Limus Devices for the Treatment of SFA: Latest Outcomes and Future Perspectives
Abstract
1. Introduction
1.1. TAXUS Versus LIMUS, Biochemical Consideration
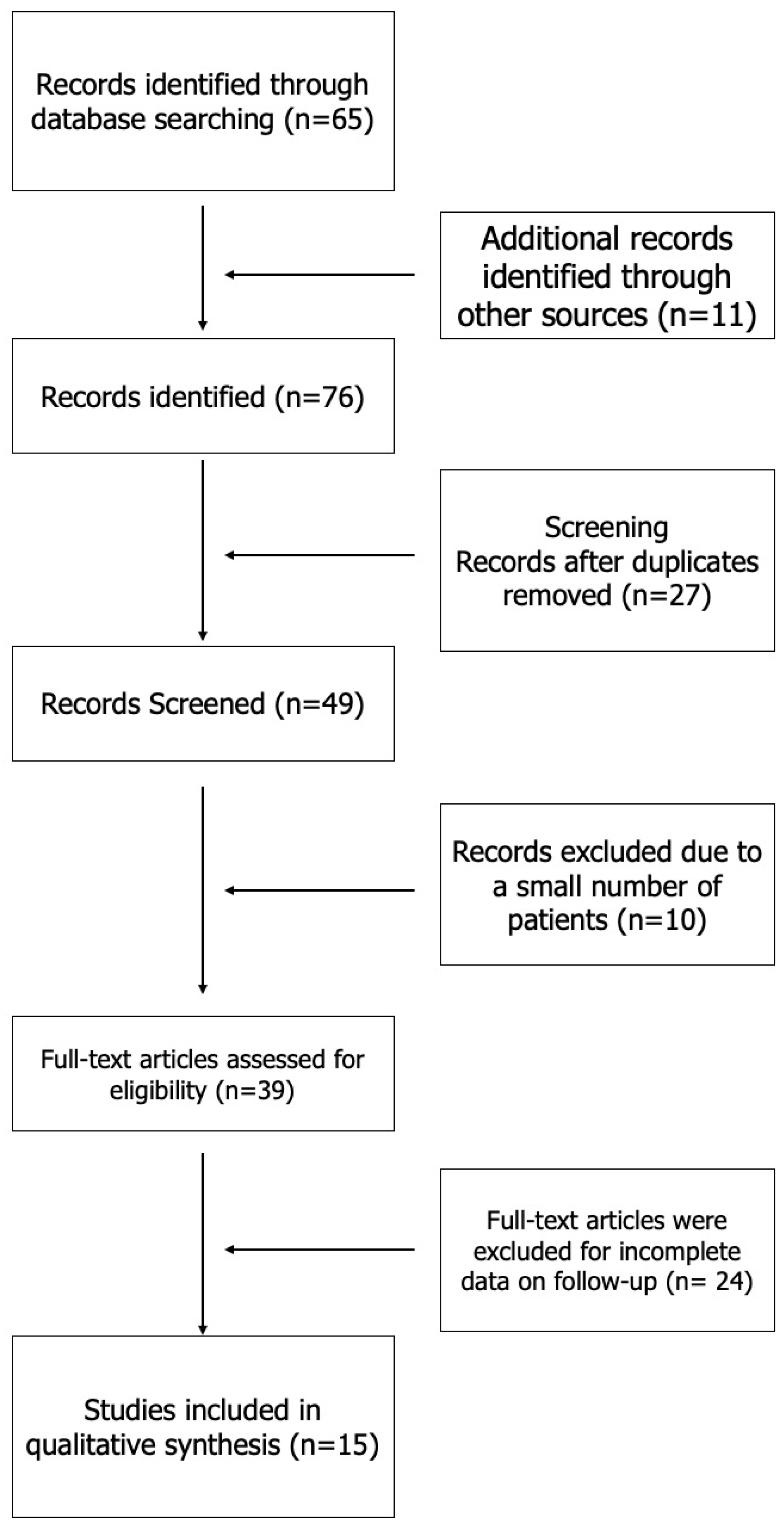
1.2. Review Method
1.3. Sirolimus Devices
1.3.1. STENT—Historical Data
1.3.2. NiTiDES Stent
1.4. Bioresorbable Vascular Scaffold
1.5. Drug-Eluting Ballon
Magic Touch
1.6. SELUTION SLR
1.7. Other Trials
1.7.1. CVT-SFA Trial
1.7.2. PREVISION Trial
2. Discussion
2.1. Drug-Eluting Stent
2.2. Bioresorbable Vascular Scaffold
2.3. Drug-Eluting Balloon
3. Future Directions
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allison, M.A.; Ho, E.; Denenberg, J.O.; Langer, R.D.; Newman, A.B.; Fabsitz, R.R.; Criqui, M.H. Ethnic-Specific Prevalence of Peripheral Arterial Disease in the United States. Am. J. Prev. Med. 2007, 32, 328–333. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics—2022 Update: A Report from the American Heart Association. Circulation 2022, 145, E153–E639. [Google Scholar] [CrossRef] [PubMed]
- Fowkes, F.G.R.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.A.; Williams, L.J.; Mensah, G.A.; et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef]
- Allison, M.A.; Armstrong, D.G.; Goodney, P.P.; Hamburg, N.M.; Kirksey, L.; Lancaster, K.J.; Mena-Hurtado, C.I.; Misra, S.; Treat-Jacobson, D.J.; Solaru, K.T.W.; et al. Health Disparities in Peripheral Artery Disease: A Scientific Statement from the American Heart Association. Circulation 2023, 148, 286–296. [Google Scholar] [CrossRef]
