The Impact of Multilevel Anterior Cervical Discectomy and Fusion on Cervical Sagittal Alignment: A Comparative Study of Single-, Two-, and Three-Level Procedures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
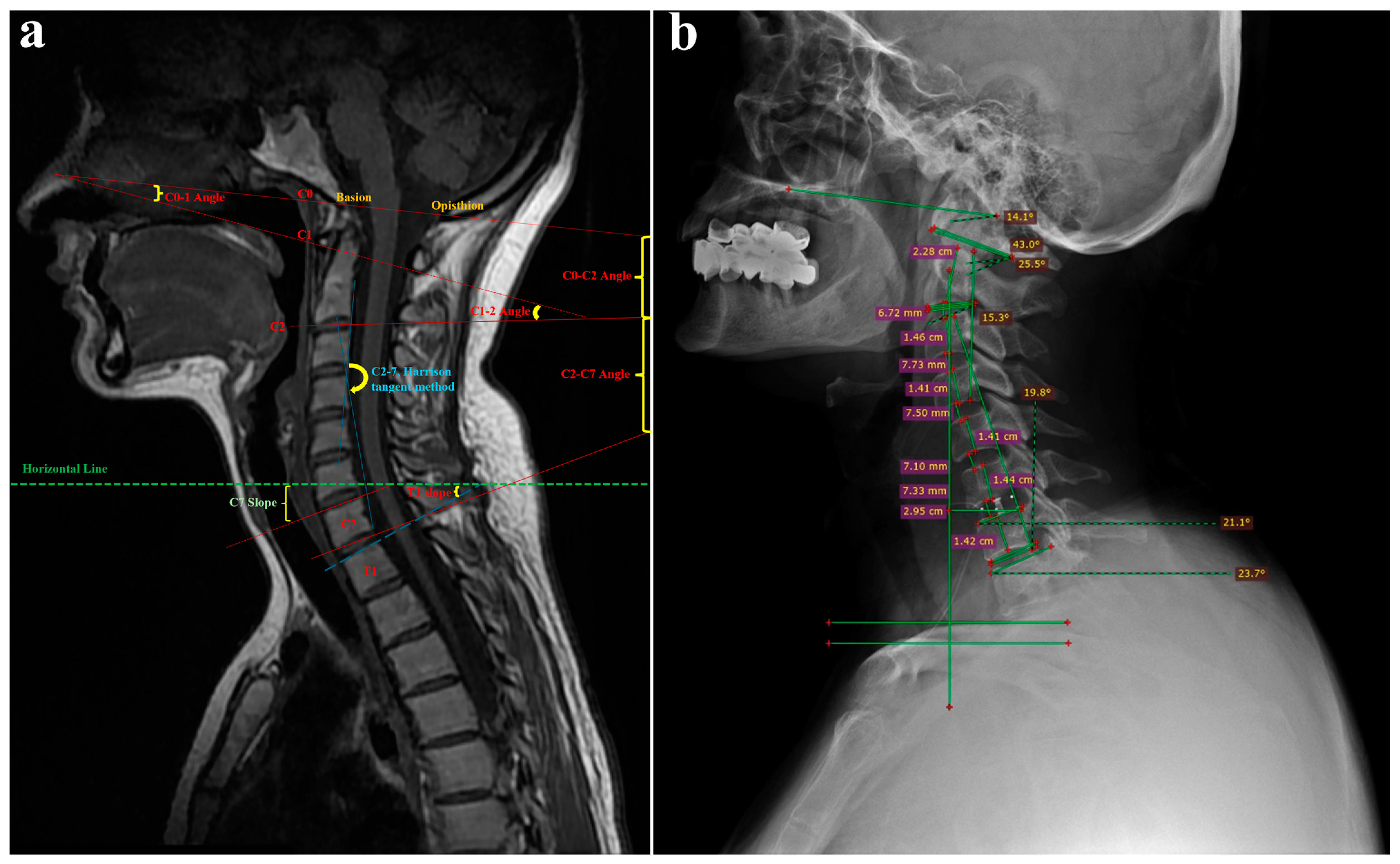
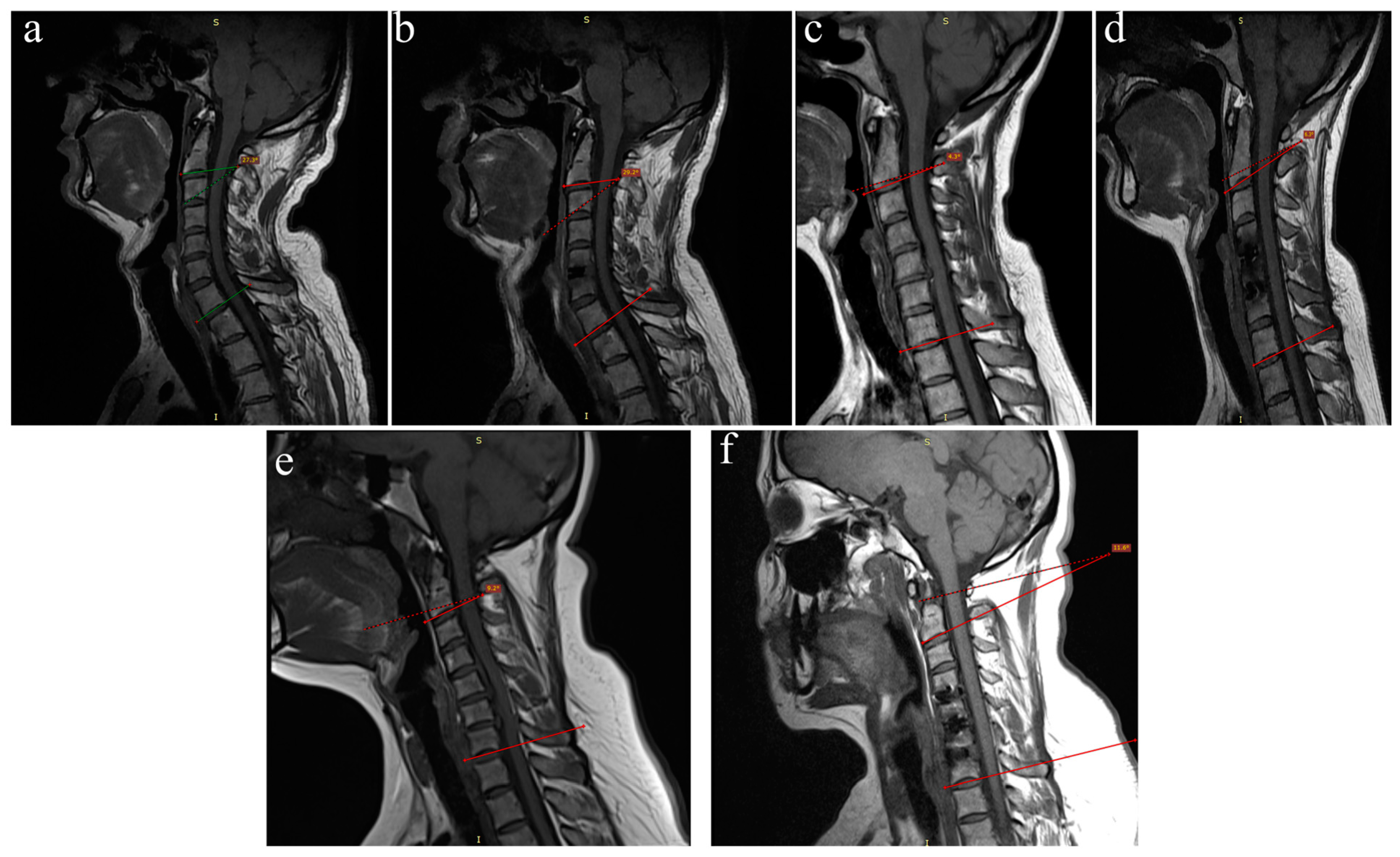
2.2. Radiological Assessment
2.3. Surgical Approach
2.4. Postoperative Follow-Up
2.5. Clinical and Radiological Assessment
2.6. Statistical Analysis
3. Results
3.1. Demographic Findings
3.2. Clinical Findings
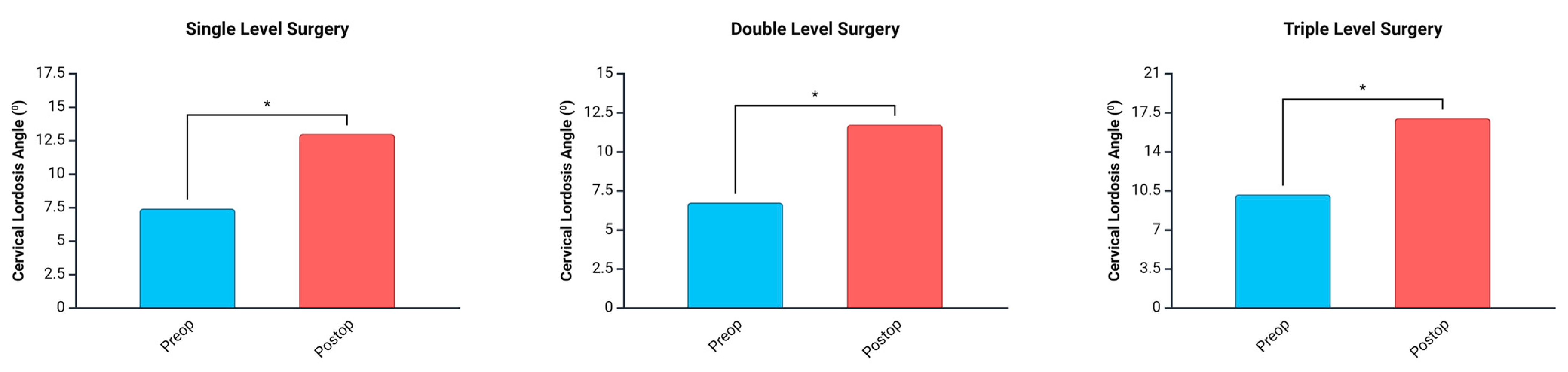
3.3. Radiological Results
3.4. Postoperative Follow-Up and Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Badhiwala, J.H.; Ahuja, C.S.; Akbar, M.A.; Witiw, C.D.; Nassiri, F.; Furlan, J.C.; Curt, A.; Wilson, J.R.; Fehlings, M.G. Degenerative cervical myelopathy—Update and future directions. Nat. Rev. Neurol. 2020, 16, 108–124. [Google Scholar] [CrossRef]
- Fakhoury, J.; Dowling, T.J. Cervical Degenerative Disc Disease; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Wang, X.-R.; Kwok, T.C.; Griffith, J.F.; Yu, B.W.; Leung, J.C.; Wáng, Y.X. Prevalence of cervical spine degenerative changes in elderly population and its weak association with aging, neck pain, and osteoporosis. Ann. Transl. Med. 2019, 7, 486. [Google Scholar] [CrossRef]
- Iyer, S.; Kim, H.J. Cervical radiculopathy. Curr. Rev. Musculoskelet. Med. 2016, 9, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Hejrati, N.; Pedro, K.; Alvi, M.A.; Quddusi, A.; Fehlings, M.G. Degenerative cervical myelopathy: Where have we been? Where are we now? Where are we going? Acta Neurochir. 2023, 165, 1105–1119. [Google Scholar] [CrossRef]
- Quek, C.X.; Goh, G.S.; Soh, R.C.C. Does Cervical Alignment Matter? The Effect of 2-level Anterior Cervical Discectomy and Fusion on Sagittal Alignment and Patient-reported Outcomes. Clin. Spine Surg. 2021, 34, E545–E551. [Google Scholar] [CrossRef]
- Dunn, C.; Moore, J.; Sahai, N.; Issa, K.; Faloon, M.; Sinha, K.; Emami, A. Minimally invasive posterior cervical foraminotomy with tubes to prevent undesired fusion: A long-term follow-up study. J. Neurosurg. Spine 2018, 29, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Yang, Y.; Wang, Y.; Liu, H.; Hong, Y.; Gong, Q.; Song, Y. Comparison of anterior cervical discectomy and fusion with the zero-profile device versus plate and cage in treating cervical degenerative disc disease: A meta-analysis. J. Clin. Neurosci. 2016, 33, 11–18. [Google Scholar] [CrossRef]
