Single-Incision Laparoscopy in Abdominal Trauma: Current Evidence, Clinical Applications, and Evolving Role—A Narrative Review
Abstract
1. Introduction
2. Methods
3. Conventional Laparoscopy in Abdominal Trauma
3.1. Techniques
3.2. Outcomes and Benefits
3.3. Limitations
4. Evolution of Single-Port Laparoscopic Techniques
5. Evidence for SPLS in Abdominal Trauma
5.1. SPLS in Penetrating Abdominal Trauma
5.2. SPLS in Blunt Abdominal Trauma (Small Bowel Injury)
5.3. SPLS in Solid Organ Injuries
5.4. SPLS in Pediatric Abdominal Trauma
6. Technical Considerations and Patient Selection for SPLS in Abdominal Trauma
6.1. Patient Selection
6.2. Important Selection Criteria and Technical Factors for SPLS in Abdominal Trauma
6.2.1. Location of Injury Suspicion
6.2.2. Surgeon Experience and Skills
6.2.3. Equipment and Instrumentation
6.2.4. Adjunct Techniques
6.2.5. Safety and Bailout
6.3. Outcomes and Specific Considerations
7. SPLS Intracorporeal and Extracorporeal Examination and Procedure
7.1. Authors’ Method
7.2. Surgical Setup and Access
7.3. Intracorporeal Exploration Phase
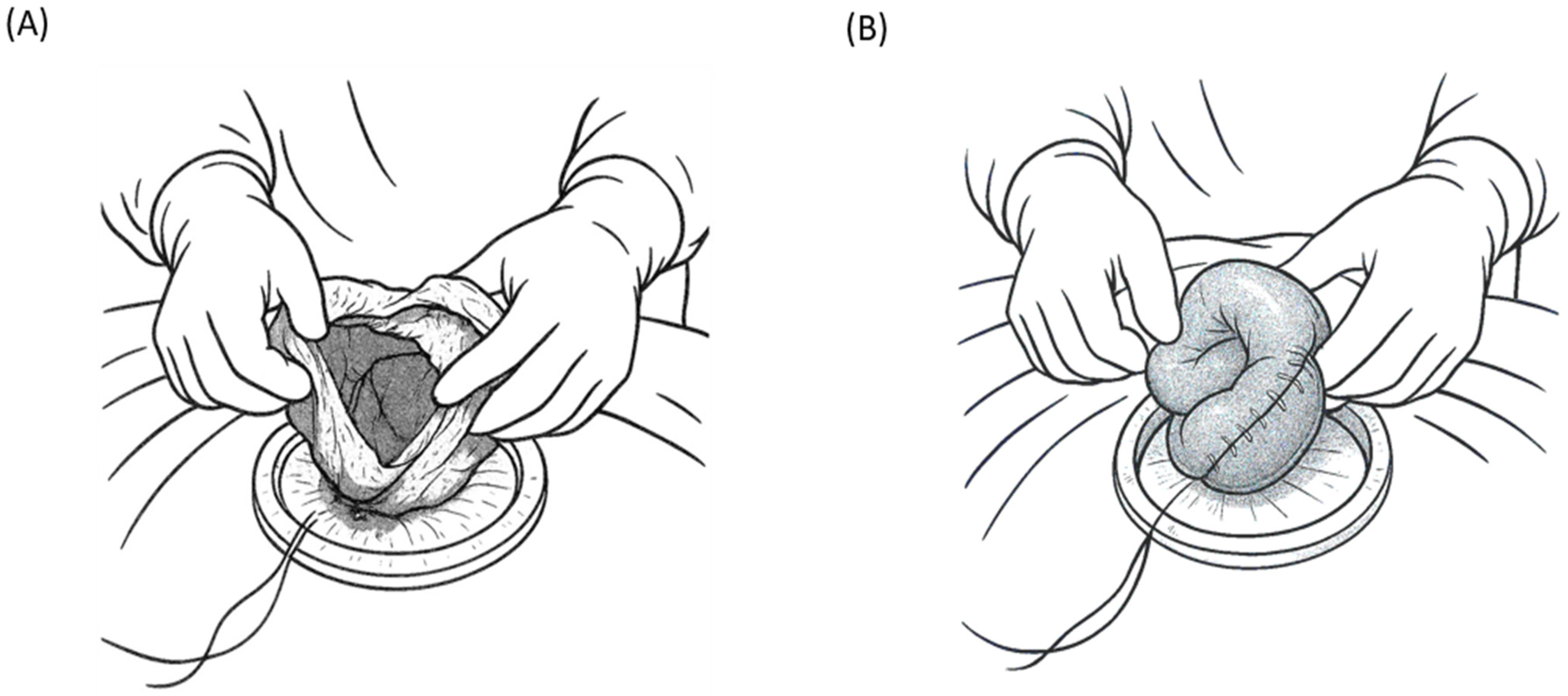
7.4. Extracorporeal Evaluation and Intervention Phase
7.5. Special Considerations
7.6. Advantages of the Hybrid Single-Port Approach
8. Future Directions
8.1. Increasing Adoption and Training
8.2. Clinical Research and Evidence Building
8.3. Technological Advancements
8.4. Protocol Integration and Hybrid Approaches
8.5. Long-Term Outcomes and Quality of Life
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CT | Computed tomography |
| NOTES | Natural orifice transluminal endoscopic surgery |
| SILS | Single-incision laparoscopic surgery |
| SPLS | Single-port laparoscopic surgery |
References
- Gazzaniga, A.B.; Stanton, W.W.; Bartlett, R.H. Laparoscopy in the diagnosis of blunt and penetrating injuries to the abdomen. Am. J. Surg. 1976, 131, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, N.; Baron, N.; Delany, H.M. Peritoneoscopy as an aid in the diagnosis of abdominal trauma: A preliminary report. J. Trauma 1977, 17, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Ki, Y.-J.; Jo, Y.-G.; Park, Y.-C.; Kang, W.-S. The efficacy and safety of laparoscopy for blunt abdominal trauma: A systematic review and meta-analysis. J. Clin. Med. 2021, 10, 1853. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cheng, L.; Liu, J.; Zhang, B.; Wang, W.; Zhu, W.; Guo, Y.; Bao, C.; Hu, Y.; Qi, S.; et al. Laparoscopy vs. laparotomy for the management of abdominal trauma: A systematic review and meta-analysis. Front. Surg. 2022, 9, 817134. [Google Scholar] [CrossRef]
