Socioeconomic Disadvantage, Residential Remoteness and Access to Specialised Interventions in Cerebral Palsy: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
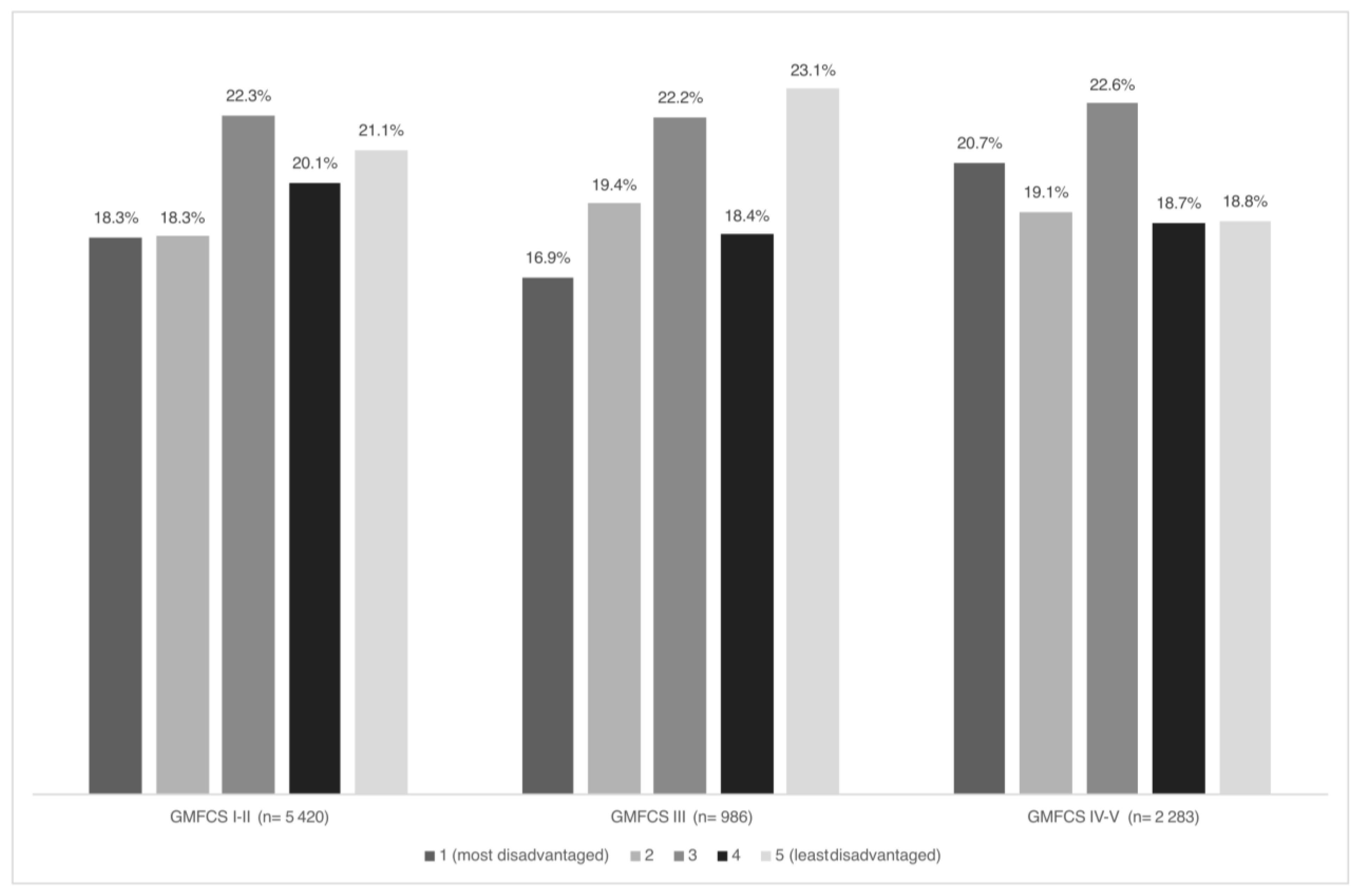
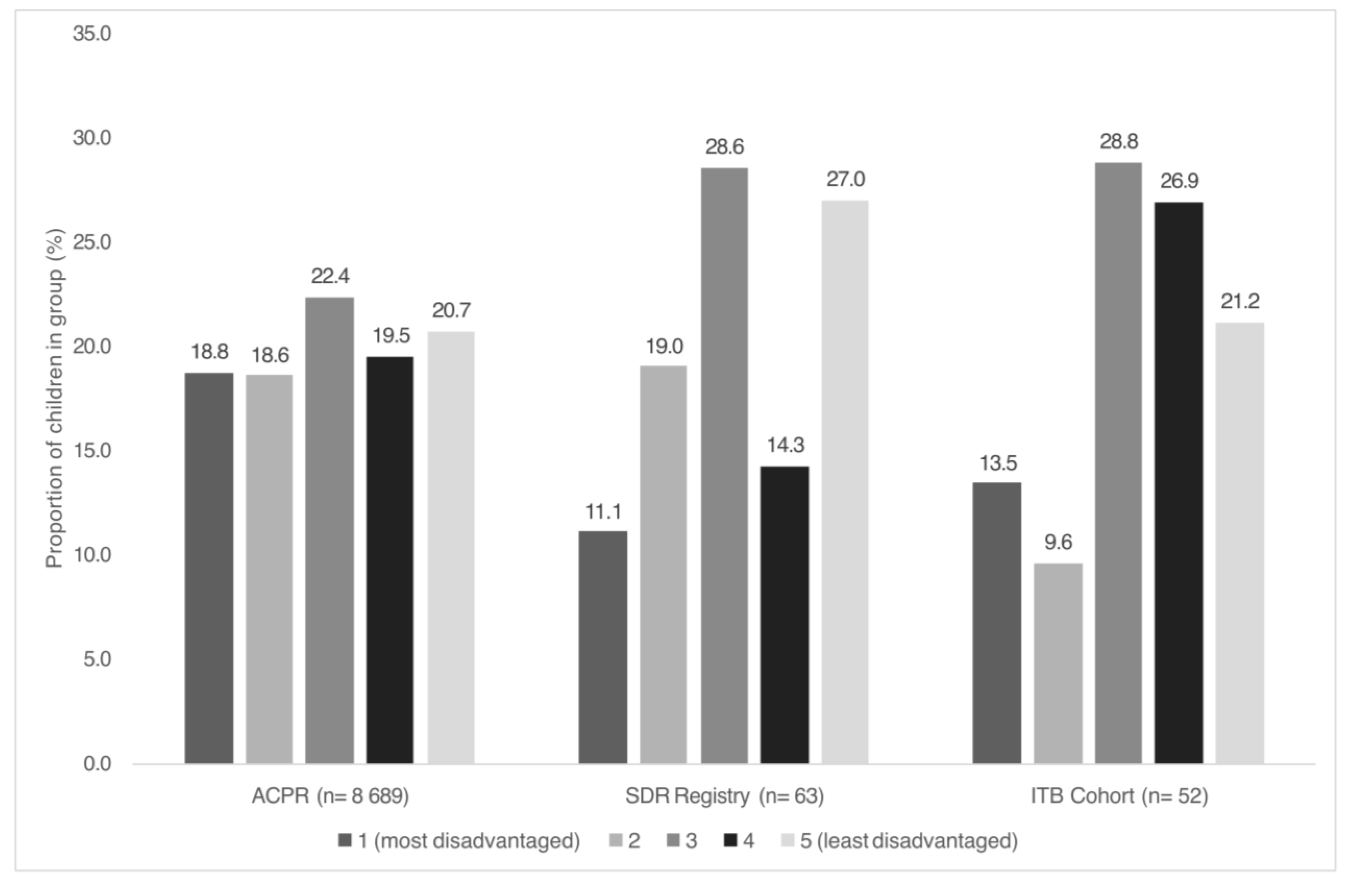
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Galea, C.; Mcintyre, S.; Smithers-Sheedy, H.; Reid, S.M.; Gibson, C.; Delacy, M.; Watson, L.; Goldsmith, S.; Badawi, N.; Blair, E.; et al. Cerebral palsy trends in Australia (1995–2009): A population-based observational study. Dev. Med. Child. Neurol. 2019, 61, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Graham, D.; Paget, S.P.; Wimalasundera, N. Current thinking in the health care management of children with cerebral palsy. Med. J. Aust. 2019, 210, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Solaski, M.; Majnemer, A.; Oskoui, M. Contribution of socio-economic status on the prevalence of cerebral palsy: A systematic search and review. Dev. Med. Child. Neurol. 2014, 56, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Woolfenden, S.; Galea, C.; Smithers-Sheedy, H.; Blair, E.; Mcintyre, S.; Reid, S.; Delacy, M.; Badawi, N.; On Behalf of the Australian Cerebral Palsy Register Group; Quest, C. Impact of social disadvantage on cerebral palsy severity. Dev. Med. Child. Neurol. 