Acupuncture for Anxiety, Depression, and Sleep in Veterans with Combat-Related Posttraumatic Stress Disorder: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
2.1. Trial Design, Participants, and Setting
2.2. Recruitment, Inclusion/Exclusion Criteria, and Withdrawal Rules
2.3. Randomization and Blinding
2.4. Outcomes and Measures
2.4.1. General Approach
2.4.2. The Hamilton Anxiety Rating Scale (HAM-A)
2.4.3. Beck Depression Inventory—II (BDI-II)
2.4.4. Pittsburgh Sleep Quality Index (PSQI)
2.4.5. Safety Assessment
2.5. Interventions
2.6. Data Management and Analyses
2.7. Ethics and Safety
3. Results
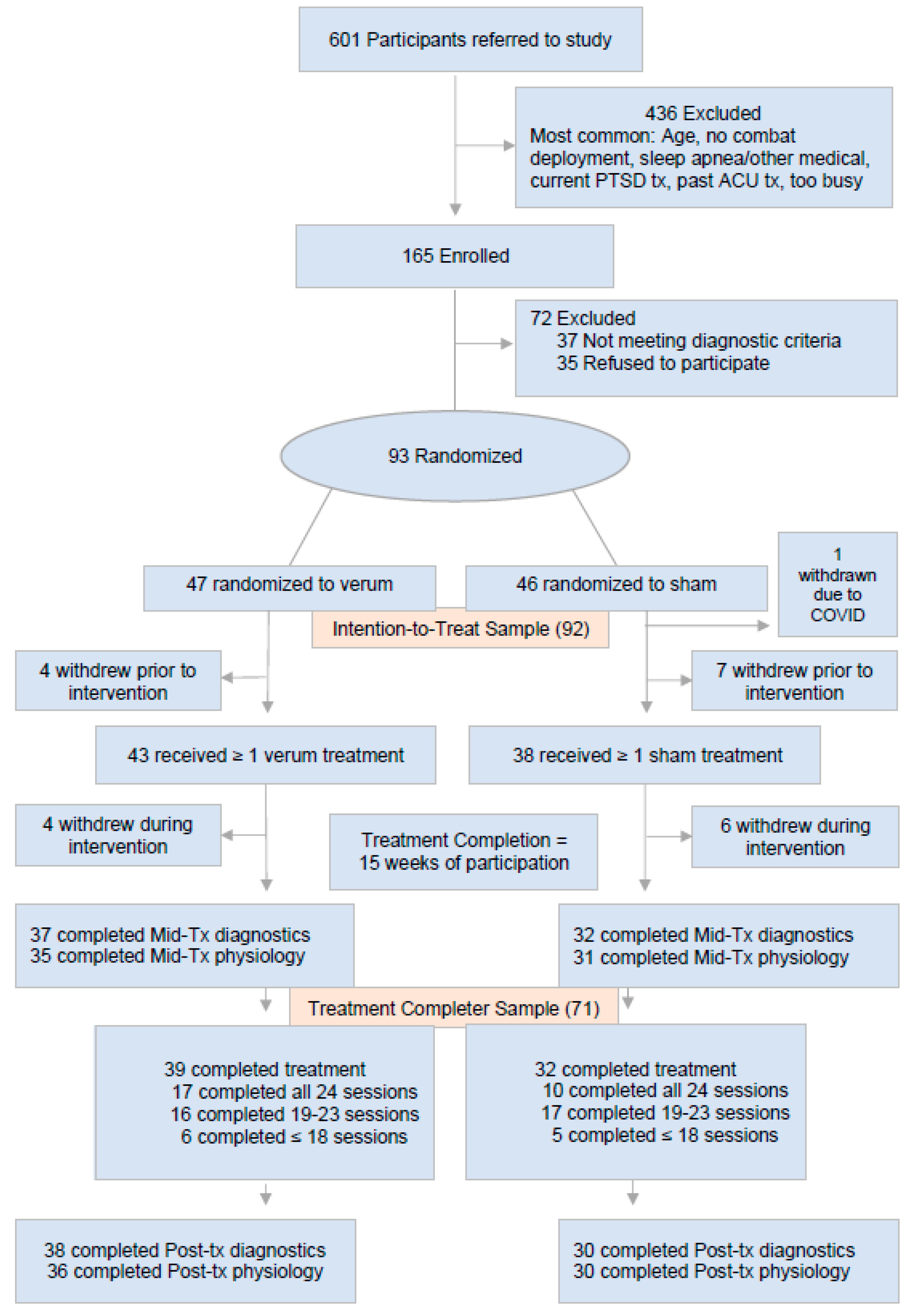
3.1. Demographics, Clinical Characteristics, and Study Flow
3.2. Primary Endpoints
- Intragroup Analyses
- Intergroup Analyses
- Intragroup Analyses
- Intergroup Analyses
- Intragroup Analyses
- Intergroup Analyses
4. Discussion
4.1. Principal Findings
4.2. Results in the Context of Other Research
4.3. Strengths and Limitations
5. Conclusions: Toward Implementation and Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eisenberg, D.M.; Davis, R.B.; Ettner, S.L.; Appel, S.; Wilkey, S.; Van Rompay, M.; Kessler, R.C. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA 1998, 280, 1569–1575. [Google Scholar] [CrossRef] [PubMed]
- VA. FY 2015 VHA Complementary & Integrative Health (CIH) Services. 2015. Available online: https://sciencebasedmedicine.org/wp-content/uploads/2016/07/FY2015_VHA_CIH_signedReport.pdf (accessed on 1 January 2020).
- Schnurr, P.P.; Chard, K.M.; Ruzek, J.I.; Chow, B.K.; Resick, P.A.; Foa, E.B.; Marx, B.P.; Friedman, M.J.; Bovin, M.J.; Caudle, K.L.; et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: A randomized clinical trial. JAMA Netw. Open 2022, 5, e2136921. [Google Scholar] [CrossRef] [PubMed]
- Duek, O.; Pietrzak, R.H.; Petrakis, I.; Hoff, R.; Harpaz-Rotem, I. Early discontinuation of pharmacotherapy in US veterans diagnosed with PTSD and the role of psychotherapy. J. Psychiatr. Res. 2021, 132, 167–173. [Google Scholar] [CrossRef] [PubMed]
- VA. Provision of Complementary and Integrative Health (CIH). Veterans Health Administration. 2022; pp. 1–14. Available online: https://www.va.gov/VHApublications/ViewPublication.asp?pub_ID=10072 (accessed on 1 January 2024).
- Gaab, J.; Kossowsky, J.; Ehlert, U.; Locher, C. Effects and components of placebos with a psychological treatment rationale–three randomized-controlled studies. Sci. Rep. 2019, 9, 1421. [Google Scholar] [CrossRef]
