The Effect of Eight Weeks of Passive Heat Therapy on Mental Health, Sleep, and Chronic Pain in Persons with Spinal Cord Injury: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design and Procedures
2.3. Outcomes
2.4. Statistical Analysis
3. Results
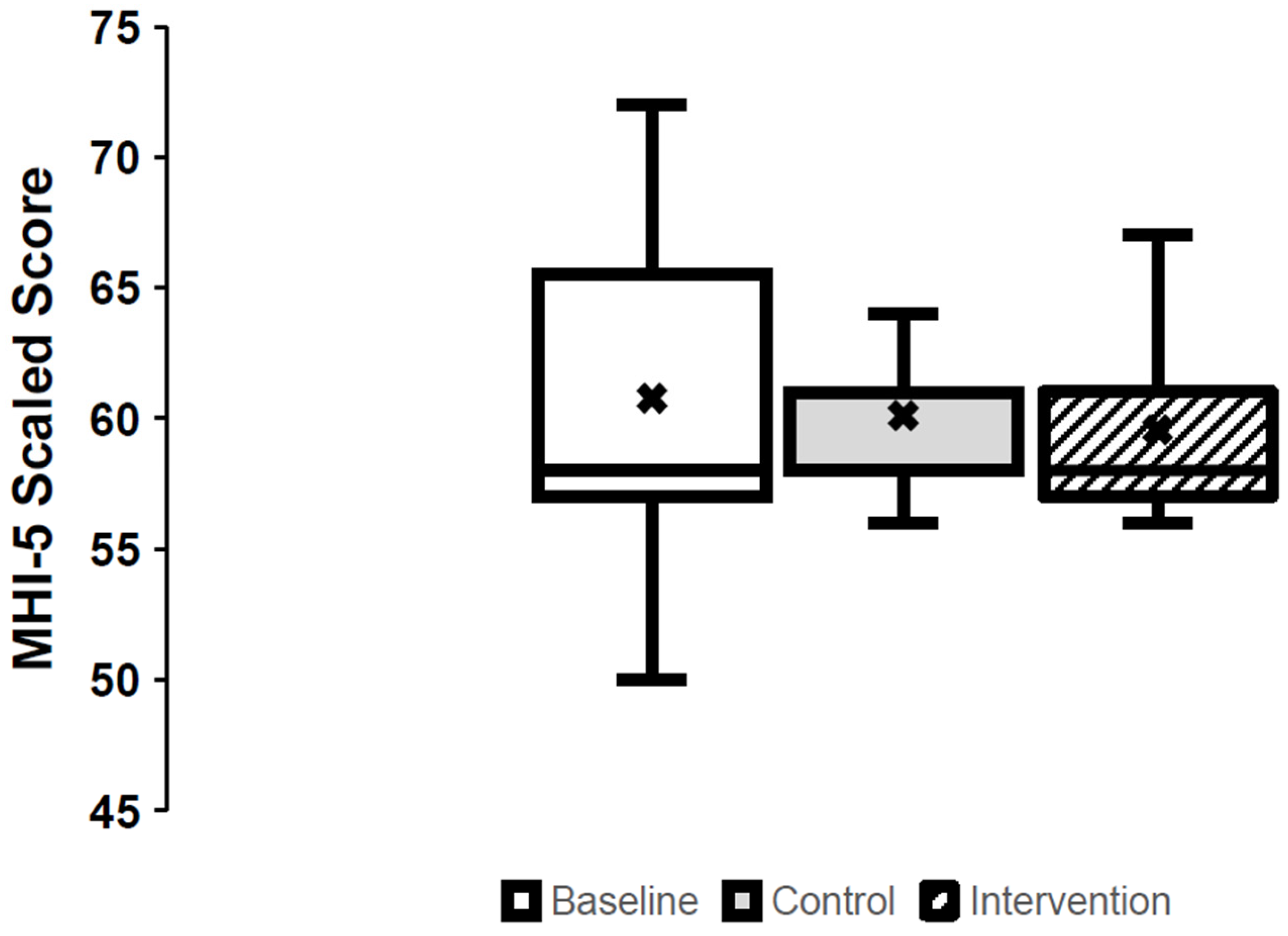
3.1. Mental Health (Figure 1)
3.2. Sleepiness
3.3. Pain (Table 2)
| Question | Baseline | Control | Intervention | p-Value | ES (CI) |
|---|---|---|---|---|---|
| Number of days with pain, median (IQR) | 7.0 (0.0, 7.0) | 6.5 (2.0, 7.0) | 4.0 (0.0, 7.0) | 0.156 | 0.25 (−2–0) |
| Worst pain intensity in last week, median (IQR) | 3.0 (0.50, 7.50) | 3.0 (0.0, 5.3) | 3.0 (0.0, 6.0) | 0.076 | 0.16 (0–1) |
| Pain unpleasantness, median (IQR) | 2.0 (0.5, 6.0) | 3.0 (0.0, 4.3) | 2.0 (0.0, 3.0) | 0.504 | 0.29 (−2–0) |
| Number of days with manageable/tolerable pain, median (IQR) | 5.5 (1.0, 7.0) | 5.0 (0.0, 7.0) | 3.0 (0.0, 6.0) | 0.494 | 0.28 (−4–0) |
| Pain intensity presently, median (IQR) | 3.0 (0.0, 5.5) | 2.0 (0.0, 3.5) | 1.0 (0.0, 4.5) | 0.039 | 0.29 (−3–0) |
| Length of time the pain lasts for, n (% of respondents) | 0.008 | ||||
| ≤1 min | 1 (10) | 2 (20) | 2 (20) | ||
| >1 min but <1 h | 0 (0) | 0 (0) | 0 (0) | ||
| ≥1 h but <24 h | 2 (20) | 1 (10) | 1 (10) | ||
| ≥24 h | 1 (10) | 1 (10) | 0 (0) | ||
| Constant/continuous | 4 (40) | 5 (50) | 5 (50) | ||
| Unknown | 1 (10) | 1 (10) | 1 (10) | ||
| Unanswered | 1 (10) | 0 (0) | 1 (10) | ||
| When during the day is the pain most intense, n (% of respondents) | 0.174 | ||||
| Morning (06:01–12:00) | 1 (10) | 1 (10) | 1 (10) | ||
| Afternoon (12:01–18:00) | 1 (10) | 0 (0) | 0 (0) | ||
| Evening (18:01–24:00) | 2 (20) | 1 (10) | 3 (30) | ||
| Night (0:01–06:00) | 1 (10) | 4 (40) | 3 (30) | ||
| Unpredictable (pain is not consistently more intense at any one time of day) | 3 (30) | 4 (40) | 2 (20) | ||
| Unanswered | 2 (20) | 0 (0) | 1 (10) |
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sankari, A.; Badr, M.S.; Martin, J.L.; Ayas, N.T.; Berlowitz, D.J. Impact Of Spinal Cord Injury On Sleep: Current Perspectives. Nat. Sci. Sleep 2019, 11, 219–229. [Google Scholar] [CrossRef]
- Post, M.; van Leeuwen, C. Psychosocial issues in spinal cord injury: A review. Spinal Cord 2012, 50, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Hunt, C.; Moman, R.; Peterson, A.; Wilson, R.; Covington, S.; Mustafa, R.; Murad, M.H.; Hooten, W.M. Prevalence of chronic pain after spinal cord injury: A systematic review and meta-analysis. Reg. Anesth. Pain. Med. 2021, 46, 328–336. [Google Scholar] [CrossRef]
- Bresnahan, J.J.; Scoblionko, B.R.; Zorn, D.; Graves, D.E.; Viscusi, E.R. The demographics of pain after spinal cord injury: A survey of our model system. Spinal Cord Ser. Cases 2022, 8, 14. [Google Scholar] [CrossRef]