- Sosa, J.L.; Baker, M.; Puente, I.; Sims, D.; Sleeman, D.; Ginzburg, E.; Martin, L. Negative laparotomy in abdominal gunshot wounds: Potential impact of laparoscopy. J. Trauma 1995, 38, 194–197. [Google Scholar] [CrossRef]
- Justin, V.; Fingerhut, A.; Uranues, S. Laparoscopy in blunt abdominal trauma: For whom? When? and why? Curr. Trauma Rep. 2017, 3, 43–50. [Google Scholar] [CrossRef]
- O’Malley, E.; Boyle, E.; O’Callaghan, A.; Coffey, J.C.; Walsh, S.R. Role of laparoscopy in penetrating abdominal trauma: A systematic review. World J. Surg. 2013, 37, 113–122. [Google Scholar] [CrossRef]
- Alzarouni, N.; Salem, A.; Nurelhuda, N.M.; Osman, R.; Eltayyeb, Y. Role of laparoscopy in patients with abdominal trauma: Rashid Hospital Trauma Center experience. J. Emerg. Med. Trauma Acute Care 2022, 2022, 30. [Google Scholar] [CrossRef]
- Kalloo, A.N.; Singh, V.K.; Jagannath, S.B.; Niiyama, H.; Hill, S.L.; Vaughn, C.A.; Magee, C.A.; Kantsevoy, S.V. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest. Endosc. 2004, 60, 114–117. [Google Scholar] [CrossRef]
- Mynster, T.; Wille-Jørgensen, P. Single incision laparoscopic surgery: New ‘toys for boys’? Colorectal Dis. 2011, 13, 351. [Google Scholar] [CrossRef]
- Pelosi, M.A.; Pelosi, M.A., III. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy). J. Reprod. Med. 1992, 37, 588–594. [Google Scholar] [PubMed]
- Navarra, G.; Pozza, E.; Occhionorelli, S.; Carcoforo, P.; Donini, I. One-wound laparoscopic cholecystectomy. Br. J. Surg. 1997, 84, 695. [Google Scholar] [PubMed]
- Chamberlain, R.S.; Sakpal, S.V. A comprehensive review of single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES) techniques for cholecystectomy. J. Gastrointest. Surg. 2009, 13, 1733–1740. [Google Scholar] [CrossRef]
- Lim, K.H.; Chung, B.S.; Kim, J.Y.; Kim, S.S. Laparoscopic surgery in abdominal trauma: A single center review of a 7-year experience. World J. Emerg. Surg. 2015, 10, 16. [Google Scholar] [CrossRef]
- Fabian, T.C.; Croce, M.A.; Stewart, R.M.; Pritchard, F.E.; Minard, G.; Kudsk, K.A. A prospective analysis of diagnostic laparoscopy in trauma. Ann. Surg. 1993, 217, 557–564. [Google Scholar] [CrossRef]
- Townsend, M.C.; Flancbaum, L.; Choban, P.S.; Cloutier, C.T. Diagnostic laparoscopy as an adjunct to selective conservative management of solid organ injuries after blunt abdominal trauma. J. Trauma 1993, 35, 647–651. [Google Scholar] [CrossRef]
- Ivatury, R.R.; Simon, R.J.; Weksler, B.; Bayard, V.; Stahl, W.M. Laparoscopy in the evaluation of the intrathoracic abdomen after penetrating injury. J. Trauma 1992, 33, 101–109. [Google Scholar] [CrossRef]