- Pilkington, K. Anxiety, depression and acupuncture: A review of the clinical research. Auton. Neurosci. 2010, 157, 91–95. [Google Scholar] [CrossRef]
- Amorim, D.; Brito, I.; Caseiro, A.; Figueiredo, J.P.; Pinto, A.; Macedo, I.; Machado, J. Electroacupuncture and acupuncture in the treatment of anxiety—A double blinded randomized parallel clinical trial. Complement. Ther. Clin. Pract. 2022, 46, 101541. [Google Scholar] [CrossRef]
- Tong, Q.Y.; Liu, R.; Zhang, K.; Gao, Y.; Cui, G.W.; Shen, W.D. Can acupuncture therapy reduce preoperative anxiety? A systematic review and meta-analysis. J. Integr. Med. 2021, 19, 20–28. [Google Scholar] [CrossRef]
- Fan, J.Q.; Lu, W.J.; Tan, W.Q.; Liu, X.; Wang, Y.-T.; Wang, N.-B.; Zhuang, L.-X. Effectiveness of acupuncture for anxiety among patients with parkinson disease: A randomized clinical trial. JAMA Netw. Open 2022, 5, e2232133. [Google Scholar] [CrossRef]
- Yin, X.; Li, W.; Liang, T.; Lu, B.; Yue, H.; Li, S.; Zhong, V.W.; Zhang, W.; Li, X.; Zhou, S.; et al. Effect of Electroacupuncture on Insomnia in Patients With Depression: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2220563. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, Y.; Qin, S.; Wang, X.; Jiang, Y.; Wu, W. Randomized controlled trial of acupuncture for anxiety and depression in patients with chronic insomnia. Ann. Transl. Med. 2021, 9, 1426. [Google Scholar] [CrossRef]
- Foa, E.B.; Riggs, D.S.; Dancu, C.V.; Rothbaum, B.O. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J. Trauma. Stress 1993, 6, 459–473. [Google Scholar] [CrossRef]
- Hollifield, M.; Sinclair-Lian, N.; Warner, T.D.; Hammerschlag, R. Acupuncture for posttraumatic stress disorder: A randomized controlled pilot trial. J. Nerv. Ment. Dis. 2007, 195, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Engel, C.C.; Cordova, E.H.; Benedek, D.M.; Liu, X.; Gore, K.L.; Goertz, C.; Freed, M.C.; Crawford, C.; Jonas, W.B.; Ursano, R.J. Randomized effectiveness trial of a brief course of acupuncture for posttraumatic stress disorder. Med. Care 2014, 52 (Suppl. 5), S57–S64. [Google Scholar] [CrossRef] [PubMed]
- Hollifield, M.; Hsiao, A.F.; Smith, T.; Calloway, T.; Jovanovic, T.; Smith, B.; Carrick, K.; Norrholm, S.D.; Munoz, A.; Alpert, R.; et al. Acupuncture for combat-related posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry 2024, 81, 545–554. [Google Scholar] [CrossRef]
- Hollifield, M.; Hsiao, A.F.; Carrick, K.; Munoz, A.G.; Calloway, T.; Cocozza, K.; Smith, B.; Smith, T.; Jovanovic, T.; Norrholm, S.; et al. Acupuncture for combat post-traumatic stress disorder: Trial development and methodological approach for a randomized controlled clinical trial. Trials 2021, 22, 594. [Google Scholar] [CrossRef]