- Yong, R.J.; Mullins, P.M.; Bhattacharyya, N. Prevalence of chronic pain among adults in the United States. Pain 2022, 163, e328–e332. [Google Scholar] [CrossRef] [PubMed]
- Le, J.; Dorstyn, D. Anxiety prevalence following spinal cord injury: A meta-analysis. Spinal Cord 2016, 54, 570–578, Correction in: Spinal Cord 2016, 54, 626. https://doi.org/10.1038/sc.2016.69. [Google Scholar] [CrossRef]
- Biering-Sørensen, F.; Biering-Sørensen, M. Sleep disturbances in the spinal cord injured: An epidemiological questionnaire investigation, including a normal population. Spinal Cord 2001, 39, 505–513. [Google Scholar] [CrossRef]
- Shafazand, S.; Anderson, K.D.; Nash, M.S. Sleep Complaints and Sleep Quality in Spinal Cord Injury: A Web-Based Survey. J. Clin. Sleep Med. 2019, 15, 719–724. [Google Scholar] [CrossRef]
- Rikard, S.M.; Strahan, A.E.; Schmit, K.M.; Guy, G.P. Chronic Pain Among Adults—United States, 2019–2021. MMWR Morb. Mortal Wkly Rep. 2023, 72, 379–385. [Google Scholar] [CrossRef]
- A Alnawwar, M.; I Alraddadi, M.; A Algethmi, R.; A Salem, G.; A Salem, M.; A Alharbi, A. The Effect of Physical Activity on Sleep Quality and Sleep Disorder: A Systematic Review. Cureus 2023, 15, e43595. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 4, CD011279. [Google Scholar] [CrossRef] [PubMed]
- Maynou, L.; Hernández-Pizarro, H.M.; Errea Rodríguez, M. The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 4771. [Google Scholar] [CrossRef] [PubMed]
- Chekroud, S.R.; Gueorguieva, R.; Zheutlin, A.B.; Paulus, M.; Krumholz, H.M.; Krystal, J.H.; Chekroud, A.M. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: A cross-sectional study. Lancet Psychiatry 2018, 5, 739–746. [Google Scholar] [CrossRef]
- Tamminen, N.; Reinikainen, J.; Appelqvist-Schmidlechner, K.; Borodulin, K.; Mäki-Opas, T.; Solin, P. Associations of physical activity with positive mental health: A population-based study. Ment. Health Phys. Act. 2020, 18, 100319. [Google Scholar] [CrossRef]
- Ponzano, M.; Buren, R.; Adams, N.T.; Jun, J.; Jetha, A.; Mack, D.E.; Ginis, K.A.M. Effect of Exercise on Mental Health and Health-related Quality of Life in Adults With Spinal Cord Injury: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2024, 105, 2350–2361. [Google Scholar] [CrossRef] [PubMed]
- Hearn, J.H.; Finlay, K.A. Internet-delivered mindfulness for people with depression and chronic pain following spinal cord injury: A randomized, controlled feasibility trial. Spinal Cord 2018, 56, 750–761. [Google Scholar] [CrossRef]
- Trbovich, M.; Wu, B.; Koek, W.; Wecht, J.; Kellogg, D. Are Thermoregulatory Sweating and Active Vasodilation in Skin Controlled by Separate Nerves During Passive Heat Stress in Persons With Spinal Cord Injury? Top. Spinal Cord. Inj. Rehabil. 2022, 28, 84–95. [Google Scholar] [CrossRef]
