The Implementation of Trifecta Score to Assess the Quality of Holmium Laser Enucleation of the Prostate in Elderly Patients: An Analysis of Perioperative and Functional Outcomes and the Impact of Age
Abstract
1. Introduction
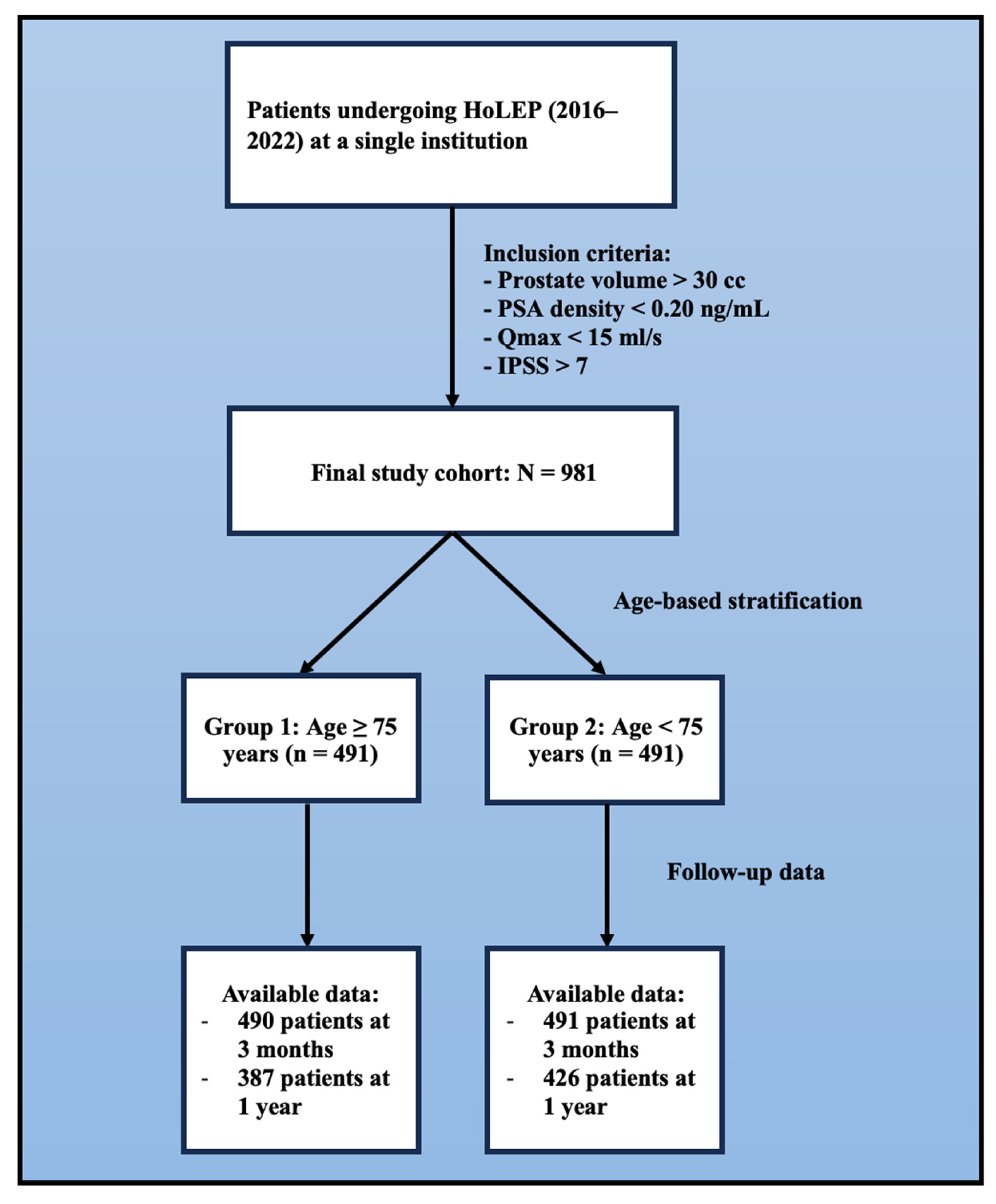
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical Technique
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BPH | Benign Prostatic Hyperplasia |
| LUTS | Lower Urinary Tract Symptoms |
| EAU | European Association of Urology |
| TURP | Transurethral Resection of the Prostate |
| OP | Open Prostatectomy |
| OT | Operative Time |
| HoLEP | Holmium Laser Enucleation of the Prostate |
| ASA | American Society of Anesthesiologists |
| Qmax | Maximum Urinary Flow Rate |
| IPSS | International Prostate Symptom Score |
| ET | Enucleation Time |
| LOS | Length of Hospital Stay |
| CD | Clavien–Dindo |
| PSA | Prostate-Specific Antigen |
| CCI | Charlson Comorbidity Index |
| UI | Urinary Incontinence |
| OR | Odds Ratio |
| CI | Confidence Interval |
| UTI | Urinary Tract Infection |
References
- D’Agate, S.; Wilson, T.; Adalig, B.; Manyak, M.; Palacios-Moreno, J.M.; Chavan, C.; Oelke, M.; Roehrborn, C.; Della Pasqua, O. Impact of disease progression on individual IPSS trajectories and consequences of immediate versus delayed start of treatment in patients with moderate or severe LUTS associated with BPH. World J. Urol. 2020, 38, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Bartoletti, R.; Cai, T.; Tinacci, G.; Longo, I.; Ricci, A.; Massaro, M.P.; Tosoratti, N.; Zini, E.; Pinzi, N. Transperineal microwave thermoablation in patients with obstructive benign prostatic hyperplasia: A phase I clinical study with a new mini-choked microwave applicator. J. Endourol. 2008, 22, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Madersbacher, S.; Sampson, N.; Culig, Z. Pathophysiology of Benign Prostatic Hyperplasia and Benign Prostatic Enlargement: A Mini-Review. Gerontology 2019, 65, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, T.; Girman, C.J.; Jacobsen, S.J.; Roberts, R.O.; Guess, H.A.; Lieber, M.M. Longitudinal prostate growth rates during 5 years in randomly selected community men 40–79 years old. J. Urol. 1999, 161, 1174–1179. [Google Scholar] [CrossRef]