- Scott, N.W.; McPherson, G.C.; Ramsay, C.R.; Campbell, M.K. The method of minimization for allocation to clinical trials. a review. Control Clin. Trials 2002, 23, 662–674. [Google Scholar] [CrossRef]
- Treasure, T.; MacRae, K.D. Minimisation: The platinum standard for trials? randomisation doesn’t guarantee similarity of groups; minimisation does. BMJ 1998, 317, 362–363. [Google Scholar] [CrossRef]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Garbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H., 3rd; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Buss, A.H.; Perry, M. The aggression questionnaire. J. Pers. Soc. Psychol. 1992, 63, 452–459. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G. Beck Depression Inventory-II (BDI-II); APA PsychTests; APA PsycNet: Champaign, IL, USA, 1996. [Google Scholar] [CrossRef]
- Stastical Analysis System [Computer Software], Version 9.4; Analydata: San Diego, CA, USA, 2013.
- Park, J.; White, A.; Stevinson, C.; Ernst, E.; James, M. Validating a new non-penetrating sham acupuncture device: Two randomised controlled trials. Acupunct. Med. 2002, 20, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Schnyer, R.N.; Iuliano, D.; Kay, J.; Shields, M.; Wayne, P. Development of protocols for randomized sham-controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis-related pelvic pain. J. Altern. Complement. Med. 2008, 14, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Gollub, R.L.; Rosman, I.S.; Webb, J.M.; Vangel, M.G.; Kirsch, I.; Kaptchuk, T.J. Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. J. Neurosci. 2006, 26, 381–388. [Google Scholar] [CrossRef]
- Shen, J.; Wenger, N.; Glaspy, J.; Hays, R.D.; Albert, P.S.; Choi, C.; Shekelle, P.G. Electroacupuncture for control of myeloablative chemotherapy–induced emesis: A randomized controlled trial. JAMA 2000, 284, 2755–2761. [Google Scholar] [CrossRef]
- Flachskampf, F.A.; Gallasch, J.; Gefeller, O.; Gan, J.; Mao, J.; Pfahlberg, A.B.; Wortmann, A.; Klinghammer, L.; Pflederer, W.; Daniel, W.G. Randomized trial of acupuncture to lower blood pressure. Circulation 2007, 115, 3121–3129. [Google Scholar] [CrossRef]
- Sinclair-Lian, N.; Hollifield, M.; Menache, M.; Warner, T.; Viscaya, J.; Hammerschlag, R. Developing a traditional chinese medicine diagnostic structure for post-traumatic stress disorder. J. Altern. Complement. Med. 2006, 12, 45–57. [Google Scholar] [CrossRef]
| Group | ||||||
|---|---|---|---|---|---|---|