- Lubrano, E.; Mazas, P.F.; Freiwald, J.; Krüger, K.; Grattagliano, I.; Mur, E.; Silva, R.Q.; Maruri, G.R.; de Medeiros, L.S. An International Multidisciplinary Delphi-Based Consensus on Heat Therapy in Musculoskeletal Pain. Pain. Ther. 2023, 12, 93–110. [Google Scholar] [CrossRef]
- Koroglu, S.; Yıldız, M. Effectiveness of hydrotherapy and balneotherapy for anxiety and depression symptoms: A meta-analysis. Curr. Psychol. 2024, 43, 24193–24204. [Google Scholar] [CrossRef]
- Curković, B.; Vitulić, V.; Babić-Naglić, D.; Dürrigl, T. The influence of heat and cold on the pain threshold in rheumatoid arthritis. Z. Rheumatol. 1993, 52, 289–291. [Google Scholar]
- Ely, B.R.; Francisco, M.A.; Halliwill, J.R.; Bryan, S.D.; Comrada, L.N.; Larson, E.A.; Brunt, V.E.; Minson, C.T. Heat therapy reduces sympathetic activity and improves cardiovascular risk profile in women who are obese with polycystic ovary syndrome. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2019, 317, R630–R640. [Google Scholar] [CrossRef] [PubMed]
- Marchand, F.; Perretti, M.; McMahon, S.B. Role of the immune system in chronic pain. Nat. Rev. Neurosci. 2005, 6, 521–532. [Google Scholar] [CrossRef]
- Kubota, K.; Kurabayashi, H.; Tamura, K.; Kawada, E.; Tamura, J.I.; Shirakura, T. A transient rise in plasma β-endorphin after a traditional 47 °C hot-spring bath in Kusatsu-spa, Japan. Life Sci. 1992, 51, 1877–1880. [Google Scholar] [CrossRef]
- Engström, Å.; Hägglund, H.; Lee, E.; Wennberg, M.; Söderberg, S.; Andersson, M. Sauna bathing in northern Sweden: Results from the MONICA study 2022. Int. J. Circumpolar Health 2024, 83, 2419698. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Queiroz, S.S.; Andersen, M.L.; Mônico-Neto, M.; da Silveira Campos, R.M.; Roizenblatt, S.; Tufik, S.; de Mello, M.T. Passive body heating improves sleep patterns in female patients with fibromyalgia. Clinics 2013, 68, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Haghayegh, S.; Khoshnevis, S.; Smolensky, M.H.; Diller, K.R.; Castriotta, R.J. Before-bedtime passive body heating by warm shower or bath to improve sleep: A systematic review and meta-analysis. Sleep. Med. Rev. 2019, 46, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Mishima, Y.; Hozumi, S.; Shimizu, T.; Hishikawa, Y.; Mishima, K. Passive body heating ameliorates sleep disturbances in patients with vascular dementia without circadian phase-shifting. Am. J. Geriatr. Psychiatry 2005, 13, 369–376. [Google Scholar] [CrossRef]
- Tai, Y.; Obayashi, K.; Yamagami, Y.; Kurumatani, N.; Saeki, K. Association Between Passive Body Heating by Hot Water Bathing Before Bedtime and Depressive Symptoms Among Community-Dwelling Older Adults. Am. J. Geriatr. Psychiatry 2022, 30, 161–170. [Google Scholar] [CrossRef]
- Coombs, G.B.; Barak, O.F.; Phillips, A.A.; Mijacika, T.; Sarafis, Z.K.; Lee, A.H.X.; Squair, J.W.; Bammert, T.D.; DeSouza, N.M.; Gagnon, D.; et al. Acute heat stress reduces biomarkers of endothelial activation but not macro-or microvascular dysfunction in cervical spinal cord injury. Am. J. Physiol.-Heart Circ. Physiol. 2019, 316, H722–H733. [Google Scholar] [CrossRef]