- Bain, K.; Meytes, V.; Chang, G.C.; Timoney, M.F. Laparoscopy in penetrating abdominal trauma is a safe and effective alternative to laparotomy. Surg. Endosc. 2019, 33, 1618–1625. [Google Scholar] [CrossRef]
- Shamim, A.A.; Zeineddin, S.; Zeineddin, A.; Olufajo, O.A.; Mathelier, G.O.; Cornwell III, E.E.; Fullum, T.; Tran, D. Are we doing too many non-therapeutic laparotomies in trauma? An analysis of the National Trauma Data Bank. Surg. Endosc. 2020, 34, 4072–4078. [Google Scholar] [CrossRef]
- Leppäniemi, A.; Haapiainen, R. Diagnostic laparoscopy in abdominal stab wounds: A prospective, randomized study. J. Trauma 2003, 55, 636–645. [Google Scholar] [CrossRef]
- Cirocchi, R.; Birindelli, A.; Inaba, K.; Mandrioli, M.; Piccinini, A.; Tabola, R.; Carlini, L.; Tugnoli, G.; Di Saverio, S. Laparoscopy for trauma and the changes in its use from 1990 to 2016: A current systematic review and meta-analysis. Surg. Laparosc. Endosc. Percutan. Tech. 2018, 28, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Guth, A.A.; Pachter, H.L. Laparoscopy for penetrating thoracoabdominal trauma: Pitfalls and promises. JSLS J. Soc. Laparoendosc. Surg. 1998, 2, 123–127. [Google Scholar]
- Di Saverio, S.; Birindelli, A.; Podda, M.; Segalini, E.; Piccinini, A.; Coniglio, C.; Frattini, C.; Tugnoli, G. Trauma laparoscopy and the six w’s: Why, where, who, when, what, and how? J. Trauma Acute Care Surg. 2019, 86, 344–367. [Google Scholar] [CrossRef]
- Piskun, G.; Rajpal, S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J. Laparoendosc. Adv. Surg. Tech. A 1999, 9, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, J.R.; Roshek, T.B.; Lynn, D.C.; Earle, D.B. Single-port laparoscopic cholecystectomy: Initial experience. Surg. Endosc. 2010, 24, 1374–1379. [Google Scholar] [CrossRef]
- Zhao, L.; Liao, Z.; Feng, S.; Wu, P.; Chen, G. Single-incision versus conventional laparoscopic appendicectomy in children: A systematic review and meta-analysis. Pediatr. Surg. Int. 2015, 31, 347–353. [Google Scholar] [CrossRef]
- Tsimoyiannis, E.C.; Tsimogiannis, K.E.; Pappas-Gogos, G.; Farantos, C.; Benetatos, N.; Mavridou, P.; Manataki, A. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: A randomized controlled trial. Surg. Endosc. 2010, 24, 1842–1848. [Google Scholar] [CrossRef]
- St Peter, S.D.S.; Adibe, O.O.; Juang, D.; Sharp, S.W.; Garey, C.L.; Laituri, C.A.; Murphy, J.P.; Andrews, W.S.; Sharp, R.J.; Snyder, C.L.; et al. Single incision versus standard 3-port laparoscopic appendectomy: A prospective randomized trial. Ann. Surg. 2011, 254, 586–590. [Google Scholar] [CrossRef]
- Ilhan, M.; Gök, A.F.K.; Bademler, S.; Cücük, Ö.C.; Soytaş, Y.; Yanar, H.T. Comparison of single incision and multi incision diagnostic laparoscopy on evaluation of diaphragmatic status after left thoracoabdominal penetrating stab wounds. J. Minim. Access Surg. 2017, 13, 13–17. [Google Scholar] [CrossRef]