- Cornu, J.N.; Gacci, M.; Hashim, H.; Herrmann, T.R.W.; Malde, S.; Netsch, C.; De Nunzio, C.; Rieken, M.; Sakalis, V.; Tutolo, M. EAU Guidelines on Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS); Edn. Presented at the EAU Annual Congress Paris April 2024; European Association of Urology: Arnhem, The Netherlands, 2024; ISBN 978-94-92671-23-3. [Google Scholar]
- Scarcella, S.; Castellani, D.; Gauhar, V.; Teoh, J.Y.-C.; Giulioni, C.; Piazza, P.; Bravi, C.A.; De Groote, R.; De Naeyer, G.; Puliatti, S.; et al. Robotic-assisted versus open simple prostatectomy: Results from a systematic review and meta-analysis of comparative studies. Investig. Clin. Urol. 2021, 62, 631–640. [Google Scholar] [CrossRef]
- Tallè, M.; Giulioni, C.; Papaveri, A.; Mengoni, F.; Orciani, R.; Pandolfo, S.D.; Imbimbo, C.; Crocetto, F.; Castellani, D.; Herrmann, T.; et al. Influence of preoperative indwelling urinary catheter on outcomes of high-power holmium laser enucleation for very large prostate (≥200 mL). World J. Urol. 2025, 43, 223. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.; Esser, J.; Suarez-Ibarrola, R.; Gratzke, C.; Miernik, A. Safety and Efficacy of Laser Enucleation of the Prostate in Elderly Patients—A Narrative Review. Clin. Interv. Aging 2022, 17, 15–33. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Autorino, R.; Zargar, H.; Mariano, M.B.; Sanchez-Salas, R.; Sotelo, R.J.; Chlosta, P.L.; Castillo, O.; Matei, D.V.; Celia, A.; Koc, G.; et al. Perioperative Outcomes of Robotic and Laparoscopic Simple Prostatectomy: A European-American Multi-institutional Analysis. Eur. Urol. 2015, 68, 86–94. [Google Scholar] [CrossRef]
- World Health Organization. Significant loss of functional ability, and care dependence. World Rep. Aging Heal. 2015. Available online: http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=2342855AC115632C5C15C1B21BAC57F9?sequence=1 (accessed on 24 May 2023).