2019, 61, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Oskoui, M.; Messerlian, C.; Blair, A.; Gamache, P.; Shevell, M. Variation in cerebral palsy profile by socio-economic status. Dev. Med. Child. Neurol. 2016, 58, 160–166. [Google Scholar] [CrossRef]
- Woolfenden, S.; Galea, C.; Badland, H.; Sheedy, H.S.; Williams, K.; Kavanagh, A.M.; Reddihough, D.; Goldfeld, S.; Lingam, R.; Badawi, N.; et al. Use of health services by preschool-aged children who are developmentally vulnerable and socioeconomically disadvantaged: Testing the inverse care law. J. Epidemiol. Community Health 2020, 74, 495–501. [Google Scholar] [CrossRef]
- Paget, S.P.; McIntyre, S.; Goldsmith, S.; Ostojic, K.; Shrapnel, J.; Schneuer, F.; Waugh, M.C.; Kyriagis, M.; Nassar, N. Non-attendance at outpatient clinic appointments by children with cerebral palsy. Dev. Med. Child. Neurol. 2022, 64, 1106–1113. [Google Scholar] [CrossRef]
- Himmelmann, K.; Påhlman, M.; Andersen, G.L.; Vik, T.; Virella, D.; Horridge, K.; Neubauer, D.; Arnaud, C.; Rackauskaite, G.; de la Cruz, J. Access to Intrathecal Baclofen Treatment for Children with Cerebral Palsy in European Countries: An SCPE Survey Reveals Important Differences. Neuropediatrics 2020, 51, 129–134. [Google Scholar] [CrossRef]