- Chung, J.H.; Kim, K.S.; Choi, H.Y.; Moon, H.S.; Kim, Y.T.; Park, S.Y.; Oh, C.Y.; Lee, K.S.; Kim, T.H.; Lee, S.W. The safety and feasibility of the single-port laparoscopic repair of intraperitoneal bladder rupture. J. Endourol. 2018, 32, 403–409. [Google Scholar] [CrossRef]
- Yang, Y.; Kim, K.S. Extracorporeal repairs of small bowel via mini-laparotomy after a single incision diagnostic laparoscopy in patients with small bowel perforations after blunt trauma: A case report. J. Med. Life Sci. 2019, 16, 13–16. [Google Scholar] [CrossRef]
- Di Saverio, S.; Giorgini, E.; Biscardi, A.; Sibilio, A.; Villani, S.; Naidoo, N.; Catena, F.; Tugnoli, G. Surgical treatment of spleen trauma. Trauma Surg. Thorac. Abdom. Trauma 2014, 2, 117–134. [Google Scholar]
- Wycoff, M.; Hoag, T.P.; Okeke, R.I.; Culhane, J.T. Association of time to definitive hemostasis with mortality in patients with solid organ injuries. Cureus 2023, 15, e45401. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, Y.; Liu, R.; Zhao, L.; Liu, H.; Zhang, J.; Li, G. Systematic review and meta-analysis of single-incision versus conventional laparoscopic appendectomy in children. J. Pediatr. Surg. 2015, 50, 1600–1609. [Google Scholar] [CrossRef]
- Baskovic, M.; Keretic, D.; Lackovic, M.; Krakar, M.B.; Pogorelic, Z. The diagnosis and management of pediatric blunt abdominal trauma-A comprehensive review. Diagnostics 2024, 14, 2257. [Google Scholar] [CrossRef]
- Butler, E.K.; Mills, B.M.; Arbabi, S.; Groner, J.I.; Vavilala, M.S.; Rivara, F.P. Laparoscopy compared with laparotomy for the management of pediatric blunt abdominal trauma. J. Surg. Res. 2020, 251, 303–310. [Google Scholar] [CrossRef]
- Campbell, B.R.; Rooney, A.S.; Krzyzaniak, A.; Lee, J.J.; Carroll, A.N.; Calvo, R.Y.; Peck, K.A.; Martin, M.J.; Bansal, V.; Sise, M.J.; et al. To the point: Utility of laparoscopy for operative management of stabbing abdominal trauma. Am. J. Surg. 2024, 231, 125–131. [Google Scholar] [CrossRef]
- Leppäniemi, A.K.; Elliott, D.C. The role of laparoscopy in blunt abdominal trauma. Ann. Med. 1996, 28, 483–489. [Google Scholar] [CrossRef]
- Chol, Y.B.; Lim, K.S. Therapeutic laparoscopy for abdominal trauma. Surg. Endosc. 2003, 17, 421–427. [Google Scholar] [CrossRef]
- Heeney, A.; O’Connor, D.B.; Martin, S.; Winter, D.C. Single-port access laparoscopic surgery for complex Crohn’s disease. Inflam. Bowel Dis. 2010, 16, 1273–1274. [Google Scholar] [CrossRef]