- Kani, K.K.; Chew, F.S. Anterior cervical discectomy and fusion: Review and update for radiologists. Skelet. Radiol. 2018, 47, 7–17. [Google Scholar] [CrossRef]
- Noordhoek, I.; Koning, M.T.; Vleggeert-Lankamp, C.L.A. Evaluation of bony fusion after anterior cervical discectomy: A systematic literature review. Eur. Spine J. 2019, 28, 386–399. [Google Scholar] [CrossRef] [PubMed]
- Nabhan, A.; Ahlhelm, F.; Shariat, K.; Pitzen, T.; Steimer, O.; Steudel, W.I.; Pape, D. The ProDisc-C prosthesis: Clinical and radiological experience 1 year after surgery. Spine 2007, 32, 1935–1941. [Google Scholar] [CrossRef]
- Gornet, M.F.; Lanman, T.H.; Burkus, J.K.; Dryer, R.F.; McConnell, J.R.; Hodges, S.D.; Schranck, F.W. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-Year outcomes of a prospective, randomized investigational device exemption clinical trial. J. Neurosurg. Spine 2019, 31, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Buttermann, G.R. Anterior Cervical Discectomy and Fusion Outcomes over 10 Years: A Prospective Study. Spine 2018, 43, 207–214. [Google Scholar] [CrossRef]
- Oshina, M.; Oshima, Y.; Tanaka, S.; Riew, K.D. Radiological Fusion Criteria of Postoperative Anterior Cervical Discectomy and Fusion: A Systematic Review. Glob. Spine J. 2018, 8, 739–750. [Google Scholar] [CrossRef]
- Riew, K.D.; Yang, J.J.; Chang, D.G.; Park, S.M.; Yeom, J.S.; Lee, J.S.; Jang, E.-C.; Song, K.S. What is the most accurate radiographic criterion to determine anterior cervical fusion? Spine J. 2019, 19, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.K.; Park, J.Y.; Kim, S.H.; Lim, D.J.; Kim, S.D.; Lee, S.K. Radiologic Assessment of Subsidence in Stand-Alone Cervical Polyetheretherketone (PEEK) Cage. J. Korean Neurosurg. Soc. 2008, 44, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Aebli, N.; Wicki, A.G.; Rüegg, T.B.; Petrou, N.; Eisenlohr, H.; Krebs, J. The Torg-Pavlov ratio for the prediction of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. 2013, 13, 605–612. [Google Scholar] [CrossRef]
- Calek, A.K.; Winkler, E.; Farshad, M.; Spirig, J.M. Pseudoarthrosis after anterior cervical discectomy and fusion: Rate of occult infections and outcome of anterior revision surgery. BMC Musculoskelet Disord 2023, 24, 688. [Google Scholar] [CrossRef]
