Impact of Different Types of Physical Exercises for the Management of Older Women with Urinary Incontinence: A Systematic Review of Randomized Clinical Trials
Abstract
1. Introduction
2. Material and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
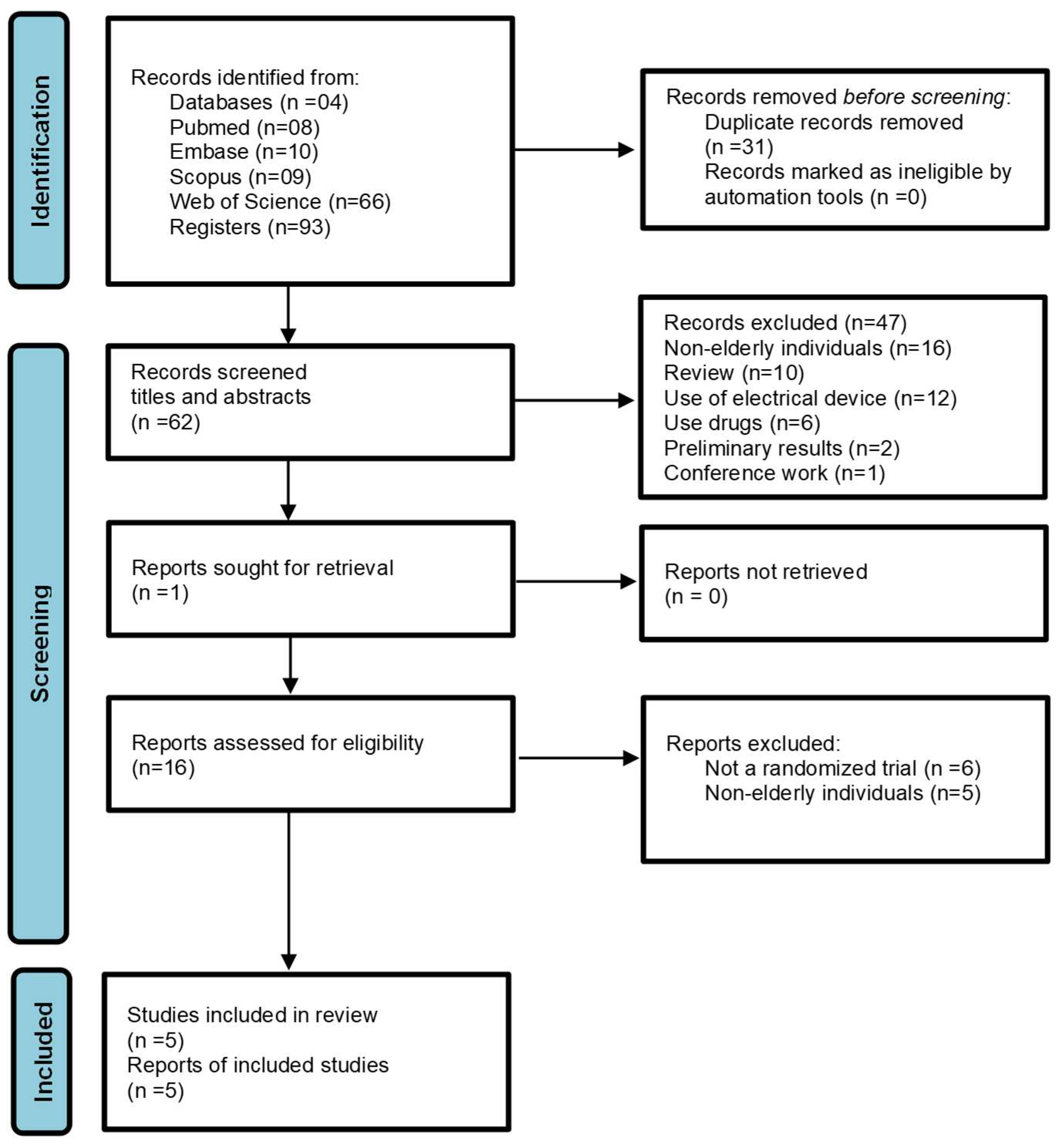
2.3. Study Selection and Data Extraction
2.4. Risk of Bias
3. Results
3.1. Study Characteristics
3.2. Intervention Protocols
3.3. Assessed Outcomes
3.4. Quality of Life
3.5. UI Severity
3.6. Pelvic Floor Muscle Training (Evaluated by Digital Palpation)
3.7. Physical Performance and Risk of Fall
3.8. Daily Urinary Forms
3.8.1. Urinary Symptoms
3.8.2. Bother Score (VAS)
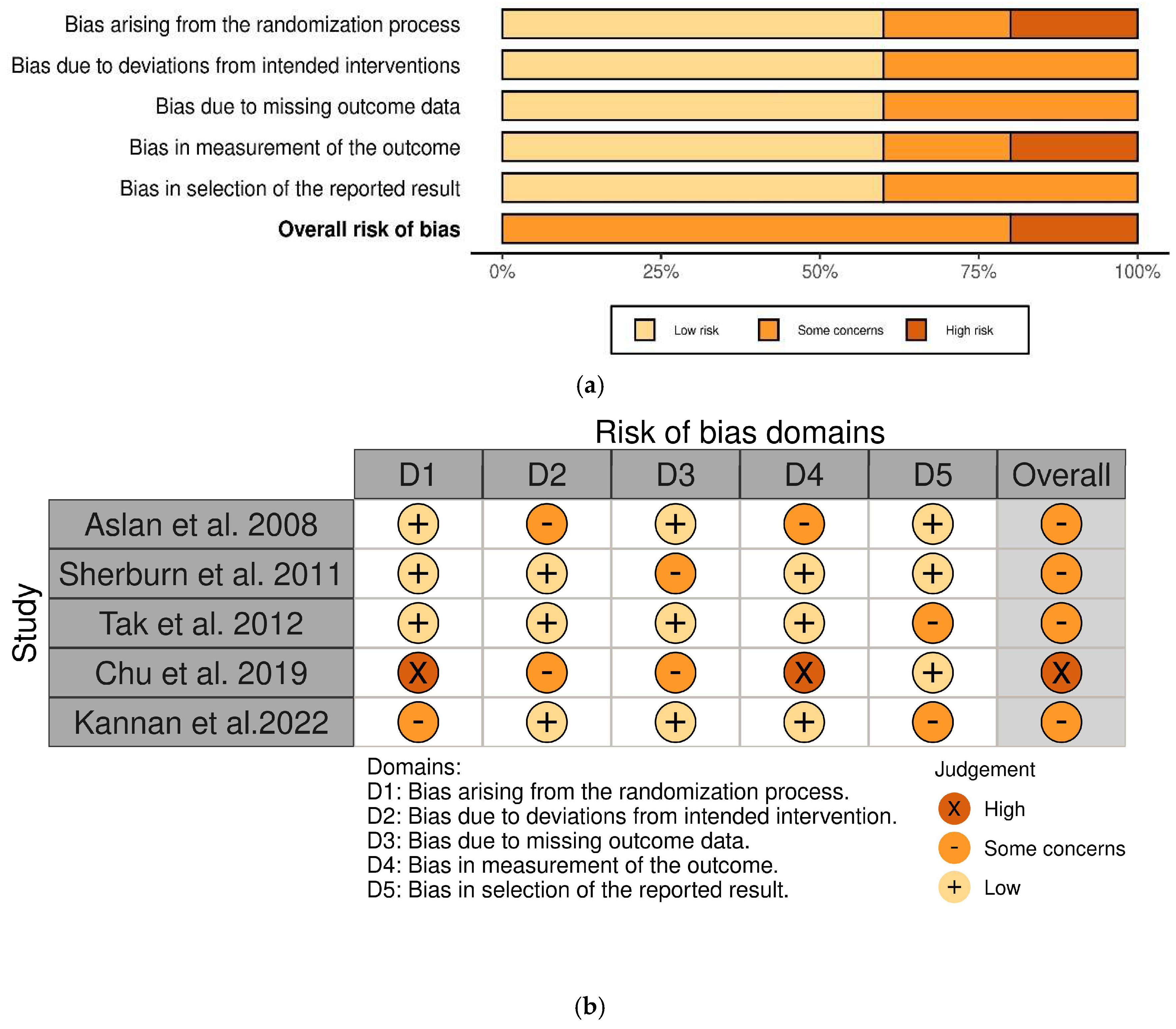
3.8.3. Risk of Bias
3.9. Performance Bias
3.9.1. Allocation
3.9.2. Assessments of Results
4. Discussion
4.1. Limitations of the Study
4.2. Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Z.; Zhang, Z.; Ren, Y.; Wang, Y.; Fang, J.; Yue, H.; Ma, S.; Guan, F. Aging and age-related diseases: From mechanisms to therapeutic strategies. Biogerontology 2021, 22, 165–187. [Google Scholar] [CrossRef] [PubMed]
- Flint, B.; Tadi, P. Physiology, Aging. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Milsom, I.; Coyne, K.S.; Nicholson, S.; Kvasz, M.; Chen, C.I.; Wein, A.J. Global prevalence and economic burden of urgency urinary incontinence: A systematic review. Eur. Urol. 2014, 65, 79–95. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, M.; Etiler, N. Addressing urinary incontinence by gender: A nationwide population-based study in Turkiye. BMC Urol. 2023, 23, 205. [Google Scholar] [CrossRef] [PubMed]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric 2019, 22, 217–222. [Google Scholar] [CrossRef]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018, 10, CD005654. [Google Scholar] [CrossRef]
- Kołodyńska, G.; Zalewski, M.; Rożek-Piechura, K. Urinary incontinence in postmenopausal women—Causes, symptoms, treatment. Menopause Rev. Przegląd Menopauzalny 2019, 18, 46–50. [Google Scholar] [CrossRef]
- Vaughan, C.P.; Markland, A.D. Urinary Incontinence in Women. Ann. Intern. Med. 2020, 172, ITC17–ITC32. [Google Scholar] [CrossRef]
- Corrado, B.; Giardulli, B.; Polito, F.; Aprea, S.; Lanzano, M.; Dodaro, C. The Impact of Urinary Incontinence on Quality of Life: A Cross-Sectional Study in the Metropolitan City of Naples. Geriatrics 2020, 5, 96. [Google Scholar] [CrossRef]
- Szychowska, A.; Drygas, W. Physical activity as a determinant of successful aging: A narrative review article. Aging Clin. Exp. Res. 2022, 34, 1209–1214. [Google Scholar] [CrossRef]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- Townsend, M.K.; Curhan, G.C.; Resnick, N.M.; Grodstein, F. BMI, waist circumference, and incident urinary incontinence in older women. Obesity 2008, 16, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.H.; Hirayama, F. Physical activity and urinary incontinence in older adults: A community-based study. Curr. Aging Sci. 2012, 5, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Farzinmehr, A.; Moezy, A.; Koohpayehzadeh, J.; Kashanian, M. A Comparative Study of Whole Body Vibration Training and Pelvic Floor Muscle Training on Women’s Stress Urinary Incontinence: Three- Month Follow-Up. J. Fam. Reprod. Health 2015, 9, 147–154. [Google Scholar] [PubMed] [PubMed Central]