- Gilling, P.J.; Kennett, K.; Das, A.K.; Thompson, D.; Fraundorfer, M.R. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: An update on the early clinical experience. J. Endourol. 1998, 12, 457–459. [Google Scholar] [CrossRef]
- Mantica, G.; Ambrosini, F.; Drocchi, G.; Zubko, Z.; Monaco, L.L.; Cafarelli, A.; Calarco, A.; Colombo, R.; De Cobelli, O.; De Marco, F.; et al. Non-surgical management of BPH: An updated review of current literature and state of the art on natural compounds and medical therapy. Arch. Ital. Urol. Androl. 2024, 96, 13098. [Google Scholar] [CrossRef]
- Palumbo, S.; Lucarelli, G.; Lasorsa, F.; Damiano, R.; Autorino, R.; Aveta, A.; Spena, G.; Perdonà, S.; Russo, P.; Giulioni, C.; et al. Urobiome and Inflammation: A Systematic Review on Microbial Imbalances and Diagnostic Tools for Urinary Disorders. Urology 2025, in press. [CrossRef] [PubMed]
- O’Sullivan, E.D.; Hughes, J.; Ferenbach, D.A. Renal Aging: Causes and Consequences. J. Am. Soc. Nephrol. 2017, 28, 407–420. [Google Scholar] [CrossRef] [PubMed]
- Giulioni, C.; Palantrani, V.; De Stefano, V.; Cicconofri, A.; Antezza, A.; Beltrami, M.; Milanese, G.; Ranghino, A.; Gauhar, V.; Castellani, D.; et al. Current Evidence on Surgical Management for Benign Prostatic Hyperplasia in Renal Transplant Recipients: A Systematic Review. J. Endourol. 2023, 37, 1129–1138. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, B.; Li, B.; Yang, S.; Wang, Z.; Han, C.; Wu, J.; Tian, R. Correlation Between Benign Prostatic Hyperplasia/Lower Urinary Tract Symptoms and Renal Function in Elderly Men Aged 80 Years and Older. Clin. Interv. Aging 2023, 18, 61–69. [Google Scholar] [CrossRef]
- Brandt, T.W.; Luizzi, J.M.; Caras, R.J. Evaluation of Current Surgical BPH Interventions for Young and Elderly Men. Curr. Urol. Rep. 2024, 25, 79–91. [Google Scholar] [CrossRef]
- Burtt, G.; Springate, C.; Martin, A.; Woodward, E.; Zantek, P.; Al Jaafari, F.; Muir, G.; Misrai, V. The Efficacy and Safety of Laser and Electrosurgical Transurethral Procedures for the Treatment of BPO in High-Risk Patients: A Systematic Review. Res. Rep. Urol. 2022, 14, 247–257. [Google Scholar] [CrossRef]
- Romero-Otero, J.; García-González, L.; García-Gómez, B.; Justo-Quintas, J.; García-Rojo, E.; González-Padilla, D.A.; Sopeña-Sutil, R.; Duarte-Ojeda, J.M.; Rodríguez-Antolín, A. Factors Influencing Intraoperative Blood Loss in Patients Undergoing Holmium Laser Enucleation of the Prostate (HoLEP) for Benign Prostatic Hyperplasia: A Large Multicenter Analysis. Urology 2019, 132, 177–182. [Google Scholar] [CrossRef]
- Harrison, S.L.; Buckley, B.J.R.; Ritchie, L.A.; Proietti, R.; Underhill, P.; Lane, D.A.; Lip, G.Y.H. Oral anticoagulants and outcomes in adults ≥80 years with atrial fibrillation: A global federated health network analysis. J. Am. Geriatr. Soc. 2022, 70, 2386–2392. [Google Scholar] [CrossRef]