- Arshi, A.; Wang, C.; Park, H.Y.; Blumstein, G.W.; Buser, Z.; Wang, J.C.; Shamie, A.N.; Park, D.Y. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: An analysis of a large nationwide database. Spine J. 2018, 18, 1180–1187. [Google Scholar] [CrossRef]
- Tally, W.C.; Tarabadkar, S.; Kovalenko, B.V. Safety and feasibility of outpatient ACDF in an ambulatory setting: A retrospective chart review. Int. J. Spine Surg. 2013, 7, e84–e87. [Google Scholar] [CrossRef]
- Villavicencio, A.T.; Pushchak, E.; Burneikiene, S.; Thramann, J.J. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J. 2007, 7, 148–153. [Google Scholar] [CrossRef]
- Zhu, B.; Xu, Y.; Liu, X.; Liu, Z.; Dang, G. Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy: A systemic review and meta-analysis. Eur. Spine J. 2013, 22, 1583–1593. [Google Scholar] [CrossRef]
- Han, Y.C.; Liu, Z.Q.; Wang, S.J.; Li, L.J.; Tan, J. Is anterior cervical discectomy and fusion superior to corpectomy and fusion for treatment of multilevel cervical spondylotic myelopathy? A systemic review and meta-analysis. PLoS ONE 2014, 9, e87191. [Google Scholar] [CrossRef] [PubMed]
- Knott, P.T.; Mardjetko, S.M.; Techy, F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010, 10, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, J.; Wei, X.; Guan, H.; Wang, B.; Xu, H.; Chen, J. The importance of preoperative T1 slope for determining proper postoperative C2–7 Cobb’s angle in patients undergoing cervical reconstruction. J. Orthop. Surg. Res. 2020, 15, 507. [Google Scholar] [CrossRef]
- Sakai, K.; Yoshii, T.; Hirai, T.; Arai, Y.; Torigoe, I.; Tomori, M.; Sato, H.; Okawa, A. Cervical Sagittal Imbalance is a Predictor of Kyphotic Deformity After Laminoplasty in Cervical Spondylotic Myelopathy Patients Without Preoperative Kyphotic Alignment. Spine 2016, 41, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Shi, C.; Wu, H.; Xu, Z.; Lin, W.; Shen, X.; Wu, X.D.; Zhang, Y.; Yuan, W. Application of Zero-profile Spacer in the Treatment of Three-level Cervical Spondylotic Myelopathy: 5-Year Follow-up Results. Spine 2020, 45, 504–511. [Google Scholar] [CrossRef]
- Dohzono, S.; Toyoda, H.; Takahashi, S.; Suzuki, A.; Terai, H.; Nakamura, H. Restrictions of cervical flexion after laminoplasty increase in the mechanical stress at the occipitocervical junction in non-rheumatoid arthritis patients. J. Clin. Neurosci. 2017, 45, 187–192. [Google Scholar] [CrossRef]