- Gonzaga, S.; de Oliveira, R.G.; Dutra, L.L.; Oliveira, L.S.; de Oliveira, L.C. Comparative analysis of pelvic floor muscle training and Pilates in managing urinary incontinence among postmenopausal women: A randomized controlled trial. Int. Urogynecol. J. 2024, 35, 561–569. [Google Scholar] [CrossRef]
- Kim, G.S.; Kim, E.G.; Shin, K.Y.; Choo, H.J.; Kim, M.J. Combined pelvic muscle exercise and yoga program for urinary incontinence in middle-aged women. Jpn. J. Nurs. Sci. 2015, 12, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Evidence-based Complementary and Alternative Medicine. Evid.-Based Complement. Altern. Med. 2006, 3, 555–558. [CrossRef] [PubMed] [PubMed Central]
- O’Connor, E.; Nic An Riogh, A.; Karavitakis, M.; Monagas, S.; Nambiar, A. Diagnosis and Non-Surgical Management of Urinary Incontinence—A Literature Review with Recommendations for Practice. Int. J. Gen. Med. 2021, 14, 4555–4565. [Google Scholar] [CrossRef]
- Bø, K. Urinary Incontinence, Pelvic Floor Dysfunction, Exercise and Sport. Sports Med. 2004, 34, 451–464. [Google Scholar] [CrossRef]
- Cho, S.T.; Kim, K.H. Pelvic floor muscle exercise and training for coping with urinary incontinence. J. Exerc. Rehabil. 2021, 17, 379–387. [Google Scholar] [CrossRef]
- Fitz, F.F.; Gimenez, M.M.; de Azevedo Ferreira, L.; Matias, M.M.P.; Bortolini, M.A.T.; Castro, R.A. Effects of voluntary pre-contraction of the pelvic floor muscles (the Knack) on female stress urinary incontinence—A study protocol for a RCT. Trials 2021, 22, 484. [Google Scholar] [CrossRef]
- Hady, D.A.A.; Mabrouk, O.M.; Osman, D.A. Ultrasound imaging of core muscles activity in multiparous women with vaginal laxity: A cross-sectional study. Sci. Rep. 2024, 14, 149063. [Google Scholar] [CrossRef] [PubMed]
- Ashton-Miller, J.A.; DeLancey, J.O. Functional anatomy of the female pelvic floor. Ann. N. Y. Acad. Sci. 2007, 1101, 266–296. [Google Scholar] [CrossRef] [PubMed]
- Curillo-Aguirre, C.A.; Gea-Izquierdo, E. Effectiveness of Pelvic Floor Muscle Training on Quality of Life in Women with Urinary Incontinence: A Systematic Review and Meta-Analysis. Medicina 2023, 59, 1004. [Google Scholar] [CrossRef]
- Peinado-Molina, R.A.; Martínez-Vázquez, S.; Hernández-Martínez, A.; Martínez-Galiano, J.M. Impact and Influence of Urinary Incontinence on Physical Activity Levels. Eur. Urol. Open Sci. 2023, 55, 50–58. [Google Scholar] [CrossRef]