- Daryanto, B.; Suryanullah, W.S.; Putra, P.Y.P. Holmium laser enucleation of the prostate versus transurethral resection of the prostate in treatment of benign prostatic hyperplasia: A meta-analysis of 13 randomized control trials. Curr. Urol. 2025, 19, 6–16. [Google Scholar] [CrossRef]
- Agarwal, S.; Busse, P.J. Innate and adaptive immunosenescence. Ann. Allergy Asthma Immunol. 2010, 104, 183–210. [Google Scholar] [CrossRef]
- Olagundoye, O.; Ross, S.; Gibson, W.; Wagg, A. Defining and prioritizing modifiable risk factors towards the co-creation of a urinary incontinence self-management intervention for older men: A sequential multimethod study protocol. PLoS ONE 2024, 19, e0305052. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gauhar, V.; Sancha, F.G.; Enikeev, D.; Sofer, M.; Fong, K.Y.; Socarrás, M.R.; Elterman, D.; Chiruvella, M.; Bendigeri, M.T.; Tursunkulov, A.N.; et al. Results from a global multicenter registry of 6193 patients to refine endoscopic anatomical enucleation of the prostate (REAP) by evaluating trends and outcomes and nuances of prostate enucleation in a real-world setting. World J. Urol. 2023, 41, 3033–3040. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Zhang, J.; Zhu, H.; Huang, F.; Shadike, A.; Jiang, C. Predictive factors of stress urinary incontinence after Holmium Laser Enucleation of the Prostate: A magnetic resonance imaging-based retrospective study. Transl. Androl. Urol. 2024, 13, 1775–1785. [Google Scholar] [CrossRef] [PubMed]
- Savin, Z.; Veredgorn, Y.; Taha, T.; Alsaraia, N.; Lifshitz, K.; Nevo, A.; Yossepowitch, O.; Sofer, M. En bloc holmium laser enucleation of prostate in octogenarians and nonagenarians: Clinical characteristics and outcome. Lasers Med. Sci. 2023, 38, 196. [Google Scholar] [CrossRef]
- Mmeje, C.O.; Nunez-Nateras, R.; Warner, J.N.; Humphreys, M.R. Age-stratified outcomes of holmium laser enucleation of the prostate. BJU Int. 2013, 112, 982–989. [Google Scholar] [CrossRef]
- Piao, S.; Choo, M.S.; Kim, M.; Jeon, H.J.; Oh, S.J. Holmium Laser Enucleation of the Prostate is Safe for Patients Above 80 Years: A Prospective Study. Int. Neurourol. J. 2016, 20, 143–150. [Google Scholar] [CrossRef]
- Grosso, A.A.; Di Maida, F.; Nardoni, S.; Salvi, M.; Giudici, S.; Lambertini, L.; Cadenar, A.; Tellini, R.; Cocci, A.; Mari, A.; et al. Patterns and Predictors of Optimal Surgical and Functional Outcomes after Holmium Laser Enucleation of the Prostate (HoLEP): Introducing the Concept of “Trifecta”. World J. Mens. Health. 2023, 41, 603–611. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Miano, R.; Di Lorenzo, N.; Spera, E.; Vespasiani, G.; Mugnier, C. Laparoscopic versus robot-assisted bilateral nerve-sparing radical prostatectomy: Comparison of pentafecta rates for a single surgeon. Surg. Endosc. 2013, 27, 4297–4304. [Google Scholar] [CrossRef]
| Variable | Group 1 Age ≥ 75 Years n = 490 | Group 2 Age < 75 Years n = 491 | p Value |
|---|---|---|---|
| Age, years | 78.9 (3.7) | 65.1 (6.15) | <0.001 |
| Body Mass Index, kg/m2 | 26.0 (2.6) | 25.3 (2.7) | 0.008 |
| ASA Score, n (%) | |||