- Song, P.; Fang, Z.; Wang, H.; Cai, Y.; Rahimi, K.; Zhu, Y.; Fowkes, F.G.R.; I Fowkes, F.J.; Rudan, I. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: A systematic review, meta-analysis, and modelling study. Lancet Glob. Health 2020, 8, e721–e729. [Google Scholar] [CrossRef]
- Issa, R.; Nazir, S.; Khan Minhas, A.M.; Lang, J.; Ariss, R.W.; Kayani, W.T.; Khalid, M.U.; Sperling, L.; Shapiro, M.D.; Jneid, H.; et al. Demographic and regional trends of peripheral artery disease-related mortality in the United States, 2000 to 2019. Vasc. Med. 2023, 28, 205–213. [Google Scholar] [CrossRef]
- Aday, A.W.; Matsushita, K. Epidemiology of Peripheral Artery Disease and Polyvascular Disease. Circ. Res. 2021, 128, 1818–1832. [Google Scholar] [CrossRef]
- Mosarla, R.C.; Armstrong, E.; Bitton-Faiwiszewski, Y.; Schneider, P.A.; Secemsky, E.A. State-of-the-Art Endovascular Therapies for the Femoropopliteal Segment: Are We There Yet? J. Soc. Cardiovasc. Angiogr. Interv. 2022, 1, 100439. [Google Scholar] [CrossRef]
- Lupattelli, L.; Barzi, F.; Corneli, P.; Lemmi, A.; Mosca, S. Percutaneous transluminal angioplasty of the vascular area of the lower limbs. Current indications. Radiol Med. 1988, 76, 179–186. Available online: https://pubmed.ncbi.nlm.nih.gov/2971990/ (accessed on 6 October 2024).