- Langhammer, B.; Bergland, A.; Rydwik, E. The Importance of Physical Activity Exercise among Older People. BioMed Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 1, 2. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. JMLA 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Rayyan: AI-Powered Systematic Review Management Platform [Internet]. Rayyan: AI-Powered Systematic Review Management Platform. Available online: https://www.rayyan.ai (accessed on 1 January 2025).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, 14898. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions [Internet]. Available online: https://dariososafoula.wordpress.com/wp-content/uploads/2017/01/cochrane-handbook-for-systematic-reviews-of-interventions-2019-1.pdf (accessed on 1 January 2025).
- Higgins, J.P.T.; Morgan, R.L.; Rooney, A.A.; Taylor, K.W.; Thayer, K.A.; Silva, R.A.; Lemeris, C.; Akl, E.A.; Bateson, T.F.; Berkman, N.D.; et al. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ. Int. 2024, 186, 108602. [Google Scholar] [CrossRef]
- Aslan, E.; Komurcu, N.; Beji, N.K.; Yalcin, O. Bladder training and Kegel exercises for women with urinary complaints living in a rest home. Gerontology 2008, 54, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Sherburn, M.; Bird, M.; Carey, M.; Bø, K.; Galea, M.P. Incontinence improves in older women after intensive pelvic floor muscle training: An assessor-blinded randomized controlled trial. Neurourol. Urodyn. 2011, 30, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Tak, E.C.; van Hespen, A.; van Dommelen, P.; Hopman-Rock, M. Does improved functional performance help to reduce urinary incontinence in institutionalized older women? A multicenter randomized clinical trial. BMC Geriatr. 2012, 12, 51. [Google Scholar] [CrossRef]
- Chu, C.M.; Schmitz, K.H.; Khanijow, K.; Stambakio, H.; Newman, D.K.; Arya, L.A.; Andy, U.U. Feasibility and outcomes: Pilot Randomized Controlled Trial of a home-based integrated physical exercise and bladder-training program vs usual care for community-dwelling older women with urinary incontinence. Neurourol. Urodyn. 2019, 38, 1399–1408. [Google Scholar] [CrossRef]
- Kannan, P.; Hsu, W.H.; Suen, W.T.; Chan, L.M.; Assor, A.; Ho, C.M. Yoga and Pilates compared to pelvic floor muscle training for urinary incontinence in elderly women: A randomised controlled pilot trial. Complement. Ther. Clin. Pract. 2022, 46, 101502. [Google Scholar] [CrossRef]
- Aoki, Y.; Brown, H.W.; Brubaker, L.; Cornu, J.N.; Daly, J.O.; Cartwright, R. Urinary incontinence in women. Nat. Rev. Dis. Primers 2017, 3, 17042. [Google Scholar] [CrossRef]
- Imamura, M.; Williams, K.; Wells, M.; McGrother, C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database Syst. Rev. 2015, 2015, CD003505. [Google Scholar] [CrossRef]
