-up among women with endometrial hyperplasia. J. Clin. Oncol. 2010, 28, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Reed, S.D.; Newton, K.M.; Garcia, R.L.; Allison, K.H.; Voigt, L.F.; Jordan, C.D.; Epplein, M.; Swisher, E.; Upson, K.; Ehrlich, K.J.; et al. Complex hyperplasia with and without atypia: Clinical outcomes and implications of progestin therapy. Obstet. Gynecol. 2010, 116 Pt 1, 365–373. [Google Scholar] [CrossRef]
- Bettocchi, S.; Ceci, O.; Vicino, M.; Marello, F.; Impedovo, L.; Selvaggi, L. Diagnostic inadequacy of dilatation and curettage. Fertil. Steril. 2001, 75, 803–805. [Google Scholar] [CrossRef]
- Dueholm, M.; Hjorth, I.M.D.; Dahl, K.; Ørtoft, G. Hysteroscopic resectoscope-directed biopsies and outpatient endometrial sampling for assessment of tumor histology in women with endometrial cancer or atypical hyperplasia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 251, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Bourdel, N.; Chauvet, P.; Tognazza, E.; Pereira, B.; Botchorishvili, R.; Canis, M. Sampling in Atypical Endometrial Hyperplasia: Which Method Results in the Lowest Underestimation of Endometrial Cancer? A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2016, 23, 692–701. [Google Scholar] [CrossRef] [PubMed]
- Ørtoft, G.; Dueholm, M.; Mathiesen, O.; Hansen, E.E.; Lundorf, E.; Møller, C.; Marinovskij, E.; Petersen, L.K. Preoperative staging of endometrial cancer using TVS. MRI. and hysteroscopy. Acta Obstet. Gynecol. Scand. 2013, 92, 536–545. [Google Scholar] [CrossRef]
- Piatek, S.; Warzecha, D.; Kisielewski, F.; Szymusik, I.; Panek, G.; Wielgos, M. Pipelle biopsy and dilatation and curettage in clinical practice: Are factors affecting their effectiveness the same? J. Obstet. Gynaecol. Res. 2019, 45, 645–651. [Google Scholar] [CrossRef]
- Sakna, N.A.; Elgendi, M.; Salama, M.H.; Zeinhom, A.; Labib, S.; Nabhan, A.N. Diagnostic accuracy of endometrial sampling tests for detecting endometrial cancer: A systematic review and meta-analysis. BMJ Open 2023, 13, e072124. [Google Scholar] [CrossRef] [PubMed]
- Quintana-Bertó, R.; Padilla-Iserte, P.; Gil-Moreno, A.; Oliver-Pérez, R.; Coronado, P.J.; Martín-Salamanca, M.B.; Pantoja-Garrido, M.; Lorenzo, C.; Beric, D.; Gilabert-Estellés, J.; et al. Preoperative sampling in endometrial cancer: Evaluation of the histopathological agreement with definitive surgical specimen. Clin. Transl. Oncol. 2022, 24, 2388–2394. [Google Scholar] [CrossRef]
- Utida, G.M.; Kulak, J., Jr. Hysteroscopic and aspiration biopsies in the histologic evaluation of the endometrium. a comparative study. Medicine 2019, 98, e17183. [Google Scholar] [CrossRef]
- Cooper, J.M.; Erickson, M.L. Endometrial sampling techniques in the diagnosis of abnormal uterine bleeding. Obstet. Gynecol. Clin. N. Am. 2000, 27, 235–244. [Google Scholar] [CrossRef]
- Kulaksiz, D.; Erin, R. Direct hysteroscopic endometrial sampling and pipelle sampling in perimenopausal women. Minerva Obstet. Gynecol. 2022, 74, 343–347. [Google Scholar] [CrossRef]
- Piriyev, E.; Mellin, W.; Römer, T. Comparison of aspirating pipettes and hysteroscopy with curettage. Arch. Gynecol. Obstet. 2020, 301, 1485–1492. [Google Scholar] [CrossRef]
- Dijkhuizen, F.P.; Mol, B.W.; Brölmann, H.A.; Heintz, A.P. The accuracy of endometrial sampling in the diagnosis of patients with endometrial carcinoma and hyperplasia: A meta-analysis. Cancer 2000, 89, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.J.; Mann, C.H.; Shah, N.; Khan, K.S.; Song, F.; Gupta, J.K. Accuracy of outpatient endometrial biopsy in the diagnosis of endometrial cancer: A systematic quantitative review. BJOG 2002, 109, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Raglan, O.; Kalliala, I.; Markozannes, G.; Cividini, S.; Gunter, M.J.; Nautiyal, J.; Gabra, H.; Paraskevaidis, E.; Martin-Hirsch, P.; Tsilidis, K.K.; et al. Risk factors for endometrial cancer: An umbrella review of the literature. Int. J. Cancer 2019, 145, 1719–1730. [Google Scholar] [CrossRef]
- Vitale, S.G.; Buzzaccarini, G.; Riemma, G.; Pacheco, L.A.; Sardo, A.D.S.; Carugno, J.; Chiantera, V.; Török, P.; Noventa, M.; Haimovich, S.; et al. Endometrial biopsy: Indications. techniques and recommendations. An evidence-based guideline for clinical practice. J. Gynecol. Obstet. Hum. Reprod. 2023, 52, 102588. [Google Scholar] [CrossRef] [PubMed]
- Will, A.J.; Sanchack, K.E. Endometrial Biopsy; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541135/ (accessed on 19 May 2025).