- Leicht, C.A.; Kouda, K.; Umemoto, Y.; Banno, M.; Kinoshita, T.; Moriki, T.; Nakamura, T.; Bishop, N.C.; Goosey-Tolfrey, V.L.; Tajima, F. Hot water immersion induces an acute cytokine response in cervical spinal cord injury. Eur. J. Appl. Physiol. 2015, 115, 2243–2252. [Google Scholar] [CrossRef]
- Trbovich, M.; Wu, Y.; Koek, W.; Wecht, J.; Kellogg, D. Elucidating mechanisms of attenuated skin vasodilation during passive heat stress in persons with spinal cord injury. J. Spinal Cord Med. 2024, 47, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Trbovich, M.; Wu, Y.; Koek, W.; Zhao, J.; Kellogg, D. Impact of tetraplegia vs. paraplegia on venoarteriolar, myogenic and maximal cutaneous vasodilation responses of the microvasculature: Implications for cardiovascular disease. J. Spinal Cord Med. 2022, 45, 49–57. [Google Scholar] [CrossRef]
- van Leeuwen, C.M.; van der Woude, L.H.; Post, M.W. Validity of the mental health subscale of the SF-36 in persons with spinal cord injury. Spinal Cord 2012, 50, 707–710. [Google Scholar] [CrossRef]
- Friedman, B.; Heisel, M.; Delavan, R. Validity of the SF-36 five-item Mental Health Index for major depression in functionally impaired, community-dwelling elderly patients. J. Am. Geriatr. Soc. 2005, 53, 1978–1985. [Google Scholar] [CrossRef] [PubMed]
- Zürcher, C.; Tough, H.; Fekete, C.; SwiSCI Study Group. Mental health in individuals with spinal cord injury: The role of socioeconomic conditions and social relationships. PLoS ONE 2019, 14, e0206069. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Widerström-Noga, E.; Biering-Sørensen, F.; Bryce, T.N.; Cardenas, D.D.; Finnerup, N.B.; Jensen, M.P.; Richards, J.S.; Richardson, E.J.; Siddall, P.J. The International Spinal Cord Injury Pain Extended Data Set (Version 1.0). Spinal Cord 2016, 54, 1036–1046. [Google Scholar] [CrossRef]
- Rowbotham, M.C. What is a ‘clinically meaningful’reduction in pain? Pain 2001, 94, 131–132. [Google Scholar] [CrossRef] [PubMed]
- Naumann, J.; Sadaghiani, C. Therapeutic benefit of balneotherapy and hydrotherapy in the management of fibromyalgia syndrome: A qualitative systematic review and meta-analysis of randomized controlled trials. Arthritis Res. Ther. 2014, 16, R141. [Google Scholar] [CrossRef]
- Bai, R.; Li, C.; Xiao, Y.; Sharma, M.; Zhang, F.; Zhao, Y. Effectiveness of spa therapy for patients with chronic low back pain: An updated systematic review and meta-analysis. Medicine 2019, 98, e17092. [Google Scholar] [CrossRef]