- Grunt, S.; Fieggen, A.G.; Vermeulen, R.J.; Becher, J.G.; Langerak, N.G. Selection criteria for selective dorsal rhizotomy in children with spastic cerebral palsy: A systematic review of the literature. Dev. Med. Child. Neurol. 2014, 56, 302–312. [Google Scholar] [CrossRef]
- Saulino, M.; Ivanhoe, C.B.; McGuire, J.R.; Ridley, B.; Shilt, J.S.; Boster, A.L. Best Practices for Intrathecal Baclofen Therapy: Patient Selection. Neuromodulation 2016, 19, 607–615. [Google Scholar] [CrossRef]
- Australian Cerebral Palsy Register Group. Report of the Australian Cerebral Palsy Register, Birth Years 1995–2016. 2023. Available online: https://cerebralpalsy.org.au/wp-content/uploads/2023/06/2023-ACPR-Report.pdf (accessed on 22 August 2024).
- DeLacy, M.J.; Louca, C.; Smithers-Sheedy, H.; McIntyre, S.; Australian Cerebral Palsy Register, G. Change in residential remoteness during the first 5 years of life in an Australian cerebral palsy cohort. Dev. Med. Child. Neurol. 2016, 58 (Suppl. S2), 60–65. [Google Scholar] [CrossRef]
- Arefadib, N.; Moore, T.G. Reporting the Health and Development of Children in Rural and Remote Australia. 2017. Available online: https://ccch.org.au/resource-hub/reports/reporting-the-health-and-development-of-children-in-rural-and-remote-australia/ (accessed on 21 August 2024).