- Moore, J.F.; Carugno, J. Hysteroscopy; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK564345/ (accessed on 19 May 2025).
- Cooper, D.B.; Menefee, G.W. Dilation and Curettage. 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK568791/ (accessed on 19 May 2025).
- Pennant, M.E.; Mehta, R.; Moody, P.; Hackett, G.; Prentice, A.; Sharp, S.J.; Lakshman, R. Premenopausal abnormal uterine bleeding and risk of endometrial cancer. BJOG 2017, 124, 404–411. [Google Scholar] [CrossRef]
- Husain, S.; Al Hammad, R.S.; Alduhaysh, A.K.; AlBatly, M.M.; Alrikabi, A. Pathological spectrum of endometrial biopsies in Saudi women with abnormal uterine bleeding: A retrospective study of 13-years. Saudi Med. J. 2021, 42, 270–279. [Google Scholar] [CrossRef]
- Sharma, S.; Makaju, R.; Shrestha, S.; Shrestha, A. Histopathological Findings of Endometrial Samples and its Correlation Between the Premenopausal and Postmenopausal Women in Abnormal Uterine Bleeding. Kathmandu Univ. Med. J. 2014, 12, 275–278. [Google Scholar] [CrossRef]
- Committee on Practice Bulletins—Gynecology. Practice bulletin no. 128: Diagnosis of abnormal uterine bleeding in reproductive-aged women. Obstet. Gynecol. 2012, 120, 197–206. [Google Scholar] [CrossRef]
- Lasmar, R.B.; Dias, R.; Barrozo, P.R.M.; Oliveira, M.A.P.; Coutinho, E.S.F.; da Rosa, D.B. Prevalence of hysteroscopic findings and histologic diagnoses in patients with abnormal uterine bleeding. Fertil. Steril. 2008, 89, 1803–1807. [Google Scholar] [CrossRef]
- van Doorn, H.C.; Opmeer, B.C.; Burger, C.W.; Duk, M.J.; Kooi, G.S.; Mol, B.W.J. Inadequate office endometrial sample requires further evaluation in women with postmenopausal bleeding and abnormal ultrasound results. Int. J. Gynaecol. Obstet. 2007, 99, 100–104. [Google Scholar] [CrossRef]
- Dueholm, M.; Forman, A.; Jensen, M.L.; Laursen, H.; Kracht, P. Transvaginal sonography combined with saline contrast sonohysterography in evaluating the uterine cavity in premenopausal patients with abnormal uterine bleeding. Ultrasound Obstet. Gynecol. 2001, 18, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Xie, B.; Qian, C.; Yang, B.; Ning, C.; Yao, X.; Du, Y.; Shi, Y.; Luo, X.; Chen, X. Risk Factors for Unsuccessful Office-Based Endometrial Biopsy: A Comparative Study of Office-Based Endometrial Biopsy (Pipelle) and Diagnostic Dilation and Curettage. J. Minim. Invasive Gynecol. 2018, 25, 724–729. [Google Scholar] [CrossRef]