- Xiao, B.; Wu, B.; Rong, T.; Cui, W.; Sang, D.; Liu, B. Clinical impact of 3-level anterior cervical decompression and fusion (ACDF) on the occipito-atlantoaxial complex: A retrospective study of patients who received a zero-profile anchored spacer versus cage-plate construct. Eur. Spine J. 2021, 30, 3656–3665. [Google Scholar] [CrossRef]
- Spanos, S.L.; Siasios, I.D.; Dimopoulos, V.G.; Paterakis, K.N.; Mastrogiannis, D.S.; Giannis, T.P.; Fotiadou, A.A.; Pollina, J.; Fountas, K.N. Correlation of Clinical and Radiological Outcome After Anterior Cervical Discectomy and Fusion With a Polyetheretherketone Cage. J. Clin. Med. Res. 2018, 10, 268. [Google Scholar] [CrossRef]
- Núñez-Pereira, S.; Hitzl, W.; Bullmann, V.; Meier, O.; Koller, H. Sagittal balance of the cervical spine: An analysis of occipitocervical and spinopelvic interdependence, with C-7 slope as a marker of cervical and spinopelvic alignment. J. Neurosurg. Spine 2015, 23, 16–23. [Google Scholar] [CrossRef]
- Lau, D.; DiGiorgio, A.M.; Chan, A.K.; Ore, C.L.D.; Virk, M.S.; Chou, D.; Bisson, E.F.; Mummaneni, P.V. Applicability of cervical sagittal vertical axis, cervical lordosis, and T1 slope on pain and disability outcomes after anterior cervical discectomy and fusion in patients without deformity. J. Neurosurg. Spine 2020, 32, 23–30. [Google Scholar] [CrossRef]
- Godlewski, B.; Stachura, M.K.; Czepko, R.A.; Banach, M.; Czepko, R. Analysis of changes in cervical spinal curvature and intervertebral disk space height following ACDF surgery in a group of 100 patients followed up for 12 months. J. Clin. Neurosci. 2018, 52, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Poblete, J.; Martinez-Anda, J.J.; Rebollar-Mendoza, A.A.; Castro-Moreno, Y.; Torne, R.; Reyes, L.; Fuster, S.; Tornero, E.; Arch-Tirado, E.; de Leo-Vargas, R.; et al. Clinical and Radiological Outcome in a Series of Patients Treated by Anterior Cervical Discectomy and Fusion: Retrospective Controlled Study With 2 Different Stand-Alone Cages. Int. J. Spine Surg. 2022, 16, 779–791. [Google Scholar] [CrossRef]
- Guo, S.; Lu, S.; Kong, C.; Li, X.; Liu, C. Comparison of Clinical Outcomes and Sagittal Alignment After Different Levels of Anterior Cervical Discectomy and Fusion in Patients With Cervical Spondylotic Myelopathy: From One-level to Three-level. Spine 2021, 46, E153–E160. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Lü, G.; Wang, B.; Li, L.; Kuang, L. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: A retrospective study with 2-year follow-up. Eur. Spine J. 2016, 25, 2255–2262. [Google Scholar] [PubMed]