- Dotter, C.T.; Judkins, M.P. Percutaneous Transluminal Treatment of Arteriosclerotic Obstruction. Radiology 1965, 84, 631–643. [Google Scholar] [CrossRef]
- Colombo, A.; De Gregorio, J.; Moussa, I.; Kobayashi, Y.; Karvouni, E.; Di Mario, C.; Albiero, R.; Finci, L.; Moses, J. Intravascular ultrasound-guided percutaneous transluminal coronary angioplasty with provisional spot stenting for treatment of long coronary lesions. J. Am. Coll. Cardiol. 2001, 38, 1427–1433. [Google Scholar] [CrossRef] [PubMed]
- Gieskes, L.; Rousseau, H.; Otal, P.; Léger, P.; Soula, P.; Glock, Y.; Joffre, F. Percutaneous treatment of popliteal aneurysms using a covered stent: Preliminary clinical experience. J. Mal. Vasc. 1995, 20, 264–267. Available online: https://pubmed.ncbi.nlm.nih.gov/8586944/ (accessed on 6 October 2024). [PubMed]
- Massaro, G.; Maffi, V.; Russo, D.; Benedetto, D.; Bonanni, M.; Chiricolo, G.; Sangiorgi, G. ‘Leave Nothing Behind’ Strategy in Coronary and Peripheral Artery Disease: An Insight into Sirolimus-Coated Balloons. EMJ Int. Cardiol. 2022, 10, 60–71. [Google Scholar] [CrossRef]
- di Palma, G.; Sanchez-Jimenez, E.F.; Lazar, L.; Cortese, B. Should paclitaxel be considered an old generation DCB? The limus era. Rev. Cardiovasc. Med. 2021, 22, 1323–1330. [Google Scholar] [CrossRef]
- Ferreira, L.T.; Figueiredo, A.C.; Orr, B.; Lopes, D.; Maiato, H. Dissecting the role of the tubulin code in mitosis. In Methods in Cell Biology; Elsevier: Amsterdam, The Netherlands, 2018; Volume 144, pp. 33–74. [Google Scholar] [CrossRef]
- Herdeg, C.; Oberhoff, M.; Baumbach, A.; Blattner, A.; I Axel, D.; Schröder, S.; Heinle, H.; Karsch, K.R. Local paclitaxel delivery for the prevention of restenosis: Biological effects and efficacy in vivo. J. Am. Coll. Cardiol. 2000, 35, 1969–1976. [Google Scholar] [CrossRef]
- Wessely, R.; Blaich, B.; Belaiba, R.S.; Merl, S.; Görlach, A.; Kastrati, A.; Schömig, A. Comparative characterization of cellular and molecular anti-restenotic profiles of paclitaxel and sirolimus. Implications for local drug delivery. Thromb. Haemost. 2007, 97, 1003–1012. [Google Scholar] [CrossRef]
- Chen, Y.; Zeng, Y.; Zhu, X.; Miao, L.; Liang, X.; Duan, J.; Li, H.; Tian, X.; Pang, L.; Wei, Y.; et al. Significant difference between sirolimus and paclitaxel nanoparticles in anti-proliferation effect in normoxia and hypoxia: The basis of better selection of atherosclerosis treatment. Bioact. Mater. 2021, 6, 880–889. [Google Scholar] [CrossRef]
- Laganà, D.; Carrafiello, G.; Dizonno, M.; Barresi, M.; Caronno, R.; Castelli, P.; Fugazzola, C. Trattamento percutaneo delle occlusioni croniche complete dell’arteria femorale superficiale. Radiol. Med. 2008, 113, 567–577. [Google Scholar] [CrossRef]
- Cotroneo, A.R.; Pascali, D.; Santoro, M.; Giancristofaro, D.; Quinto, F.; Iezzi, R. Endovascular treatment of femoropopliteal steno-obstructive disease with percutaneous transluminal angioplasty: Midterm results. Radiol. Med. 2008, 113, 1043–1055. [Google Scholar] [CrossRef]
- Ruffino, M.A.; Fronda, M.; Bergamasco, L.; Natrella, M.; Fanelli, G.; Bellosta, R.; Pegorer, M.; Attisani, L.; Ruggiero, M.; Malfa, P.; et al. Prognostic risk factors for loss of patency after femoropopliteal bailout stenting with dual-component stent: Results from the TIGRIS Italian Multicenter Registry. Radiol. Med. 2021, 126, 1129–1137. [Google Scholar] [CrossRef]
- Laganà, D.; Carrafiello, G.; Lumia, D.; Fontana, F.; Mangini, M.; Vizzari, F.A.; Piffaretti, G.; Fugazzola, C. Recanalisation of thrombotic arterial occlusions with rotational thrombectomy. Radiol. Med. 2011, 116, 932–944. [Google Scholar] [CrossRef]
- Duda, S.H.; Bosiers, M.; Lammer, J.; Scheinert, D.; Zeller, T.; Oliva, V.; Tielbeek, A.; Anderson, J.; Wiesinger, B.; Tepe, G.; et al. Drug-eluting and bare nitinol stents for the treatment of atherosclerotic lesions in the superficial femoral artery: Long-term results from the SIROCCO trial. J. Endovasc. Ther. 2006, 13, 701–710. [Google Scholar] [CrossRef]