| Population | Verum | Sham | ||||
| N | Mean, SD | N | Mean, SD | N | Mean, SD | |
| Clinical Characteristics | ||||||
| Hamilton Anxiety Rating Scale (HAMA) | 93 | 32.8, 9.5 | 47 | 33.6, 9.2 | 46 | 32.0, 9.7 |
| Beck’s Depression Inventory (BDI) | 92 | 31.4, 10.9 | 46 | 32.0, 11.0 | 46 | 30.7, 11.0 |
| Pittsburgh Sleep Quality Index (PSQT) | 93 | 14.2, 3.5 | 47 | 14.2, 3.7 | 46 | 14.2, 3.3 |
| Clinician-Administered PTSD Scale-5 (CAPS-5) | 92 | 36.9, 6.3 | 47 | 37.1, 6.7 | 45 | 36.6, 5.8 |
| N | (%) | N | (%) | N | (%) | |
| Age Group | ||||||
| 24–29 | 11 | (11.8) | 3 | (6.4) | 8 | (17.4) |
| 30–34 | 22 | (23.7) | 10 | (21.3) | 12 | (26.1) |
| 35–39 | 22 | (23.7) | 13 | (27.7) | 9 | (19.6) |
| 40–44 | 9 | (9.7) | 6 | (12.8) | 3 | (6.5) |
| 45–49 | 16 | (17.2) | 8 | (17.0) | 8 | (17.4) |
| 50+ | 13 | (14.0) | 7 | (14.9) | 6 | (13.0) |
| Sex | ||||||
| Male | 85 | (91.4) | 43 | (91.5) | 42 | (91.3) |
| Female | 8 | (8.6) | 4 | (8.5) | 4 | (8.7) |
| Country of Birth | ||||||
| USA | 72 | (77.4) | 35 | (74.5) | 37 | (80.4) |
| Other | 21 | (22.6) | 12 | (25.5) | 9 | (19.6) |
| Education Level | ||||||
| HS/GED | 19 | (20.4) | 12 | (25.5) | 7 | (15.2) |
| Some College | 39 | (41.9) | 18 | (38.3) | 21 | (45.7) |
| College Degree | 35 | (37.6) | 17 | (36.2) | 18 | (39.1) |
| Marital Status | ||||||
| Married | 46 | (49.5) | 24 | (51.1) | 22 | (47.8) |
| Single | 20 | (21.5) | 13 | (27.7) | 7 | (15.2) |
| Divorced | 21 | (22.6) | 8 | (17.0) | 13 | (28.3) |
| Other | 6 | (6.5) | 2 | (4.3) | 4 | (8.7) |
| Religion | ||||||
| Buddhist | 4 | (4.3) | 3 | (6.4) | 1 | (2.2) |
| Christian | 46 | (49.5) | 22 | (46.8) | 24 | (52.2) |
| Muslim | 2 | (2.2) | 0 | 0 | 2 | (4.3) |
| Other | 21 | (22.6) | 10 | (21.3) | 11 | (23.9) |
| None | 20 | (21.5) | 12 | (25.5) | 8 | (17.4) |
| Live With Self | ||||||
| No | 64 | (68.8) | 33 | (70.2) | 31 | (67.4) |
| Yes | 29 | (31.2) | 14 | (29.8) | 15 | (32.6) |
| Live With Spouse | ||||||
| No | 49 | (52.7) | 24 | (51.1) | 25 | (54.3) |
| Yes | 44 | (47.3) | 23 | (48.9) | 21 | (45.7) |
| Live With Children | ||||||
| No | 62 | (66.7) | 31 | (66.0) | 31 | (67.4) |
| Yes | 31 | (33.3) | 16 | (34.0) | 15 | (32.6) |
| Live With Parents | ||||||
| No | 78 | (83.9) | 37 | (78.7) | 41 | (89.1) |
| Yes | 15 | (16.1) | 10 | (21.3) | 5 | (10.9) |
| Live With Relatives | ||||||
| No | 86 | (92.5) | 44 | (93.6) | 42 | (91.3) |
| Yes | 7 | (7.5) | 3 | (6.4) | 4 | (8.7) |
| Live With Others | ||||||
| No | 79 | (84.9) | 41 | (87.2) | 38 | (82.6) |
| Yes | 14 | (15.1) | 6 | (12.8) | 8 | (17.4) |