| 1 | 56 (11.4) | 148 (30.1) | <0.001 |
| 2 | 272 (55.5) | 297 (60.5) | 0.11 |
| 3 | 162 (33.1) | 46 (9.4) | <0.001 |
| Charlson Comorbidity Index | 4.43 (0.94) | 1.75 (0.49) | <0.001 |
| Surgery with ongoing anticoagulant/antiplatelet, n (%) | 0.004 | ||
| Yes | 117 (23.8) | 81 (16.4) | |
| No | 373 (76.2) | 410 (83.6) | |
| Prostate volume, mL | 73.6 (38.9) | 74.0 (37.4) | 0.92 |
| Preoperative PSA, ng/mL | 2.43 (2.17) | 2.85 (2.26) | 0.39 |
| Preoperative IUC, n (%) | 0.66 | ||
| Yes | 42 (8.6) | 46 (9.3) | |
| No | 448 (91.4) | 445 (90.7) | |
| Preoperative IPSS | 20.4 (5.7) | 17.9 (2.4) | 0.41 |
| Preoperative Q max, mL/s | 9.1(2.7) | 8.7 (2.9) | 0.57 |
| Preoperative PVR, mL | 74.7 (55.2) | 67.8 (52.1) | 0.01 |
| Variable | Group 1 Age ≥ 75 Years n = 490 | Group 2 Age < 75 Years n = 491 | p Value |
|---|---|---|---|
| Operative time, minutes | 57.3 (27.5) | 54.6 (24.2) | 0.26 |
| Enucleation type, n (%) | 0.26 | ||
| 3 lobes | 268 (54.6) | 286 (58.3) | |
| 2 lobes | 222 (45.4) | 205 (41.7) | |
| Electrocautery after enucleation, n (%) | 31 (6.3) | 109 (5.6) | 0.54 |
| Enucleation time, minutes | 44.0 (21.4) | 43.2 (12.6) | 0.71 |
| Adenoma requiring monopolar resection, n (%) | 0.63 | ||
| Yes | 22 (4.5) | 19 (3.8) | |
| No | 468 (95.5) | 472 (96.2) | |
| Length of hospital stay, days | 2.03 (0.23) | 2.01 (0.13) | 0.09 |
| Time to urethral catheter removal, days | 2.23 (1.20) | 2.07 (0.73) | 0.02 |
| Histologic findings, n (%) | 0.04 | ||
| Incidental prostate cancer | 27 (5.5) | 14 (2.8) | |
| Benign prostatic tissue | 463 (94.5) | 477 (97.2) | |
| No perioperative complications, n (%) | 424 (86.5) | 444 (90.4) | 0.06 |
| 3MPO IPSS * | 7.6 (4.8) | 7.0 (4.5) | 0.04 |
| 3MPO IPSS < 8, n (%) | 346 (70.6) | 369 (75.1) | 0.11 |
| 3MPO Q max *, mL/s | 23.6 (5.8) | 27.9 (7.2) | <0.001 |
| 3MPO Q max > 15 mL/s, n (%) | 448 (91.4) | 463 (94.3) | 0.08 |
| 3MPO PVR *, mL | 16.2 (12.3) | 14.9 (13.6) | 0.05 |
| 1YPO IPSS ∆ | 5.2 (3.9) | 4.8 (4.2) | 0.06 |
| 1YPO Q max ∆, mL/s | 22.9 (4.4) | 26.8 (5.1) | 0.16 |
| 1YPO PVR ∆, mL | 14.7 (10.5 | 14.1 (9.6) | 0.23 |
| Trifecta Score Achievement, n (%) | 311 (63.5) | 338 (68.8) | 0.08 |
| Variable | Group 1 Age ≥ 75 Years n = 490 | Group 2 Age < 75 Years n = 491 | p Value |
|---|---|---|---|
| Early complications, n (%) | |||
| Urinary tract infection (CD 2) | 17 (3.5) | 14 (2.9) | 0.58 |
| Acute urinary retention within 24 h (CD 2) | 21 (4.3) | 16 (3.3) | 0.40 |
| Blood transfusion (CD2) | 23 (4.7) | 11 (2.2) | 0.04 |
| Postoperative bleeding needing endoscopic hemostasis (CD 3) | 6 (1.2) | 3 (0.6) | 0.31 |
| Sepsis needing ICU (CD 4) | 2 (0.4) | 2 (0.4) | 0.99 |
| Late complications, n (%) | |||
| Bulbar urethral stricture requiring outpatient dilatation | 17 (3.5) | 11 (2.3) | 0.25 |
| Urethral stricture necessitating urethrotomy under anesthesia | 11 (2.2) | 13 (2.6) | 0.68 |
| Bladder neck sclerosis requiring transurethral Incision | 23 (4.7) | 14 (2.8) | 0.13 |