- Wu, A.S.; Podolsky, E.R.; King, S.A.; Curcillo, P.G.; Paul, G. Single Port Access (SPA™) technique: Video summary. Surg. Endosc. 2010, 24, 1473. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Dong, C.-Z.; Zang, Y.-F.; Xue, Y.; Zhou, X.-G.; Wang, Y.; Ding, Y.-L. Initial experience of single-incision plus one port left-side approach totally laparoscopic distal gastrectomy with uncut Roux-en-Y reconstruction. World J. Gastroenterol. 2020, 26, 4669–4679. [Google Scholar] [CrossRef]
- Solomon, D.; Bell, R.L.; Duffy, A.J.; Roberts, K.E. Single-port cholecystectomy: Small scar, short learning curve. Surg. Endosc. 2010, 24, 2954–2957. [Google Scholar] [CrossRef]
- Murgatroyd, B.; Chakravartty, S.; Sarma, D.R.; Patel, A.G. Two hundred seventy-five single-incision laparoscopic gastric band insertions: What have we learnt? Obes. Surg. 2014, 24, 1073–1077. [Google Scholar] [CrossRef]
- Wormser, C.; Runge, J.J. Advances in laparoscopic surgery. Vet. Clin. North Am. Small Anim. Pract. 2016, 46, 63–84. [Google Scholar] [CrossRef]
- Dapri, G.; Carnevali, P.; Himpens, J.; Bianchi, P.; Opocher, E.; Montorsi, M.; Cadière, G.-B. Single-access transumbilical diagnostic laparoscopy for pancreatic tumor using curved and reusable instruments. Ann. Surg. Oncol. 2011, 18, 628. [Google Scholar] [CrossRef]
- Shussman, N.; Schlager, A.; Elazary, R.; Khalaileh, A.; Keidar, A.; Talamini, M.; Horgan, S.; Rivkind, A.I.; Mintz, Y. Single-incision laparoscopic cholecystectomy: Lessons learned for success. Surg. Endosc. 2011, 25, 404–407. [Google Scholar] [CrossRef]
- Bury, K.; Pawlak, M.; Śmietański, M.; Muysoms, F. Single-incision port-site herniation: Meta-analysis vs. nationwide cohort study. Hernia 2016, 20, 11–12. [Google Scholar] [CrossRef]
- Stabilini, C.; Garcia-Urena, M.A.; Berrevoet, F.; Cuccurullo, D.; Capoccia Giovannini, S.; Dajko, M.; Rossi, L.; Decaestecker, K.; López Cano, M. An evidence map and synthesis review with meta-analysis on the risk of incisional hernia in colorectal surgery with standard closure. Hernia 2022, 26, 411–436. [Google Scholar] [CrossRef]
- Lujan-Mompean, J.A.; Parrilla-Paricio, P.; Robles-Campos, R.; Torralba-Martinez, J.A.; Sanchez-Bueno, F.; Arenas-Ricart, J. Laparoscopic surgery in the management of traumatic hemoperitoneum in stable patients. Surg. Endosc. 1995, 9, 879–881. [Google Scholar] [CrossRef]
- Swain, P.; Fritscher-Ravens, A. Role of video endoscopy in managing small bowel disease. Gut 2004, 53, 1866–1875. [Google Scholar] [CrossRef] [PubMed]
- Watts, G.T. Closed injury of the common bile duct and duodenum. Postgrad. Med. J. 1955, 31, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Koto, M.Z.; Matsevych, O.Y.; Mosai, F.; Patel, S.; Aldous, C.; Balabyeki, M. Laparoscopy for blunt abdominal trauma: A challenging endeavor. Scand. J. Surg. 2019, 108, 273–279. [Google Scholar] [CrossRef]