- Oosterveld, F.G.J.; Rasker, J.J.; Floors, M.; Landkroon, R.; van Rennes, B.; Zwijnenberg, J.; van de Laar, M.A.F.J.; Koel, G.J. Infrared sauna in patients with rheumatoid arthritis and ankylosing spondylitis. A pilot study showing good tolerance, short-term improvement of pain and stiffness, and a trend towards long-term beneficial effects. Clin. Rheumatol. 2009, 28, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.-H.; Kim, N.-H.; Kim, H.-C.; Yang, Y.-H.; Kim, J.; Hwang, B. Dry sauna therapy is beneficial for patients with low back pain. Anesth. Pain. Med. 2019, 14, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Jo, Y.-Y.; Kim, Y.H.; Park, C.-K. Current insights and therapeutic strategies for targeting TRPV1 in neuropathic pain management. Life Sci. 2024, 355, 122954. [Google Scholar] [CrossRef]
- Chadwick, A.L.; Shi, C.; McMillan, M.; Miller, J.; Hu, J.; Geiger, P.C. The impact of a heat therapy intervention on pain and fibromyalgia symptoms in patients with fibromyalgia: A pilot study. Front. Pain Res. 2025, 6, 1526491. [Google Scholar] [CrossRef]
- Dönmez, A.; Karagülle, M.Z.; Tercan, N.; Dinler, M.; İşsever, H.; Turan, M. SPA therapy in fibromyalgia: A randomised controlled clinic study. Rheumatol. Int. 2005, 26, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Hulsebosch, C.E.; Hains, B.C.; Crown, E.D.; Carlton, S.M. Mechanisms of chronic central neuropathic pain after spinal cord injury. Brain Res. Rev. 2009, 60, 202–213. [Google Scholar] [CrossRef]
- Ely, B.R.; Clayton, Z.S.; McCurdy, C.E.; Pfeiffer, J.; Needham, K.W.; Comrada, L.N.; Minson, C.T. Heat therapy improves glucose tolerance and adipose tissue insulin signaling in polycystic ovary syndrome. Am. J. Physiol. Endocrinol. Metab. 2019, 317, E172–E182. [Google Scholar] [CrossRef]
- Tanaka, K.; Kuzumaki, N.; Hamada, Y.; Suda, Y.; Mori, T.; Nagumo, Y.; Narita, M. Elucidation of the mechanisms of exercise-induced hypoalgesia and pain prolongation due to physical stress and the restriction of movement. Neurobiol. Pain 2023, 14, 100133. [Google Scholar] [CrossRef]
- Masuda, A.; Nakazato, M.; Kihara, T.; Minagoe, S.; Tei, C. Repeated Thermal Therapy Diminishes Appetite Loss and Subjective Complaints in Mildly Depressed Patients. Psychosom. Med. 2005, 67, 643–647. [Google Scholar] [CrossRef]
- Hanusch, K.U.; Janssen, C.W. The impact of whole-body hyperthermia interventions on mood and depression–are we ready for recommendations for clinical application? Int. J. Hyperth. 2019, 36, 572–580. [Google Scholar] [CrossRef]
- Janssen, C.W.; Lowry, C.A.; Mehl, M.R.; Allen, J.J.B.; Kelly, K.L.; Gartner, D.E.; Medrano, A.; Begay, T.K.; Rentscher, K.; White, J.J.; et al. Whole-Body Hyperthermia for the Treatment of Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016, 73, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Putkonen, P.T.S.; Eloma, E. Sauna and physiological sleep: Increased slow-wave sleep after heat exposure. In Sauna Studies; The Finnish Sauna Society: Helsinki, Finland, 1976; pp. 270–279. [Google Scholar]