- Lammer, J.; Bosiers, M.; Zeller, T.; Schillinger, M.; Boone, E.; Zaugg, M.J.; Verta, P.; Peng, L.; Gao, X.; Schwartz, L.B. First clinical trial of nitinol self-expanding everolimus-eluting stent implantation for peripheral arterial occlusive disease. J. Vasc. Surg. 2011, 54, 394–401. [Google Scholar] [CrossRef]
- Steiner, S.; Honton, B.; Langhoff, R.; Chiesa, R.; Kahlberg, A.; Thieme, M.; Zeller, T.; Garot, P.; Commeau, P.; Cremonesi, A.; et al. 2-Year Results with a Sirolimus-Eluting Self-Expanding Stent for Femoropopliteal Lesions: The First-in-Human ILLUMINA Study. JACC Cardiovasc. Interv. 2022, 15, 618–626. [Google Scholar] [CrossRef]
- Serruys, P.W.; A Ormiston, J.; Onuma, Y.; Regar, E.; Gonzalo, N.; Garcia-Garcia, H.M.; Nieman, K.; Bruining, N.; Dorange, C.; Miquel-Hébert, K.; et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. Lancet 2009, 373, 897–910. [Google Scholar] [CrossRef]
- Serruys, P.W.; Onuma, Y.; Ormiston, J.A.; de Bruyne, B.; Regar, E.; Dudek, D.; Thuesen, L.; Smits, P.C.; Chevalier, B.; McClean, D.; et al. Evaluation of the second generation of a bioresorbable everolimus drug-eluting vascular scaffold for treatment of de novo coronary artery stenosis: Six-month clinical and imaging outcomes. Circulation 2010, 122, 2301–2312. [Google Scholar] [CrossRef]
- Koelemay, M.J.W.; Lijmer, J.G.; Stoker, J.; Legemate, D.A.; Bossuyt, P.M.M. Magnetic resonance angiography for the evaluation of lower extremity arterial disease: A meta-analysis. JAMA 2001, 285, 1338–1345. [Google Scholar] [CrossRef]
- Karamessini, M.T.; Kagadis, G.C.; Petsas, T.; Karnabatidis, D.; Konstantinou, D.; Sakellaropoulos, G.C.; Nikiforidis, G.C.; Siablis, D. CT angiography with three-dimensional techniques for the early diagnosis of intracranial aneurysms. Comparison with intra-arterial DSA and the surgical findings. Eur. J. Radiol. 2004, 49, 212–223. [Google Scholar] [CrossRef]
- Heublein, B.; Rohde, R.; Kaese, V.; Niemeyer, M.; Hartung, W.; Haverich, A. Biocorrosion of magnesium alloys: A new principle in cardiovascular implant technology? Heart 2003, 89, 651–656. [Google Scholar] [CrossRef]
- Onuma, Y.; Serruys, P.W. Bioresorbable scaffold: The advent of a new era in percutaneous coronary and peripheral revascularization? Circulation 2011, 123, 779–797. [Google Scholar] [CrossRef]
- Lammer, J.; Bosiers, M.; Deloose, K.; Schmidt, A.; Zeller, T.; Wolf, F.; Lansink, W.; Sauguet, A.; Vermassen, F.; Lauwers, G.; et al. Bioresorbable Everolimus-Eluting Vascular Scaffold for Patients with Peripheral Artery Disease (ESPRIT I): 2-Year Clinical and Imaging Results. JACC Cardiovasc. Interv. 2016, 9, 1178–1187. [Google Scholar] [CrossRef]
- Choke, E.; Tang, T.Y.; Peh, E.; Damodharan, K.; Cheng, S.C.; Tay, J.S.; Finn, A.V. MagicTouch PTA Sirolimus Coated Balloon for Femoropopliteal and Below the Knee Disease: Results from XTOSI Pilot Study Up To 12 Months. J. Endovasc. Ther. 2021, 29, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Chek Choke, E.T.; Yap, H.Y.; Chong, T.T. Sirolimus Coated Balloon for Femoropopliteal and Below The Knee Disease: Xtosi Trial 24 Month RESULTS. Ann. Vasc. Surg. 2023, 89, 101. [Google Scholar] [CrossRef]
- Barco, S.; Sebastian, T.; Voci, D.; Engelberger, R.P.; Grigorean, A.; Holy, E.; Leeger, C.; Münger, M.; Périard, D.; Probst, E.; et al. Major adverse limb events in patients with femoro-popliteal and below-the-knee peripheral arterial disease treated with either sirolimus-coated balloon or standard uncoated balloon angioplasty: A structured protocol summary of the “SirPAD” randomized controlled trial. Trials 2022, 23, 334. [Google Scholar] [CrossRef]
- Ierardi, A.M.; Franchin, M.; Fontana, F.; Piffaretti, G.; Duka, E.; Tonolini, M.; Miele, V.; Tozzi, M.; Carrafiello, G. Usefulness of paclitaxel-releasing high-pressure balloon associated with cutting balloon angioplasty for treatment of outflow stenoses of failing hemodialysis arteriovenous shunts. Radiol. Med. 2017, 122, 69–76. [Google Scholar] [CrossRef]
- Sirolimus Coated Balloon Versus Standard Balloon for SFA and Popliteal Artery Disease. Available online: https://ctv.veeva.com/study/sirolimus-coated-balloon-versus-standard-balloon-for-sfa-and-popliteal-artery-disease (accessed on 1 October 2024).