- Alhashash, M.; Allouch, H.; Boehm, H.; Shousha, M. Results of Four-Level Anterior Cervical Discectomy and Fusion Using Stand-Alone Interbody Titanium Cages. Asian Spine J. 2022, 16, 82–91. [Google Scholar] [CrossRef]
- Kwon, W.-K.; Kim, P.S.; Ahn, S.Y.; Song, J.Y.; Kim, J.H.; Park, Y.-K.; Kwon, T.-H.; Moon, H.J. Analysis of Associating Factors With C2-7 Sagittal Vertical Axis After Two-level Anterior Cervical Fusion: Comparison Between Plate Augmentation and Stand-alone Cages. Spine 2017, 42, 318–325. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, B.; Zhu, J.; Li, C.; Wei, F.; Yuan, Y.; Zhu, D. Comparison of Clinical and Radiologic Outcomes Between Self-Locking Stand-Alone Cage and Cage with Anterior Plate for Multilevel Anterior Cervical Discectomy and Fusion: A Meta-Analysis. World Neurosurg. 2019, 125, e117–e131. [Google Scholar] [CrossRef]
- Ryu, H.-S.; Han, M.S.; Lee, S.S.; Moon, B.J.; Lee, J.K. Influence of subsidence after stand-alone anterior cervical discectomy and fusion in patients with degenerative cervical disease: A long-term follow-up study. Medicine 2022, 101, e30673. [Google Scholar] [CrossRef]
- Elsayed, A.; Sakr, S. Fixation of multiple level anterior cervical disc using cages versus cages and plating. Egypt. J. Neurol. Psychiatry Neurosurg. 2019, 55, 12. [Google Scholar] [CrossRef]
- Singh, K.; Phillips, F.M.; Park, D.K.; Pelton, M.A.; An, H.S.; Goldberg, E.J. Factors affecting reoperations after anterior cervical discectomy and fusion within and outside of a Federal Drug Administration investigational device exemption cervical disc replacement trial. Spine J. 2012, 12, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Li, N.; Ding, Y.; Zhang, Z.; Jiang, W.; Jiang, T.; Qiao, Q.; Qian, Y.; Cheng, H. Incidence of Adjacent Segment Degeneration and Its Associated Risk Factors Following Anterior Cervical Discectomy and Fusion: A Meta-Analysis. World Neurosurg. 2024, 183, e153–e172. [Google Scholar] [CrossRef] [PubMed]
| n (%) | ||
|---|---|---|
| Level | ||
| Single | 36 (38.3) | |
| Double | 40 (42.6) | |
| Triple | 18 (19.1) | |
| Gender | ||
| Female | 46 (48.9) | |
| Male | 48 (51.1) | |
| Mean (SD) | Median (min/max) | |