- Liao, W.C. Effects of passive body heating on body temperature and sleep regulation in the elderly: A systematic review. Int. J. Nurs. Stud. 2002, 39, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Spong, J.; Graco, M.; Brown, D.J.; Schembri, R.; Berlowitz, D.J. Subjective sleep disturbances and quality of life in chronic tetraplegia. Spinal Cord 2015, 53, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Portugal, E.M.M.; Cevada, T.; Monteiro-Junior, R.S.; Guimarães, T.T.; Rubini, E.d.C.; Lattari, E.; Blois, C.; Deslandes, A.C. Neuroscience of exercise: From neurobiology mechanisms to mental health. Neuropsychobiology 2013, 68, 1–14. [Google Scholar] [CrossRef]
- Ogawa, T.; Hoekstra, S.P.; Kamijo, Y.-I.; Goosey-Tolfrey, V.L.; Walsh, J.J.; Tajima, F.F.; Leicht, C.A. Serum and plasma brain-derived neurotrophic factor concentration are elevated by systemic but not local passive heating. PLoS ONE 2021, 16, e0260775. [Google Scholar] [CrossRef]
- LaVela, S.L.; Etingen, B.; Miskevics, S.; Cella, D. Use of PROMIS-29® in US Veterans: Diagnostic Concordance and Domain Comparisons with the General Population. J. Gen. Intern. Med. 2019, 34, 1452–1458. [Google Scholar] [CrossRef]
| Age in years, mean (SD) | 45 (14) |
| Years since injury, mean (SD) | 9.2 (10.5) |
| Lesion level at time of study, n (%) | |
| Cervical, C4–C7 | 4 (40) |
| Thoracic, T5–T12 | 6 (60) |
| AIS completeness at time of study, n (%) | |
| A | 4 (40) |
| B | 1 (10) |
| C | 4 (40) |
| D | 1 (10) |
| BMI in kg/m2, mean (SD) | 28.0 (3.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uhlig-Reche, H.; Hoekstra, S.; Wu, Y.; Kellogg, D.L., Jr.; Romo, T.; Leicht, C.A.; Trbovich, M.B. The Effect of Eight Weeks of Passive Heat Therapy on Mental Health, Sleep, and Chronic Pain in Persons with Spinal Cord Injury: A Pilot Study. J. Clin. Med. 2025, 14, 3566. https://doi.org/10.3390/jcm14103566
Uhlig-Reche H, Hoekstra S, Wu Y, Kellogg DL Jr., Romo T, Leicht CA, Trbovich MB. The Effect of Eight Weeks of Passive Heat Therapy on Mental Health, Sleep, and Chronic Pain in Persons with Spinal Cord Injury: A Pilot Study. Journal of Clinical Medicine. 2025; 14(10):3566. https://doi.org/10.3390/jcm14103566
Chicago/Turabian StyleUhlig-Reche, Hannah, Sven Hoekstra, Yubo Wu, Dean Lundt Kellogg, Jr., Terry Romo, Christof A. Leicht, and Michelle B. Trbovich. 2025. "The Effect of Eight Weeks of Passive Heat Therapy on Mental Health, Sleep, and Chronic Pain in Persons with Spinal Cord Injury: A Pilot Study" Journal of Clinical Medicine 14, no. 10: 3566. https://doi.org/10.3390/jcm14103566
APA StyleUhlig-Reche, H., Hoekstra, S., Wu, Y., Kellogg, D. L., Jr., Romo, T., Leicht, C. A., & Trbovich, M. B. (2025). The Effect of Eight Weeks of Passive Heat Therapy on Mental Health, Sleep, and Chronic Pain in Persons with Spinal Cord Injury: A Pilot Study. Journal of Clinical Medicine, 14(10), 3566. https://doi.org/10.3390/jcm14103566