- Cross, D.; Waheed, N.; Krake, M.; Gahreman, D. Effectiveness of supervised Kegel exercises using bio-feedback versus unsupervised Kegel exercises on stress urinary incontinence: A quasi-experimental study. Int. Urogynecol. J. 2023, 34, 913–920. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sigurdardottir, T.; Steingrimsdottir, T.; Geirsson, R.T.; Halldorsson, T.I.; Aspelund, T.; Bø, K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence?: An assessor-blinded randomized controlled trial. Am. J. Obstet. Gynecol. 2020, 222, 247.e1–247.e8. [Google Scholar] [CrossRef]
- Woodley, S.J.; Lawrenson, P.; Boyle, R.; Cody, J.D.; Mørkved, S.; Kernohan, A.; Hay-Smith, E.J.C. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2020, 5, CD007471. [Google Scholar] [CrossRef]
- Tsikopoulos, I.; Lazarou, L.; Tzelves, L.; Sakalis, V.; Papathanasiou, C.; Samarinas, M. The effect of pelvic floor muscle training on urodynamic parameters in women with stress urinary incontinence. Cent. Eur. J. Urol. 2023, 76, 315–321. [Google Scholar] [CrossRef]
- Kharaji, G.; ShahAli, S.; Ebrahimi-Takamjani, I.; Sarrafzadeh, J.; Sanaei, F.; Shanbehzadeh, S. Supervised versus unsupervised pelvic floor muscle training in the treatment of women with urinary incontinence—A systematic review and meta-analysis. Int. Urogynecol. J. 2023, 34, 1339–1349. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, L.P.; Dumoulin, C.; Hay-Smith, E.J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A cochrane systematic review abridged republication. Braz. J. Phys. Ther. 2019, 23, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Todhunter-Brown, A.; Hazelton, C.; Campbell, P.; Elders, A.; Hagen, S.; McClurg, D. Conservative interventions for treating urinary incontinence in women: An Overview of Cochrane systematic reviews. Cochrane Database Syst. Rev. 2022, 9, CD012337. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yıldız, N.; Özlü, A. Factors predicting the treatment success of bladder training for urgency urinary incontinence. Neurourol. Urodyn. 2022, 41, 1809–1816. [Google Scholar] [CrossRef]
- Åström, Y.; Asklund, I.; Lindam, A.; Sjöström, M. Quality of life in women with urinary incontinence seeking care using e-health. BMC Womens Health 2021, 21, 337. [Google Scholar] [CrossRef]
- AlQuaiz, A.M.; Kazi, A.; AlYousefi, N.; Alwatban, L.; AlHabib, Y.; Turkistani, I. Urinary Incontinence Affects the Quality of Life and Increases Psychological Distress and Low Self-Esteem. Healthcare 2023, 11, 1772. [Google Scholar] [CrossRef]
- Abu Raddaha, A.H.; Nasr, E.H. Kegel Exercise Training Program among Women with Urinary Incontinence. Healthcare 2022, 10, 2359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Author | Population/Age (Years Old) | Groups/Sample (n) | Outcomes | Intervention | Observed impacts |
|---|---|---|---|---|---|
| Aslan et al., 2008 [34] | Living at a rest home/70–89 | Treatment Group: 25 Control Group: 25 |
| Intervention 6–8 weeks, BT, and Kegel exercises Control: BT and the PFMT were not performed |
|
| Sherburn et al., 2011 [35] | Community-dwelling women/over 65 | PFMT group: 43 BT group: 41 |