- Taneva, G.T.; Pitoulias, G.A.; ABU Bakr, N.; Kazemtash, M.; Castellanos, J.M.; Donas, K.P. Assessment of Sirolimus- vs. paCLitaxEl-coated balloon angioPlasty in atherosclerotic femoropopliteal lesiOnS (ASCLEPIOS Study): Preliminary results. J. Cardiovasc. Surg. 2022, 63, 8–12. [Google Scholar] [CrossRef]
- Teichgräber, U.; Ingwersen, M.; Platzer, S.; Lehmann, T.; Zeller, T.; Aschenbach, R.; Scheinert, D. Head-to-head comparison of sirolimus- versus paclitaxel-coated balloon angioplasty in the femoropopliteal artery: Study protocol for the randomized controlled SIRONA trial. Trials 2021, 22, 665. [Google Scholar] [CrossRef]
- Concept Medical’s MagicTouch Sirolimus-Coated Balloon Granted IDE for SFA Treatment—Endovascular Today. Available online: https://fyra.io (accessed on 9 September 2023).
- Zeller, T.; Brechtel, K.; Meyer, D.-R.; Noory, E.; Beschorner, U.; Albrecht, T. Six-Month Outcomes from the First-in-Human, Single-Arm SELUTION Sustained-Limus-Release Drug-Eluting Balloon Trial in Femoropopliteal Lesions. J. Endovasc. Ther. 2020, 27, 683–690. [Google Scholar] [CrossRef]
- Interim Report of the Success Pta Study Evaluating Safety and Efficacy of the Novel Sirolimus-Eluting Selution Slr Balloon in Peripheral Arterial Disease. Available online: https://secure.onlinecongress.it/Olc/Client/Programme/Public/Abstract/SEM/3618054469399499078201026/EN/Detail?semIdAbstract=198 (accessed on 1 October 2024).
- Jensen, C.J.; Richardt, G.; Tölg, R.; Erglis, A.; Skurk, C.; Jung, W.; Neumann, F.J.; Stangl, K.; Brachmann, J.; Fischer, D.; et al. Angiographic and clinical performance of a paclitaxel-coated balloon compared to a second-generation sirolimus-eluting stent in patients with in-stent restenosis: The BIOLUX randomised controlled trial. EuroIntervention 2018, 14, 1096–1103. [Google Scholar] [CrossRef]
- MedAlliance Commences SELUTION4SFA IDE Trial—Endovascular Today. Available online: https://evtoday.com/news/medalliance-commences-selution4sfa-ide-trial (accessed on 1 October 2024).
- 12-Month PRISTINE Registry Data Show Efficacy of Sirolimus-Eluting Balloon in the Treatment of “Severe” CLTI—Interventional News. Available online: https://interventionalnews.com/firstcirse-session-reveals-12-month-pristine-registry-data-showing-efficacy-of-sirolimus-eluting-balloon-in-the-treatment-of-severe-clti-patients/ (accessed on 1 October 2024).
- Prospective Registry to Investigate the Safety and Efficacy of the Treatment with the Selution Sirolimus Drug Coated Balloon in TASC C and D Atheroma-occlusive Infra-Inguinal Disease in Patients with Chronic Limb Threatening Ischemia from Singapore. Available online: https://ctv.veeva.com/study/prospective-registry-to-investigate-the-safety-and-efficacy-of-the-treatment-with-the-selution-sirol (accessed on 1 October 2024).