| Annual Income | ||||||
| Missing | 1 | (1.1) | 1 | (2.1) | 0 | 0 |
| USD 0–19,999 | 13 | (14.0) | 3 | (6.4) | 10 | (21.7) |
| USD 20,000–34,999 | 14 | (15.1) | 6 | (12.8) | 8 | (17.4) |
| USD 35,000–49,999 | 22 | (23.7) | 13 | (27.7) | 9 | (19.6) |
| >USD 50,000 | 43 | (46.2) | 24 | (51.1) | 19 | (41.3) |
| Employed | ||||||
| No | 51 | (54.8) | 30 | (63.8) | 21 | (45.7) |
| Yes | 42 | (45.2) | 17 | (36.2) | 25 | (54.3) |
| Work Hours | ||||||
| <40 | 16 | (17.2) | 6 | (12.8) | 10 | (21.7) |
| 40 | 22 | (23.7) | 12 | (25.5) | 10 | (21.7) |
| >40 | 7 | (7.5) | 1 | (2.1) | 6 | (13.0) |
| Missing | 48 | (51.6) | 28 | (59.6) | 20 | (43.5) |
| Race | ||||||
| American Indian/Alaskan Native | 2 | (2.2) | 2 | (4.3) | 0 | 0 |
| White | 44 | (47.3) | 23 | (48.9) | 21 | (45.7) |
| Asian | 17 | (18.3) | 8 | (17.0) | 9 | (19.6) |
| Black/African American | 12 | (12.9) | 5 | (10.6) | 7 | (15.2) |
| More than one | 15 | (16.1) | 6 | (12.8) | 9 | (19.6) |
| Unknown | 3 | (3.2) | 3 | (6.4) | 0 | 0 |
| Ethnicity | ||||||
| Hispanic | 43 | (46.2) | 23 | (48.9) | 20 | (43.5) |
| Non-Hispanic | 50 | (53.8) | 24 | (51.1) | 26 | (56.5) |
| Combat Exposure | ||||||
| Light | 3 | (3.2) | 1 | (2.1) | 2 | (4.3) |
| Moderate Light | 16 | (17.2) | 8 | (17.0) | 8 | (17.4) |
| Moderate | 31 | (33.3) | 16 | (34.0) | 15 | (32.6) |
| Moderate Heavy | 28 | (30.1) | 14 | (29.8) | 14 | (30.4) |
| Heavy | 15 | (16.1) | 8 | (17.0) | 7 | (15.2) |
| Deployment Preparedness | ||||||
| Low Preparedness | 7 | (7.5) | 4 | (8.5) | 3 | (6.5) |
| Moderate Preparedness | 46 | (49.5) | 23 | (48.9) | 23 | (50.0) |
| High Preparedness | 40 | (43.0) | 20 | (42.6) | 20 | (43.5) |
| Pre-Treatment | Mid-Treatment | Post-Treatment | ||
|---|---|---|---|---|
| N | Mean (SD) | Mean (SD) | Mean (SD) | |
| Intention to Treat *** | ||||
| Total Randomized | 93 | 32.8 (9.5) | N = 74, 23.1 (10.6) | N = 72, 21.1 (11.2) |
| Verum * | 47 | 33.6 (9.2) | N = 38, 23.3 (10.8) | N = 39, 19.4 (10.3) |
| Sham * | 46 | 32.0 (9.7) | N = 36, 22.9 (10.6) | N = 33, 23.2 (12.1) |
| Treatment Completers **** | ||||
| Total Sample | 71 | 33.1 (9.6) | N = 69, 23.0 (10.7) | N = 68, 20.6 (11.1) |
| Verum ** | 39 | 33.4 (9.7) | N = 37, 22.9 (10.8) | N = 38, 18.8 (9.7) |
| Sham ** | 32 | 32.8 (9.5) | N = 32, 23.1 (10.7) | N = 30, 22.8 (12.5) |
| Pre-Treatment | Mid-Treatment | Post-Treatment | ||
|---|---|---|---|---|
| N | Mean (SD) | Mean (SD) | Mean (SD) | |
| Intention to Treat *** | ||||
| Total Sample | 92 | 31.4 (10.9) | N = 74, 21.1 (11.3) | N = 71, 18.5 (13.0) |