| Age (years) | 50.83 (12.83) | 50 (22/78) |
| JOA Recovery Rate (%) | 93.9 (10.38) | 100 (68.75/100) |
| Group | Operated CDD Levels | n (%) |
|---|---|---|
| Single (n = 36) | C4-C5 | 2 (5.6) |
| C5-C6 | 22 (61.1) | |
| C6-C7 | 12 (33.3) | |
| Double (n = 40) | C4-C5/C5-C6 | 10 (25.0) |
| C5-C6/C6-C7 | 26 (65.0) | |
| C6-C7/C7-T1 | 4 (10.0) | |
| Triple (n = 18) | C3-C4/C5-C6/C6-C7 | 18 (100) |
| Single | Double | Triple | p | |
|---|---|---|---|---|
| (n = 36) | (n = 40) | (n = 18) | ||
| Age (years), mean (SD) | 46.33 (12.89) | 52.55 (11.17) | 56 (14.63) | 0.133 f |
| Gender, n (%) | 0.446 ff | |||
| Female | 22 (61.1) | 16 (40) | 8 (44.4) | |
| Male | 14 (38.9) | 24 (60) | 10 (55.6) | |
| JOA Recovery Rate (%), median (min/max) | 100 (75/100) | 100 (69.23/100) | 91.66 (68.75/100) A | 0.040 k |
| Preop/Postop/Change | ||||
| VAS, median (min/max) | 10 (9/10)/1 (1/2)/−9 (−9/−7) | 10 (9/10)/1 (1/3)/−8 (−9/−7) | 10 (9/10)/1 (1/3)/−8 (−9/−7) | 0.999 k/0.771 k/0.716 k |
| p value (preop vs. postop) | <0.001 ɯ | <0.001 ɯ | 0.003 ɯ | |
| Average Disc Height (mm), median (min/max) | 3.81 (1.31/6.84)/7.0 (5.0/8.66)/3.48 (−1.28/6.44) | 3.37 (1.91/5.12)/7.21 (5.83/8.67)/3.92 (2.84/5.29) | 3.66 (1.86/4.26)/7.58 (4.47/8.64)/3.59 (1.87/4.98) | 0.262 k/0.887 k/0.199 k |
| p value (preop vs. postop) | <0.001 ɯ | <0.001 ɯ | 0.004 ɯ | |
| Single | Double | Triple | p | |
|---|---|---|---|---|
| (n = 36) | (n = 40) | (n = 18) | ||
| Preop/Postop/Change | ||||
| C2-C3 disc height (mm), median (min/max) | 3.64 (1.34/7.49)/6.35 (3.95/8.55)/3.07 (−1.56/4.79) | 3.22 (1.96/7.22)/6.19 (4.59/7.53)/2.94 (−0.29/4.15) | 3.28 (2.21/4.93)/6 (2.13/6.82)/1.67 (−0.08/3.54) | 0.576 k/0.173 k/0.105 k |
| p value (preop vs. postop) | <0.001 ɯ | <0.001 ɯ | 0.007 ɯ | |
| C3-C4 disc height (mm), median (min/max) | 3.71 (1.28/7.21)/7.01 (4.44/8.51)/3.36 (−2.09/7.23) | 3.9 (1.92/6.31)/6.33 (4.79/9.09)/2.84 (0.29/5.17) | 3.55 (1.41/4.52)/6 (2.47/11.2)/3.11 (1.06/6.68) | 0.606 k/0.291 k/0.564 k |
| p value (preop vs. postop) | <0.001 ɯ | <0.001 ɯ | 0.003 ɯ | |
| C4-C5 disc height (mm), mean (SD) | 3.56 (1.22)/6.64 (1.24)/3.08 (1.86) | 3.31 (1.36)/6.68 (1.27)/3.37 (1.42) | 3.66 (0.79)/7.52 (1.49)/3.86 (1.27) | 0.718 f/0.215 f/0.490 R |
| p value (preop vs. postop) | <0.001 t | 0.001 t | 0.001 t | |