- Study Details. CVT-SFA First in Human Trial for Treatment of Superficial Femoral Artery or Proximal Popliteal Artery. Available online: https://clinicaltrials.gov/study/NCT05734157 (accessed on 1 October 2024).
- Study of BD Sirolimus Drug Coated Catheter for Treatment of Femoropopliteal Arteries. Clinical Research Trial Listing. Available online: https://www.centerwatch.com/clinical-trials/listings/NCT05556681/study-of-bd-sirolimus-drug-coated-catheter-for-treatment-of-femoropopliteal-arteries (accessed on 1 October 2024).
- Müller-Hülsbeck, S.; Benko, A.; Soga, Y.; Fujihara, M.; Iida, O.; Babaev, A.; O’connor, D.; Zeller, T.; Dulas, D.D.; Diaz-Cartelle, J.; et al. Two-Year Efficacy and Safety Results from the IMPERIAL Randomized Study of the Eluvia Polymer-Coated Drug-Eluting Stent and the Zilver PTX Polymer-free Drug-Coated Stent. CardioVascular Interv. Radiol. 2021, 44, 368–375. [Google Scholar] [CrossRef]
- Müller-Hülsbeck, S.; Keirse, K.; Zeller, T.; Schroë, H.; Diaz-Cartelle, J. Long-Term Results from the MAJESTIC Trial of the Eluvia Paclitaxel-Eluting Stent for Femoropopliteal Treatment: 3-Year Follow-up. Cardiovasc. Interv. Radiol. 2017, 40, 1832–1838. [Google Scholar] [CrossRef] [PubMed]
- Gouëffic, Y.; Sauguet, A.; Desgranges, P.; Feugier, P.; Rosset, E.; Ducasse, E.; Kaladji, A.; du Mont, L.S.; Pernès, J.M.; Commeau, P.; et al. A Polymer-Free Paclitaxel-Eluting Stent Versus a Bare-Metal Stent for De Novo Femoropopliteal Lesions: The BATTLE Trial. JACC Cardiovasc. Interv. 2020, 13, 447–457. [Google Scholar] [CrossRef]
- Gouëffic, Y.; Torsello, G.; Zeller, T.; Esposito, G.; Vermassen, F.; Hausegger, K.A.; Tepe, G.; Thieme, M.; Gschwandtner, M.; Kahlberg, A.; et al. Efficacy of a Drug-Eluting Stent Versus Bare Metal Stents for Symptomatic Femoropopliteal Peripheral Artery Disease: Primary Results of the EMINENT Randomized Trial. Circulation 2022, 146, 1564–1576. [Google Scholar] [CrossRef] [PubMed]
- Steiner, S.; Schmidt, A.; Zeller, T.; Tepe, G.; Thieme, M.; Maiwald, L.; Schröder, H.; Euringer, W.; Popescu, C.; Brechtel, K.; et al. Low-Dose vs High-Dose Paclitaxel-Coated Balloons for Femoropopliteal Lesions: 2-Year Results from the COMPARE Trial. JACC Cardiovasc. Interv. 2022, 15, 2093–2102. [Google Scholar] [CrossRef]
- Romaguera, R.; Gómez-Hospital, J.A.; Gomez-Lara, J.; Brugaletta, S.; Pinar, E.; Jiménez-Quevedo, P.; Gracida, M.; Roura, G.; Ferreiro, J.L.; Teruel, L.; et al. A Randomized Comparison of Reservoir-Based Polymer-Free Amphilimus-Eluting Stents Versus Everolimus-Eluting Stents with Durable Polymer in Patients with Diabetes Mellitus: The RESERVOIR Clinical Trial. JACC Cardiovasc. Interv. 2016, 9, 42–50. [Google Scholar] [CrossRef]
- A Byrne, R.; Eeckhout, E.; Sardella, G.; Stella, P.; Verheye, S.; Center, Z.M.A.C. PCI in Patients with Diabetes: Role of the Cre8 Drug-eluting Stent. Interv. Cardiol. Rev. 2017, 12, 13–17. [Google Scholar] [CrossRef]