| PFMT group: 5-month exercise/session lasting 1 h, educational component and exercise for music class incorporating PFMT. Intensive PFMT, combining motor control, strength, endurance, power and functional training. BT Group: As in the PFMT group, each weekly group session began with an educational component followed by a gentle exercise for music class. Cognitive methods addressed the physiological control of the bladder and parameters related to bladder emptying, including guidance on skin care, adequate use of absorbent pads, management of water intake and adoption of the ideal posture during urination. |
|
| Tak et al., 2012 [36] | Institutionalized older women | Intervention group: 85 Control group: 70 |
| Intervention group: The Incondition program was structured in weekly 1 h training sessions for groups of 6 to 10 women over a 22-week period. Each session included behavioral and exercise training components. The behavioral intervention aimed to optimize urination control by improving knowledge about urinary continence, correcting behaviors related to using the bathroom (such as posture and relaxation techniques), and implementing BT and PFMT, with an emphasis on relaxation and breathing techniques. The exercise session, lasting 30 min, included warm-up activities, exercises aimed at improving upper limb mobility and hand function, as well as exercises involving getting up and sitting in a chair, walking and relaxation techniques. Control group: Participants received usual care, which included the use of pads to manage urinary incontinence and assistance with bathroom visits. |
|
| Chu et al., 2019 [37] | Local community centers and geriatric clinics women/65 and older | Experimental group: 17 Control group: 16 |
| Experimental group: Participants exercised three times a week using the “FlexToBa” (acronym for Flexibility, Tone, and Balance) home exercise program, consisting of six exercise modules distributed on digital media (DVDs) for progression over 24 weeks. In addition, a DVD for suppressing urinary urgency was used, associated with behavioral measures, both developed by a specialized nurse. A home visit was conducted in which a trained research coordinator provided written recommendations for adaptations to the home environment, based on a checklist for fall prevention. Control group: Participants in the usual care group were instructed to schedule an appointment with a urinary incontinence specialist or with a physical therapist/nurse specialized in UI rehabilitation. |
|
| Kannan et al., 2022 [38] | Elderly care centres/60 or above, | Yoga: 10 Pilates: 10 Standard care control: 10 |