| C5-C6 disc height (mm), median (min/max) | 3.33 (1.25/6.63)/7.55 (5.3/9.95)/3.97 (−0.43/7.21) | 2.63 (0.96/5.69) A/7.93 (4.58/16)/4.98 (1.85/13.29) | 3.03 (1.19/4.52)/8.21 (4.49/8.94)/5.18 (2.26/6.78) | 0.008 k/0.581 k/0.159 k |
| p value (preop vs. postop) | <0.001 ɯ | <0.001 ɯ | 0.003 ɯ | |
| C6-C7 disc height (mm), mean (SD) | 4.14 (1.44)/7.73 (1.69)/3.59 (1.94) | 3.13 (1.3)/8.6 (2.07)/5.47 (2.33) A | 3.48 (1.44)/7.47 (2.12)/3.99 (1.88) | 0.086 f/0.248 f/0.024 R |
| p value (preop vs. postop) | <0.001 t | <0.001 t | <0.001 t | |
| C0-C2 angle, mean (SD) | 22.43 (9.24)/20.18 (8.54)/−2.26 (9.64) | 16.86 (7.19)/19.57 (7.39)/2.71 (11.19) | 19.87 (10.89)/24.32 (7.79)/4.46 (11.88) | 0.158 f/0.316 f/0.226 R |
| p value (preop vs. postop) | 0.355 t | 0.292 t | 0.293 t | |
| C1-C2 angle, mean (SD) | 22.35 (10.64)/28.69 (6.39)/6.34 (9.26) | 29.58 (6.51)/31.67 (3.89)/2.09 (6.82) | 27.78 (8.8)/31.04 (6.44)/3.27 (4.66) | 0.043 f/0.237 f/0.226 R |
| p value (preop vs. postop) | 0.010 t | 0.186 t | 0.069 t | |
| C1-C7 angle, mean (SD) | 31.14 (17.43)/39.69 (13.18)/8.55 (13.71) | 35.05 (11.11)/42.27 (10.06)/7.22 (8.53) | 32.87 (11.31)/42.4 (12.75)/9.53 (8.54) | 0.690 f/0.764 f/0.853 R |
| p value (preop vs. postop) | 0.017 t | 0.001 t | 0.010 t | |
| C7 slope, mean (SD) | 22.28 (10.79)/29.04 (8.17)/6.76 (6.94) | 16.61 (7.26)/23.19 (8)/6.58 (8.94) | 17.58 (5.87)/24.69 (10.15)/7.11 (7.43) | 0.123 f/0.109 f/0.986 R |
| p value (preop vs. postop) | 0.001 t | 0.004 t | 0.021 t | |
| t1 slope, mean (SD.) | 26.62 (11.33)/31.03 (9.47)/4.41 (9.15) | 19.74 (7.59) A/24.13 (6.46) A/4.39 (7.07) | 19.66 (5.4)/24.26 (9)/4.6 (7.12) | 0.045 f/0.028 f/0.998 R |
| p value (preop vs. postop) | 0.057 t | 0.012 t | 0.089 t | |
| C2-C7 sva, median (min/max) | 1.92 (0.56/4.08)/3.09 (0.85/6.94)/1.41 (−0.24/3.89) | 1.53 (0.68/8.97)/2.66 (0.69/5.12)/1.01 (−6.3/4.29) | 1.45 (1.04/2.99)/2.48 (0.64/5.3)/0.84 (−0.52/3.77) | 0.800 k/0.384 k/0.620 k |
| p value (preop vs. postop) | <0.001 ɯ | 0.015 ɯ | 0.018 ɯ | |
| C2-C7 Harrison tangle method, mean (SD) | 10.56 (8.23)/12.54 (7.71)/1.98 (6.64) | 8.55 (5.05)/11.21 (7.53)/2.66 (7.82) | 7.7 (5.76)/11.88 (5.4)/4.18 (5.24) | 0.493 f/0.852 f/0.743 R |
| p value (preop vs. postop) | 0.222 t | 0.145 t | 0.044 t | |
| Independent Variable | B (SE) | p Value | Odds Ratio (95% C.I.) |
|---|---|---|---|
| Single–Triple R | |||
| Preop C5-C6 disc height (mm) | 0.27 (0.54) | 0.612 | 1.31 [0.46–3.76] |
| Postop t1 slope | 0.1 (0.08) | 0.223 | 1.1 [0.94–1.28] |