- Bontinck, J.; Goverde, P.; Schroë, H.; Hendriks, J.; Maene, L.; Vermassen, F. Treatment of the femoropopliteal artery with the bioresorbable REMEDY stent. J. Vasc. Surg. 2016, 64, 1311–1319. [Google Scholar] [CrossRef]
- Bradbury, A.W.; Adam, D.J.; Bell, J.; Forbes, J.F.; Fowkes, F.G.R.; Gillespie, I.; Ruckley, C.V.; Raab, G.M. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: Analysis of amputation free and overall survival by treatment received. J. Vasc. Surg. 2010, 51, 18S–31S. [Google Scholar] [CrossRef]
- Werner, M.; Micari, A.; Cioppa, A.; Vadalà, G.; Schmidt, A.; Sievert, H.; Rubino, P.; Angelini, A.; Scheinert, D.; Biamino, G. Evaluation of the biodegradable peripheral Igaki-Tamai stent in the treatment of de novo lesions in the superficial femoral artery: The GAIA study. JACC Cardiovasc. Interv. 2014, 7, 305–312. [Google Scholar] [CrossRef]
- El Khoury, R.; Tzvetanov, I.; Estrada, E.A.; McCarroll, E.; Michal, E.; Blumeyer, J.; Guy, L.-G.; Laflamme, M.; Schwartz, L.B. Intravascular treatment of long segments of experimental peripheral arteries with multiple, serial, balloon-expandable, resorbable scaffolds. JVS Vasc. Sci. 2022, 3, 205–210. [Google Scholar] [CrossRef]
- The Efemoral Vascular Scaffold System (EVSS) for the Treatment of Patients with Symptomatic Peripheral Vascular Disease from Stenosis or Occlusion of the Femoropopliteal Artery. Available online: https://ctv.veeva.com/study/the-efemoral-vascular-scaffold-system-evss-for-the-treatment-of-patients-with-symptomatic-peripher (accessed on 1 October 2024).
- Sachar, R.; Soga, Y.; Ansari, M.M.; Kozuki, A.; Lopez, L.; Brodmann, M.; Schroë, H.; Ramanath, V.S.; Diaz-Cartelle, J.; Zeller, T. 1-Year Results from the RANGER II SFA Randomized Trial of the Ranger Drug-Coated Balloon. JACC Cardiovasc. Interv. 2021, 14, 1123–1133. [Google Scholar] [CrossRef]
- Rosenfield, K.; Jaff, M.R.; White, C.J.; Rocha-Singh, K.; Mena-Hurtado, C.; Metzger, D.C.; Brodmann, M.; Pilger, E.; Zeller, T.; Krishnan, P.; et al. Trial of a Paclitaxel-Coated Balloon for Femoropopliteal Artery Disease. N. Engl. J. Med. 2015, 373, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Micari, A.; Brodmann, M.; Keirse, K.; Peeters, P.; Tepe, G.; Frost, M.; Wang, H.; Zeller, T.; Torsello, G.; Scheinert, D.; et al. Drug-Coated Balloon Treatment of Femoropopliteal Lesions for Patients with Intermittent Claudication and Ischemic Rest Pain: 2-Year Results from the IN.PACT Global Study. JACC Cardiovasc. Interv. 2018, 11, 945–953. [Google Scholar] [CrossRef]
- VIVANews—Results from 20 Highly Anticipated Vascular Interventional Clinical Trials to Be Presented for the First Time at VIVA19. Available online: https://viva-foundation.org/news-article?id=790 (accessed on 6 October 2024).