| Supervised sessions once a week for four weeks, followed by unsupervised home exercises guided by a CD for eight weeks. Yoga group: Virabhadrasana and Parsvakonasana poses plus hatha style yoga, which included eight poses: Tadasana, Utkatasana, Trikonasana, Malasana, Viparita Karani Variation, Salamba Setu Bandhasana, Supta Baddha Konasana, and Savasana. Pilates Group: exercises targeting the pelvic floor and core muscles (transverse abdominis and multifidus). Exercises included Pilates breathing, knee swings, heel slides, pelvic clock, tailbone flexion, pelvic lift, roll down, leg springs, circles, single leg stretch, scissors, spinal stretch, and swan prep. Eight contractions were performed for each of these PFMT (24 contractions in each session). Each contraction lasted 5–6 s, followed by relaxation for 10 s. PFMT group: group initially performed exercises in antigravity positions (lateral, dorsal, ventral or quadrupedal decubitus) with subsequent progression to counter gravity positions (sitting and standing). Activities included urethral contraction, evacuation control and a combination of urethral orifice contraction, evacuation control and vaginal wall elevation. Each session involved eight sets of PFM exercises, totaling 24 contractions per session. Each contraction was held for five to six seconds, followed by a 10 s relaxation period. |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Rocha, W.S.; Reis-Silva, A.; Coelho-Oliveira, A.C.; Moura-Fernandes, M.C.; da Silva Alves Cunha, R.; Alhammad, A.; de Sá-Caputo, D.d.C.; Bernardo-Filho, M.; Taiar, R. Impact of Different Types of Physical Exercises for the Management of Older Women with Urinary Incontinence: A Systematic Review of Randomized Clinical Trials. J. Clin. Med. 2025, 14, 3425. https://doi.org/10.3390/jcm14103425
da Rocha WS, Reis-Silva A, Coelho-Oliveira AC, Moura-Fernandes MC, da Silva Alves Cunha R, Alhammad A, de Sá-Caputo DdC, Bernardo-Filho M, Taiar R. Impact of Different Types of Physical Exercises for the Management of Older Women with Urinary Incontinence: A Systematic Review of Randomized Clinical Trials. Journal of Clinical Medicine. 2025; 14(10):3425. https://doi.org/10.3390/jcm14103425
Chicago/Turabian Styleda Rocha, Waleska Souza, Aline Reis-Silva, Ana Carolina Coelho-Oliveira, Marcia Cristina Moura-Fernandes, Rosane da Silva Alves Cunha, Ayman Alhammad, Danúbia da Cunha de Sá-Caputo, Mario Bernardo-Filho, and Redha Taiar. 2025. "Impact of Different Types of Physical Exercises for the Management of Older Women with Urinary Incontinence: A Systematic Review of Randomized Clinical Trials" Journal of Clinical Medicine 14, no. 10: 3425. https://doi.org/10.3390/jcm14103425
APA Styleda Rocha, W. S., Reis-Silva, A., Coelho-Oliveira, A. C., Moura-Fernandes, M. C., da Silva Alves Cunha, R., Alhammad, A., de Sá-Caputo, D. d. C., Bernardo-Filho, M., & Taiar, R. (2025). Impact of Different Types of Physical Exercises for the Management of Older Women with Urinary Incontinence: A Systematic Review of Randomized Clinical Trials. Journal of Clinical Medicine, 14(10), 3425. https://doi.org/10.3390/jcm14103425