- Amant, F.; Moerman, P.; Neven, P.; Timmerman, D.; Van Limbergen, E.; Vergote, I. Endometrial cancer. Lancet 2005, 366, 491–505. [Google Scholar] [CrossRef] [PubMed]
- Madan, S.M.; Al-Jufairi, Z.A. Abnormal uterine bleeding. Diagnostic value of hysteroscopy. Saudi Med. J. 2001, 22, 153–156. [Google Scholar]
- Larson, D.M.; Johnson, K.K.; Broste, S.K.; Krawisz, B.R.; Kresl, J.J. Comparison of D&C and office endometrial biopsy in predicting final histopathologic grade in endometrial cancer. Obstet. Gynecol. 1995, 86, 38–42. [Google Scholar] [PubMed]
- Loffer, F.D. The Time Has Come to Quit Relying on a Blind Endometrial Biopsy or Dilation and Curettage to Rule Out Malignant Endometrial Changes. J. Minim. Invasive Gynecol. 2019, 26, 1207–1208. [Google Scholar] [CrossRef]
- Marty, R.; Amouroux, J.; Haouet, S.; De Brux, J. The reliability of endometrial biopsy performed during hysteroscopy. Int. J. Gynaecol. Obstet. 1991, 34, 151–155. [Google Scholar] [CrossRef]
- Sharma, J.; Tiwari, S. Hysteroscopy in Abnormal Uterine Bleeding vs Ultrasonography and Histopathology Report in Perimenopausal and Postmenopausal Women. JNMA J. Nepal. Med. Assoc. 2016, 55, 26–28. [Google Scholar] [CrossRef]
- De Franciscis, P.; Riemma, G.; Schiattarella, A.; Cobellis, L.; Guadagno, M.; Vitale, S.G.; Mosca, L.; Cianci, A.; Colacurci, N. Concordance between the Hysteroscopic Diagnosis of Endometrial Hyperplasia and Histopathological Examination. Diagnostics 2019, 9, 142. [Google Scholar] [CrossRef]
- Lago, V.; Martín, B.; Ballesteros, E.; Cárdenas-Rebollo, J.M.; Minig, L. Tumor Grade Correlation Between Preoperative Biopsy and Final Surgical Specimen in Endometrial Cancer: The Use of Different Diagnostic Methods and Analysis of Associated Factors. Int. J. Gynecol. Cancer 2018, 28, 1258–1263. [Google Scholar] [CrossRef]
- Phelippeau, J.; Canlorbe, G.; Bendifallah, S.; Naoura, I.; Lefevre, M.; Ballester, M.; Daraï, E. Preoperative diagnosis of tumor grade and type in endometrial cancer by pipelle sampling and hysteroscopy: Results of a French study. Surg. Oncol. 2016, 25, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Huang, L.; Huang, K.G.; Yen, C.F.; Han, C.M.; Lee, C.L. Accuracy of hysteroscopic biopsy. compared to dilation and curettage, as a predictor of final pathology in patients with endometrial cancer. Taiwan. J. Obstet. Gynecol. 2015, 54, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Wise, M.R.; Gill, P.; Lensen, S.; Thompson, J.M.D.; Farquhar, C.M. Body mass index trumps age in decision for endometrial biopsy: Cohort study of symptomatic premenopausal women. Am. J. Obstet. Gynecol. 2016, 215, 598.e1–598.e8. [Google Scholar] [CrossRef] [PubMed]