- Iida, O.; Soga, Y.; Saito, S.; Mano, T.; Hayakawa, N.; Ichihashi, S.; Kawasaki, D.; Suzuki, K.; Yamaoka, T.; Fujihara, M.; et al. A Novel Sirolimus-Coated Balloon for the Treatment of Femoropopliteal Lesions: The SELUTION SFA Japan Trial. JACC Cardiovasc. Interv. 2024, 17, 1547–1556. [Google Scholar] [CrossRef]
- Marlevi, D.; Edelman, E.R. Vascular Lesion–Specific Drug Delivery Systems: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 2413–2431. [Google Scholar] [CrossRef]
| No. of Patients | Primary Patency (24 mos) | TLR (24 mos) | |
|---|---|---|---|
| NiTiDES (ILLUMINA Trial) [53] | 100 | 83.4% | 6.9% |
| Eluvia (IMPERIAL Trial) [49] | 309/465 | 83.5% | 7.2% |
| Zilver PTX (IMPERIAL Trial) [49] | 156/465 | 77.1% | 20.1% |
| Eluvia (MAJESTIC Trial) [50] | 57 | 83.5% | 7.2% |
| Zilver PTX (BATTLE Trial) [51] | 90/181 | 78.8% | 12.4% |
| BMS (BATTLE Trial) [51] | 91 | 74.6% | 14.4% |
| Eluvia (EMINENT Trial) [52] | 508/775 | 83% (12 mos) | 11.85% (12 mos) |
| BMS (EMINENT Trial) [52] | 267/775 | 76.3% (12 mos) | 11.8% (12 mos) |
| No. of Patients | Primary Patency | TLR | |||
|---|---|---|---|---|---|
| 12 (mos) | 24 (mos) | 12 (mos) | 24 (mos) | ||
| ESPRIT—I BVS [32] | 35 | 87.9% | 83.9% | 8.8% | 11.8% |
| REDEMY [56] | 99 | 58% | / | 33% | / |
| BASIL vs. CFE—BASI [57] | 40/80 | 80% | / | 12.4% | / |
| BASIL vs. CFE—Sugery [57] | 40/80 | 100% | / | 14.4% | / |
| GAIA [58] study | 30 | 32.1% (12 mos) | / | 57.1% (12 mos) | / |
| Primary Patency | TLR | |||||||
|---|---|---|---|---|---|---|---|---|
| No. of Patient | Lesion Length | 6 mos | 12 mos | 24 mos | 6 mos | 12 mos | 24 mos | |
| XTOSI [33,44] | 20/50 | 227 ± 108 mm | 88.2% | 78.6% | 53% | 5.6% | 5.9% | 11% (overall) |
| SELUTION SFA FIM [64] | 50 | 64.3 ± 42.8 mm | 88.4% | 75.7% | 81.6% | 2.3% | 4.3% | 4.3% |
| COMPARE/IN.PACT [53] | 207/414 | 128.3 ± 97.3 mm | / | 81.5% | 66.7% | 2.1% | 7.4% | 13% |
| COMPARE/RANGER [53] | 207/414 | 123.9 ± 97.8 mm | / | 83% | 65.5% | 2.5% | 9.5% | 17.3% |
| RANGER SFA [61] | 71/105 | 68 ± 46 mm | 87% | 86.4% | / | 5.6% | 8.8% | / |
| LEVANT 2 [62] | 316/476 | 107.9 ± 47.8 mm | 90% | 65.2% | / | / | 12.1% | / |
| IN.PACT SFA [63] | 220/331 | 89.4 ± 48.9 mm | / | 82.2% | 78.9% | / | 2.4% | 9.1% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xhepa, G.; Inzerillo, A.; Constantinescu, I.; Faerber, P.; Gleyzolle, A.; Biondetti, P.; Del Grande, F.; Xhepa, E.; Mortellaro, S.; Carrafiello, G.; et al. Limus Devices for the Treatment of SFA: Latest Outcomes and Future Perspectives. J. Clin. Med. 2025, 14, 3594. https://doi.org/10.3390/jcm14103594
Xhepa G, Inzerillo A, Constantinescu I, Faerber P, Gleyzolle A, Biondetti P, Del Grande F, Xhepa E, Mortellaro S, Carrafiello G, et al. Limus Devices for the Treatment of SFA: Latest Outcomes and Future Perspectives. Journal of Clinical Medicine. 2025; 14(10):3594. https://doi.org/10.3390/jcm14103594
Chicago/Turabian StyleXhepa, Genti, Agostino Inzerillo, Ilinca Constantinescu, Pierre Faerber, Adrien Gleyzolle, Pierpaolo Biondetti, Filippo Del Grande, Edon Xhepa, Simone Mortellaro, Gianpaolo Carrafiello, and et al. 2025. "Limus Devices for the Treatment of SFA: Latest Outcomes and Future Perspectives" Journal of Clinical Medicine 14, no. 10: 3594. https://doi.org/10.3390/jcm14103594
APA StyleXhepa, G., Inzerillo, A., Constantinescu, I., Faerber, P., Gleyzolle, A., Biondetti, P., Del Grande, F., Xhepa, E., Mortellaro, S., Carrafiello, G., Pellegrino, G., & Ricoeur, A. (2025). Limus Devices for the Treatment of SFA: Latest Outcomes and Future Perspectives. Journal of Clinical Medicine, 14(10), 3594. https://doi.org/10.3390/jcm14103594