- Australian Institute of Health and Welfare. Health System Overview 2024. Available online: https://www.aihw.gov.au/reports/australias-health/health-system-overview (accessed on 8 July 2024).
- Australian Government Department of Health and Aged Care. The Australian Health System 2019. Available online: https://www.health.gov.au/about-us/the-australian-health-system (accessed on 8 July 2024).
- Lewis, J.; Bear, N.; Baker, F.; Fowler, A.; Lee, O.; McLennan, K.; Richardson, E.; Scheinberg, A.; Smith, N.; Thomason, P.; et al. Australian children undergoing selective dorsal rhizotomy: Protocol for a national registry of multidimensional outcomes. BMJ Open. 2019, 9, e025093. [Google Scholar] [CrossRef] [PubMed]
- Stewart, K.; Hutana, G.; Kentish, M. Intrathecal baclofen therapy in paediatrics: A study protocol for an Australian multicentre, 10-year prospective audit. BMJ Open. 2017, 7, e015863. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child. Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rosblad, B.; Beckung, E.; Arner, M.; Ohrvall, A.M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child. Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Hidecker, M.J.; Paneth, N.; Rosenbaum, P.L.; Kent, R.D.; Lillie, J.; Eulenberg, J.B.; Chester, K.; Johnson, B., Jr.; Michalsen, L.; Evatt, M.; et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev. Med. Child. Neurol. 2011, 53, 704–710. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA), Australia. ABS Website. 2023. Available online: https://www.abs.gov.au/statistics/people/people-and-communities/socio-economic-indexes-areas-seifa-australia/latest-release#cite-window1 (accessed on 22 August 2024).
- Australian Bureau of Statistics. Australian Statistical Geography Standard. 2023. Available online: https://www.abs.gov.au/statistics/statistical-geography/australian-statistical-geography-standard-asgs (accessed on 21 August 2024).
- Lumsden, D.E.; Kaminska, M.; Tomlin, S.; Lin, J.P. Medication use in childhood dystonia. Eur. J. Paediatr. Neurol. 2016, 20, 625–629. [Google Scholar] [CrossRef]
- Nicholson, J.M.; Lucas, N.; Berthelsen, D.; Wake, M. Socioeconomic inequality profiles in physical and developmental health from 0-7 years: Australian National Study. J. Epidemiol. Community Health 2012, 66, 81–87. [Google Scholar] [CrossRef]
- Oosterhoff, M.; Joore, M.A.; Bartelink, N.H.M.; Winkens, B.; Schayck, O.C.P.; Bosma, H. Longitudinal analysis of health disparities in childhood. Arch. Dis. Child. 2019, 104, 781–788. [Google Scholar] [CrossRef]
- Rougeaux, E.; Hope, S.; Law, C.; Pearce, A. Have health inequalities changed during childhood in the New Labour generation? Findings from the UK Millennium Cohort Study. BMJ Open 2017, 7, e012868. [Google Scholar] [CrossRef]
- Hart, J.T. The inverse care law. Lancet 1971, 1, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Paget, S.P.; McIntyre, S.; Schneuer, F.J.; Martin, T.; Sellars, L.; Burnett, H.; Price, S.; Nassar, N. Outpatient encounters, continuity of care, and unplanned hospital care for children and young people with cerebral palsy. Dev. Med. Child. Neurol. 2024, 66, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Henry, G.; Webb, A.; Galea, C.; Pearce, A.; Balde, I.; Garrity, F.; Marmont, S.; Espie, J.; Badawi, N.; McIntyre, S. Out-of-pocket costs for families and people living with cerebral palsy in Australia. PLoS ONE 2023, 18, e0288865. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, C.; Hurst, S. Implicit bias in healthcare professionals: A systematic review. BMC Med. Ethics. 2017, 18, 19. [Google Scholar] [CrossRef]