- Sahai, A.; Ali, A.; Barratt, R.; Belal, M.; Biers, S.; Hamid, R.; Harding, C.; Parkinson, R.; Reid, S.; Thiruchelvam, N.; et al. British Association of Urological Surgeons (BAUS) consensus document: Management of bladder and ureteric injury. BJU Int. 2021, 128, 539–547. [Google Scholar] [CrossRef]
- Rashid, F.; Chakrabarty, M.M.; Singh, R.; Iftikhar, S.Y. A review on delayed presentation of diaphragmatic rupture. World J. Emerg. Surg. 2009, 4, 32. [Google Scholar] [CrossRef]
- Gonzalez, R.P.; Turk, B. Surgical options in colorectal injuries. Scand. J. Surg. 2002, 91, 87–91. [Google Scholar] [CrossRef]
- Nguyen, L.; Ditillo, M.F.; Reina Limon, R.F.A.; Anand, T.; Hosseinpour, H.; Nelson, A.C.; El-Qawaqzeh, K.W.M.; Stewart, C.; Obaid, O.; Joseph, B. Operative management of penetrating colon injury: Gone are the days of the diverting colostomy. J. Am. Coll. Surg. 2022, 235, S49–S50. [Google Scholar] [CrossRef]
- Ortiz, C.; Vela, J.; Contreras, C.; Belmar, F.; Paul, I.; Zinco, A.; Ramos, J.P.; Ottolino, P.; Achurra, P.; Jarufe, N.; et al. A new approach for the acquisition of trauma surgical skills: An OSCE type of simulation training program. Surg. Endosc. 2022, 36, 8441–8450. [Google Scholar] [CrossRef]
- Stroup, S.P.; Bazzi, W.; Derweesh, I.H. Training for laparoendoscopic single-site surgery and natural orifice transluminal endoscopic surgery. BJU Int. 2010, 106, 934–940. [Google Scholar] [CrossRef]
- Sermonesi, G.; Tian, B.W.C.A.; Vallicelli, C.; Abu-Zidan, F.M.; Damaskos, D.; Kelly, M.D.; Leppäniemi, A.; Galante, J.M.; Tan, E.; Kirkpatrick, A.W.; et al. Cesena guidelines: WSES consensus statement on laparoscopic-first approach to general surgery emergencies and abdominal trauma. World J. Emerg. Surg. 2023, 18, 57. [Google Scholar] [CrossRef]
- Celotto, F.; Ramacciotti, N.; Mangano, A.; Danieli, G.; Pinto, F.; Lopez, P.; Ducas, A.; Cassiani, J.; Morelli, L.; Spolverato, G.; et al. Da Vinci single-port robotic system current application and future perspective in general surgery: A scoping review. Surg. Endosc. 2024, 38, 4814–4830. [Google Scholar] [CrossRef] [PubMed]
- Cuschieri, A.; Hennessy, T.P.; Stephens, R.B.; Berci, G. Diagnosis of significant abdominal trauma after road traffic accidents: Preliminary results of a multicentre clinical trial comparing minilaparoscopy with peritoneal lavage. Ann. R. Coll. Surg. Engl. 1988, 70, 153–155. [Google Scholar] [PubMed]