- Drab, A.; Kanadys, W.; Malm, M.; Wdowiak, K.; Dolar-Szczasny, J.; Barczyński, B. Association of endometrial cancer risk with hypertension- an updated meta-analysis of observational studies. Sci. Rep. 2024, 14, 24884. [Google Scholar] [CrossRef] [PubMed]
- Soliman, P.T.; Oh, J.C.; Schmeler, K.M.; Sun, C.C.; Slomovitz, B.M.; Gershenson, D.D.M.; Burke, T.W.; Lu, K.H. Risk factors for young premenopausal women with endometrial cancer. Obstet. Gynecol. 2005, 105, 575–580. [Google Scholar] [CrossRef]
- Farquhar, C.M.; Lethaby, A.; Sowter, M.; Verry, J.; Baranyai, J. An evaluation of risk factors for endometrial hyperplasia in premenopausal women with abnormal menstrual bleeding. Am. J. Obstet. Gynecol. 1999, 181, 525–529. [Google Scholar] [CrossRef]
- Aune, D.; Sen, A.; Vatten, L.J. Hypertension and the risk of endometrial cancer: A systematic review and meta-analysis of case-control and cohort studies. Sci. Rep. 2017, 7, 44808. [Google Scholar] [CrossRef]
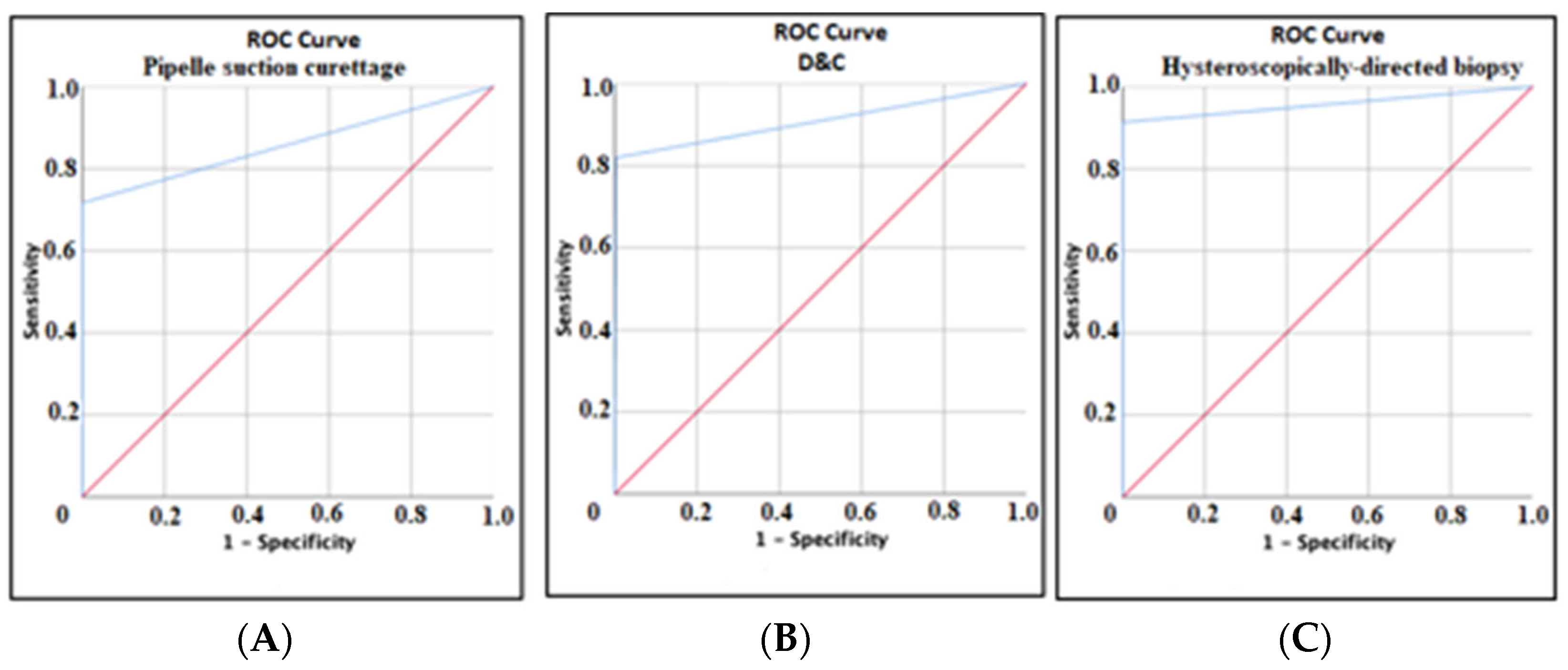
| AUC | %95 CI | Sensitivity | Specificity | PPV | NPV | p | |
|---|---|---|---|---|---|---|---|
| Pipelle suction curettage | 0.858 | 0.789–0.928 | 71.7 | 100.0 | 98.3 | 100.0 | <0.001 |
| D&C | 0.909 | 0.851–0.966 | 82.0 | 99.8 | 98.0 | 97.4 | <0.001 |
| Hysteroscopically- directed biopsy | 0.957 | 0.909–1.000 | 91.3 | 100.0 | 100.0 | 99.3 | <0.001 |
| Endometrial Hyperplasia and Carcinoma (−) (n = 1918) | Endometrial Hyperplasia and Carcinoma (+) (n = 136) | p | |
|---|---|---|---|
| Age (years), mean ± SD | 42.89 ± 6.22 | 43.65 ± 6.19 | 0.739 * |
| BMI (kg/m2), mean ± SD | 28.92 ± 5.70 | 30.98 ± 0.7 | 0.002 ** |
| Gravida, mean ± SD | 2.61 ± 1.66 | 2.29 ± 1.70 | 0.002 ** |
| Parity, mean ± SD | 2.07 ± 1.25 | 1.83 ± 1.13 | 0.007 ** |
| Endometrial thickness (mm) (Min-Max) | 12 (2–45) | 12 (5–38) | 0.234 ** |
| Smoking, n (%) | 0.971 *** | ||
| No | 1563 (81.5) | 111 (81.6) | |
| Yes | 355 (18.5) | 25 (18.4) | |
| Comorbidity, n (%) | 0.021 *** | ||
| None | 1607 (83.8) | 105 (77.2) | |
| HT | 146 (7.6) | 19 (14.0) | |