| Repeated surgery for BPH within 1 year | 5 (1.1) | 4 (0.8) | 0.74 |
| 1-Month postoperative urinary incontinence | 72 (14.7) | 66 (13.4) | 0.57 |
| Urge | 21 (4.3) | 16 (3.3) | 0.40 |
| Stress | 48 (8.3) | 37 (7.5) | 0.21 |
| Mixed | 10 (2.1) | 13 (2.6) | 0.53 |
| Kegel exercise needed, n (%) | 68 (13.8) | 45 (9.2) | 0.02 |
| 1-Year postoperative urinary incontinence | 36 (7.3) | 31 (6.2) | 0.52 |
| Urge | 2 (0.4) | 3 (0.6) | 0.66 |
| Stress | 31 (6.3) | 23 (4.6) | 0.26 |
| Mixed | 3 (0.6) | 5 (1.0) | 0.74 |
| Parameters | Odds Ratio (95% Confidence Interval) | p Values |
|---|---|---|
| Perioperative complications | 1.23 (0.78–2.96) | 0.74 |
| 3-month postoperative Qmax (>15 mL/s) | 0.76 (0.47–1.52) | 0.51 |
| 3-month postoperative IPSS (<8) | 1.03 (0.58–1.74) | 0.83 |
| Parameters | Urinary Incontinence After 1 Year OR (95% CI) | p Values |
|---|---|---|
| Age | 0.98 (0.95–1.04) | 0.55 |
| Prostate Volume | 0.95 (0.92–1.08) | 0.36 |
| Preoperative Qmax | 0.91 (0.81–0.94) | 0.38 |
| Preoperative IPSS | 1.06 (1.01–1.13) | 0.92 |
| Preoperative PVR | 0.88 (0.81–0.95) | 0.07 |
| Operative time | 1.05 (1.02–1.09) | 0.02 |
| Length of Stay | 0.91 (0.53–1.86) | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giulioni, C.; Tallè, M.; Papaveri, A.; Mengoni, F.; Orciani, R.; Pandolfo, S.D.; Imbimbo, C.; Crocetto, F.; Maurizi, V.; Gauhar, V.; et al. The Implementation of Trifecta Score to Assess the Quality of Holmium Laser Enucleation of the Prostate in Elderly Patients: An Analysis of Perioperative and Functional Outcomes and the Impact of Age. J. Clin. Med. 2025, 14, 3410. https://doi.org/10.3390/jcm14103410
Giulioni C, Tallè M, Papaveri A, Mengoni F, Orciani R, Pandolfo SD, Imbimbo C, Crocetto F, Maurizi V, Gauhar V, et al. The Implementation of Trifecta Score to Assess the Quality of Holmium Laser Enucleation of the Prostate in Elderly Patients: An Analysis of Perioperative and Functional Outcomes and the Impact of Age. Journal of Clinical Medicine. 2025; 14(10):3410. https://doi.org/10.3390/jcm14103410
Chicago/Turabian StyleGiulioni, Carlo, Matteo Tallè, Alessio Papaveri, Francesco Mengoni, Roberto Orciani, Savio Domenico Pandolfo, Ciro Imbimbo, Felice Crocetto, Valentina Maurizi, Vineet Gauhar, and et al. 2025. "The Implementation of Trifecta Score to Assess the Quality of Holmium Laser Enucleation of the Prostate in Elderly Patients: An Analysis of Perioperative and Functional Outcomes and the Impact of Age" Journal of Clinical Medicine 14, no. 10: 3410. https://doi.org/10.3390/jcm14103410
APA StyleGiulioni, C., Tallè, M., Papaveri, A., Mengoni, F., Orciani, R., Pandolfo, S. D., Imbimbo, C., Crocetto, F., Maurizi, V., Gauhar, V., & Cafarelli, A. (2025). The Implementation of Trifecta Score to Assess the Quality of Holmium Laser Enucleation of the Prostate in Elderly Patients: An Analysis of Perioperative and Functional Outcomes and the Impact of Age. Journal of Clinical Medicine, 14(10), 3410. https://doi.org/10.3390/jcm14103410