- Kaouk, J.; Aminsharifi, A.; Sawczyn, G.; Kim, S.; Wilson, C.A.; Garisto, J.; Fareed, K. Single-port robotic urological surgery using purpose-built single-port surgical system: Single-institutional experience with the first 100 cases. Urology 2020, 140, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Felli, E.; Brunetti, F.; Disabato, M.; Salloum, C.; Azoulay, D.; de’Angelis, N. Robotic right colectomy for hemorrhagic right colon cancer: A case report and review of the literature of minimally invasive urgent colectomy. World J. Emerg. Surg. 2014, 9, 1–7. [Google Scholar] [CrossRef]
- Robinson, T.D.; Sheehan, J.C.; Patel, P.B.; Marthy, A.G.; Zaman, J.A.; Singh, T.P. Emergent robotic versus laparoscopic surgery for perforated gastrojejunal ulcers: A retrospective cohort study of 44 patients. Surg. Endosc. 2022, 36, 1573–1577. [Google Scholar] [CrossRef]
- de’Angelis, N.; Khan, J.; Marchegiani, F.; Bianchi, G.; Aisoni, F.; Alberti, D.; Ansaloni, L.; Biffl, W.; Chiara, O.; Ceccarelli, G. Robotic surgery in emergency setting: 2021 WSES position paper. World J. Emerg. Surg. 2022, 17, 4. [Google Scholar] [CrossRef]
- Khoo, C.Y.; Liew, T.Y.S.; Mathur, S. Systematic review of the efficacy of a hybrid operating theatre in the management of severe trauma. World J. Emerg. Surg. 2021, 16, 43. [Google Scholar] [CrossRef]
- Smith, B.K.; Sheahan, M.G., III; Sgroi, M.; Weis, T.; Singh, N.; Rigberg, D.; Coleman, D.M.; Lee, J.T.; Shames, M.L.; Mitchell, E.L. Addressing contemporary management of vascular trauma: Optimization of patient care through collaboration. Ann. Surg. 2021, 273, e171–e172. [Google Scholar] [CrossRef]
- Grushka, J.; Ginzburg, E. Through the 10-mm looking glass: Advances in minimally invasive surgery in trauma. Scand. J. Surg. 2014, 103, 143–148. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, S.; Choi, K.-K. Single-Incision Laparoscopy in Abdominal Trauma: Current Evidence, Clinical Applications, and Evolving Role—A Narrative Review. J. Clin. Med. 2025, 14, 3610. https://doi.org/10.3390/jcm14103610
Jeon S, Choi K-K. Single-Incision Laparoscopy in Abdominal Trauma: Current Evidence, Clinical Applications, and Evolving Role—A Narrative Review. Journal of Clinical Medicine. 2025; 14(10):3610. https://doi.org/10.3390/jcm14103610
Chicago/Turabian StyleJeon, Sebeom, and Kang-Kook Choi. 2025. "Single-Incision Laparoscopy in Abdominal Trauma: Current Evidence, Clinical Applications, and Evolving Role—A Narrative Review" Journal of Clinical Medicine 14, no. 10: 3610. https://doi.org/10.3390/jcm14103610
APA StyleJeon, S., & Choi, K.-K. (2025). Single-Incision Laparoscopy in Abdominal Trauma: Current Evidence, Clinical Applications, and Evolving Role—A Narrative Review. Journal of Clinical Medicine, 14(10), 3610. https://doi.org/10.3390/jcm14103610