| C6-C7 disc height change | 0.33 (0.36) | 0.358 | 1.39 [0.69–2.82] |
| Preop t1 slope | 0.09 (0.07) | 0.238 | 1.09 [0.94–1.26] |
| JOA recovery rate (%) | 0.2 (0.08) | 0.017 | 1.22 [1.04–1.43] |
| Intercept (↓) | 21.91 (8.99) | 0.015 | - |
| Double–Triple R | |||
| Preop C5-C6 disc height (mm) | 0.37 (0.5) | 0.464 | 1.45 [0.54–3.87] |
| Postop t1 slope | 0.02 (0.07) | 0.807 | 1.02 [0.89–1.17] |
| C6-C7 disc height change | 0.34 (0.29) | 0.239 | 1.41 [0.8–2.5] |
| Preop t1 slope | 0.02 (0.06) | 0.727 | 1.02 [0.9–1.16] |
| JOA recovery rate (%) | 0.01 (0.04) | 0.772 | 1.01 [0.93–1.11] |
| Intercept | 0.96 (3.77) | 0.799 | - |
| Double–Single R | |||
| Preop C5-C6 disc height (mm) | 0.64 (0.49) | 0.192 | 1.9 [0.72–4.97] |
| Postop t1 slope | 0.08 (0.07) | 0.275 | 1.08 [0.94–1.24] |
| C6-C7 disc height change | 0.68 (0.3) | 0.025 | 1.96 [1.09–3.54] |
| Preop t1 slope | 0.11 (0.07) | 0.107 | 1.12 [0.98–1.27] |
| JOA recovery rate (%) | 0.18 (0.08) | 0.022 | 1.2 [1.03–1.4] |
| Intercept (↑) | 20.95 (8.79) | 0.017 | - |
| Single: 83.3, Double: 80.0, Triple: 22.2, Overall: 70.2 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gökoğlu, A.; Yiğit, H.; Doğan, K.; Nisari, M.; Unur, E. The Impact of Multilevel Anterior Cervical Discectomy and Fusion on Cervical Sagittal Alignment: A Comparative Study of Single-, Two-, and Three-Level Procedures. J. Clin. Med. 2025, 14, 3413. https://doi.org/10.3390/jcm14103413
Gökoğlu A, Yiğit H, Doğan K, Nisari M, Unur E. The Impact of Multilevel Anterior Cervical Discectomy and Fusion on Cervical Sagittal Alignment: A Comparative Study of Single-, Two-, and Three-Level Procedures. Journal of Clinical Medicine. 2025; 14(10):3413. https://doi.org/10.3390/jcm14103413
Chicago/Turabian StyleGökoğlu, Abdulkerim, Hüseyin Yiğit, Kadirhan Doğan, Mehtap Nisari, and Erdoğan Unur. 2025. "The Impact of Multilevel Anterior Cervical Discectomy and Fusion on Cervical Sagittal Alignment: A Comparative Study of Single-, Two-, and Three-Level Procedures" Journal of Clinical Medicine 14, no. 10: 3413. https://doi.org/10.3390/jcm14103413
APA StyleGökoğlu, A., Yiğit, H., Doğan, K., Nisari, M., & Unur, E. (2025). The Impact of Multilevel Anterior Cervical Discectomy and Fusion on Cervical Sagittal Alignment: A Comparative Study of Single-, Two-, and Three-Level Procedures. Journal of Clinical Medicine, 14(10), 3413. https://doi.org/10.3390/jcm14103413