| DM | 117 (5.6) | 5 (3.7) | |
| HT + DM | 58 (3.0) | 7 (5.1) | |
| Symptom, n (%) | 0.233 *** | ||
| Asymptomatic | 87 (4.5) | 2 (1.5) | |
| Abnormal uterine bleeding | 1781 (92.9) | 130 (95.6) | |
| Pelvic pain | 50 (2.6) | 4 (2.9) | |
| Endometrial fluid, n (%) | 0.168 **** | ||
| No | 1182 (98.1) | 136 (100.0) | |
| Yes | 36 (1.9) | 0 (0.0) |
| Univariate Logistic Regression | B | SE | Exp (B) | %95 GA | p |
|---|---|---|---|---|---|
| BMI | 0.05 | 0.19 | 1.054 | 1.016–1.094 | 0.005 * |
| Gravida | −0.131 | 0.060 | 0.877 | 0.780–0.986 | 0.029 * |
| Parity | −0.174 | 0.079 | 0.840 | 0.720–0.980 | 0.027 * |
| Comorbidity | |||||
| None | 0.025 * | ||||
| HT | 0.689 | 0.264 | 1.992 | 1.187–3.341 | 0.009 * |
| DM | −0.335 | 0.468 | 0.715 | 0.286–1.791 | 0.474 * |
| HT + DM | 0.614 | 0.413 | 1.847 | 0.823–4.147 | 0.137 * |
| Multivariate Logistic Regression | B | SE | Exp (B) | %95 GA | p |
| BMI | 0.052 | 0.020 | 1.053 | 1.012–1.096 | 0.011 * |
| Comorbidity | |||||
| None | 0.085 * | ||||
| HT | 0.829 | 0.344 | 2.291 | 1.168–4.495 | 0.016 * |
| DM | 0.034 | 0.513 | 1.035 | 0.378–2.830 | 0.947 * |
| HT + DM | 0.638 | 0.523 | 1.892 | 0.680-5.269 | 0.212 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Öztürk, F.; Sağnıç, S.; Fırtına Tuncer, S.; Tuncer, H.A. Diagnostic Efficiency of Endometrial Sampling Methods and Risk Factors for Endometrial Carcinoma and Precursor Lesions in Premenopausal Women. J. Clin. Med. 2025, 14, 3658. https://doi.org/10.3390/jcm14113658
Öztürk F, Sağnıç S, Fırtına Tuncer S, Tuncer HA. Diagnostic Efficiency of Endometrial Sampling Methods and Risk Factors for Endometrial Carcinoma and Precursor Lesions in Premenopausal Women. Journal of Clinical Medicine. 2025; 14(11):3658. https://doi.org/10.3390/jcm14113658
Chicago/Turabian StyleÖztürk, Firdevs, Saliha Sağnıç, Serap Fırtına Tuncer, and Hasan Aykut Tuncer. 2025. "Diagnostic Efficiency of Endometrial Sampling Methods and Risk Factors for Endometrial Carcinoma and Precursor Lesions in Premenopausal Women" Journal of Clinical Medicine 14, no. 11: 3658. https://doi.org/10.3390/jcm14113658
APA StyleÖztürk, F., Sağnıç, S., Fırtına Tuncer, S., & Tuncer, H. A. (2025). Diagnostic Efficiency of Endometrial Sampling Methods and Risk Factors for Endometrial Carcinoma and Precursor Lesions in Premenopausal Women. Journal of Clinical Medicine, 14(11), 3658. https://doi.org/10.3390/jcm14113658