| Verum * | 46 | 32.0 (11.0) | N = 38, 20.5 (10.7) | N = 39, 17.5 (11.9) |
| Sham * | 46 | 30.7 (11.0) | N = 36, 21.6 (12.0) | N = 32, 19.6 (14.4) |
| Treatment Completers **** | ||||
| Total Sample | 70 | 31.0 (11.3) | N = 69, 20.6 (11.3) | N = 67, 18.1 (13.0) |
| Verum ** | 38 | 30.6 (11.2) | N = 37, 20.2 (10.6) | N = 38, 17.0 (11.5) |
| Sham ** | 32 | 31.6 (11.7) | N = 32, 21.2 (12.3) | N = 29, 19.4 (14.9) |
| Pre-Treatment | Mid-Treatment | Post-Treatment | ||
|---|---|---|---|---|
| N | Mean (SD) | Mean (SD) | Mean (SD) | |
| Intention to Treat *** | ||||
| Total Sample | 93 | 14.2 (3.5) | N = 74, 13.2 (3.8) | N = 72, 12.0 (4.2) |
| Verum * | 47 | 14.2 (3.7) | N = 38, 12.9 (4.1) | N = 39, 11.2 (4.4) |
| Sham * | 46 | 14.2 (3.3) | N = 36, 13.5 (3.6) | N = 33, 13.0 (3.8) |
| Treatment Completers **** | ||||
| Total Sample | 71 | 14.0 (3.5) | N = 69, 13.0 (3.8) | N = 68, 11.8 (4.2) |
| Verum ** | 39 | 13.9 (3.8) | N = 37, 12.8 (4.1) | N = 38, 11.1 (4.5) |
| Sham ** | 32 | 14.1 (3.2) | N = 32, 13.3 (3.4) | N = 30, 12.7 (3.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsiao, A.-F.; Lai-Trzebiatowski, J.; Smith, T.; Calloway, T.; Aden, C.; Jovanovic, T.; Smith, B.; Carrick, K.; Munoz, A.; Jung, M.; et al. Acupuncture for Anxiety, Depression, and Sleep in Veterans with Combat-Related Posttraumatic Stress Disorder: A Randomized Controlled Trial. J. Clin. Med. 2025, 14, 3443. https://doi.org/10.3390/jcm14103443
Hsiao A-F, Lai-Trzebiatowski J, Smith T, Calloway T, Aden C, Jovanovic T, Smith B, Carrick K, Munoz A, Jung M, et al. Acupuncture for Anxiety, Depression, and Sleep in Veterans with Combat-Related Posttraumatic Stress Disorder: A Randomized Controlled Trial. Journal of Clinical Medicine. 2025; 14(10):3443. https://doi.org/10.3390/jcm14103443
Chicago/Turabian StyleHsiao, An-Fu, Jennifer Lai-Trzebiatowski, Tyler Smith, Teresa Calloway, Chelsea Aden, Tanja Jovanovic, Besa Smith, Kala Carrick, Andrea Munoz, Megan Jung, and et al. 2025. "Acupuncture for Anxiety, Depression, and Sleep in Veterans with Combat-Related Posttraumatic Stress Disorder: A Randomized Controlled Trial" Journal of Clinical Medicine 14, no. 10: 3443. https://doi.org/10.3390/jcm14103443
APA StyleHsiao, A.-F., Lai-Trzebiatowski, J., Smith, T., Calloway, T., Aden, C., Jovanovic, T., Smith, B., Carrick, K., Munoz, A., Jung, M., & Hollifield, M. (2025). Acupuncture for Anxiety, Depression, and Sleep in Veterans with Combat-Related Posttraumatic Stress Disorder: A Randomized Controlled Trial. Journal of Clinical Medicine, 14(10), 3443. https://doi.org/10.3390/jcm14103443