- A Lewis, J.; Paget, S.P.; Wimalasundera, N.; Wynter, M.; Campbell, L.; Lee, O.S.; Stewart, K.; Shah, R.; McKay, M.J.; The Selective Dorsal Rhizotomy Knowledge Translation Advisory Team. Informing knowledge translation for selective dorsal rhizotomy: A survey of Australian clinicians and people with lived experience of cerebral palsy. J. Paediatr. Child. Health 2024, 60, 443–448. [Google Scholar] [CrossRef]
- Barnacoat, J.M.; Lewis, J.; Stewart, K.; Mohammad, S.S.; Paget, S. Content and readability of patient educational materials about neuromodulation for childhood movement disorders. Disabil. Rehabil. 2024, 47, 2572–2578. [Google Scholar] [CrossRef]

| SDR | ITB | |
|---|---|---|
| Total (n) | 64 | 52 |
| Sex n (%) | ||
| Male | 44 (68.8) | 27 (51.9) |
| Female | 20 (31.3) | 25 (48.1) |
| GMFCS n (%) | ||
| I | ||
| II | 21 (33.3) | |
| III | 35 (55.6) | 1 (1.9) |
| IV | 7 (11.1) | 18 (34.6) |
| V | 33 (63.5) | |
| MACS n (%) | ||
| I | 35 (56.5) | |
| II | 23 (37.1) | 2 (3.8) |
| III | 4 (6.5) | 8 (15.4) |
| IV | 12 (23.1) | |
| V | 30 (57.7) | |
| CFCS n (%) | ||
| I | 52 (86.7) | 3 (5.9) |
| II | 4 (6.7) | 5 (9.8) |
| III | 4 (6.7) | 9 (17.6) |
| IV | 10 (19.6) | |
| V | 24 (47.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paget, S.P.; Stewart, K.; Copeland, L.; Waight, E.; Smith, N.; Baker, F.; Lewis, J.; on behalf of the Australian Selective Dorsal Rhizotomy Research Group and Australian Paediatric Intrathecal Baclo-fen Research Group. Socioeconomic Disadvantage, Residential Remoteness and Access to Specialised Interventions in Cerebral Palsy: A Cross-Sectional Study. J. Clin. Med. 2025, 14, 3579. https://doi.org/10.3390/jcm14103579
Paget SP, Stewart K, Copeland L, Waight E, Smith N, Baker F, Lewis J, on behalf of the Australian Selective Dorsal Rhizotomy Research Group and Australian Paediatric Intrathecal Baclo-fen Research Group. Socioeconomic Disadvantage, Residential Remoteness and Access to Specialised Interventions in Cerebral Palsy: A Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(10):3579. https://doi.org/10.3390/jcm14103579
Chicago/Turabian StylePaget, Simon P., Kirsty Stewart, Lisa Copeland, Emma Waight, Nadine Smith, Felicity Baker, Jennifer Lewis, and on behalf of the Australian Selective Dorsal Rhizotomy Research Group and Australian Paediatric Intrathecal Baclo-fen Research Group. 2025. "Socioeconomic Disadvantage, Residential Remoteness and Access to Specialised Interventions in Cerebral Palsy: A Cross-Sectional Study" Journal of Clinical Medicine 14, no. 10: 3579. https://doi.org/10.3390/jcm14103579
APA StylePaget, S. P., Stewart, K., Copeland, L., Waight, E., Smith, N., Baker, F., Lewis, J., & on behalf of the Australian Selective Dorsal Rhizotomy Research Group and Australian Paediatric Intrathecal Baclo-fen Research Group. (2025). Socioeconomic Disadvantage, Residential Remoteness and Access to Specialised Interventions in Cerebral Palsy: A Cross-Sectional Study. Journal of Clinical Medicine, 14(10), 3579. https://doi.org/10.3390/jcm14103579







