Self-Adapting Foot Orthosis Inlay Facilitates Handling and Reduces Plantar Pressure Compared to Vacuum-Based Technology
Abstract
1. Introduction
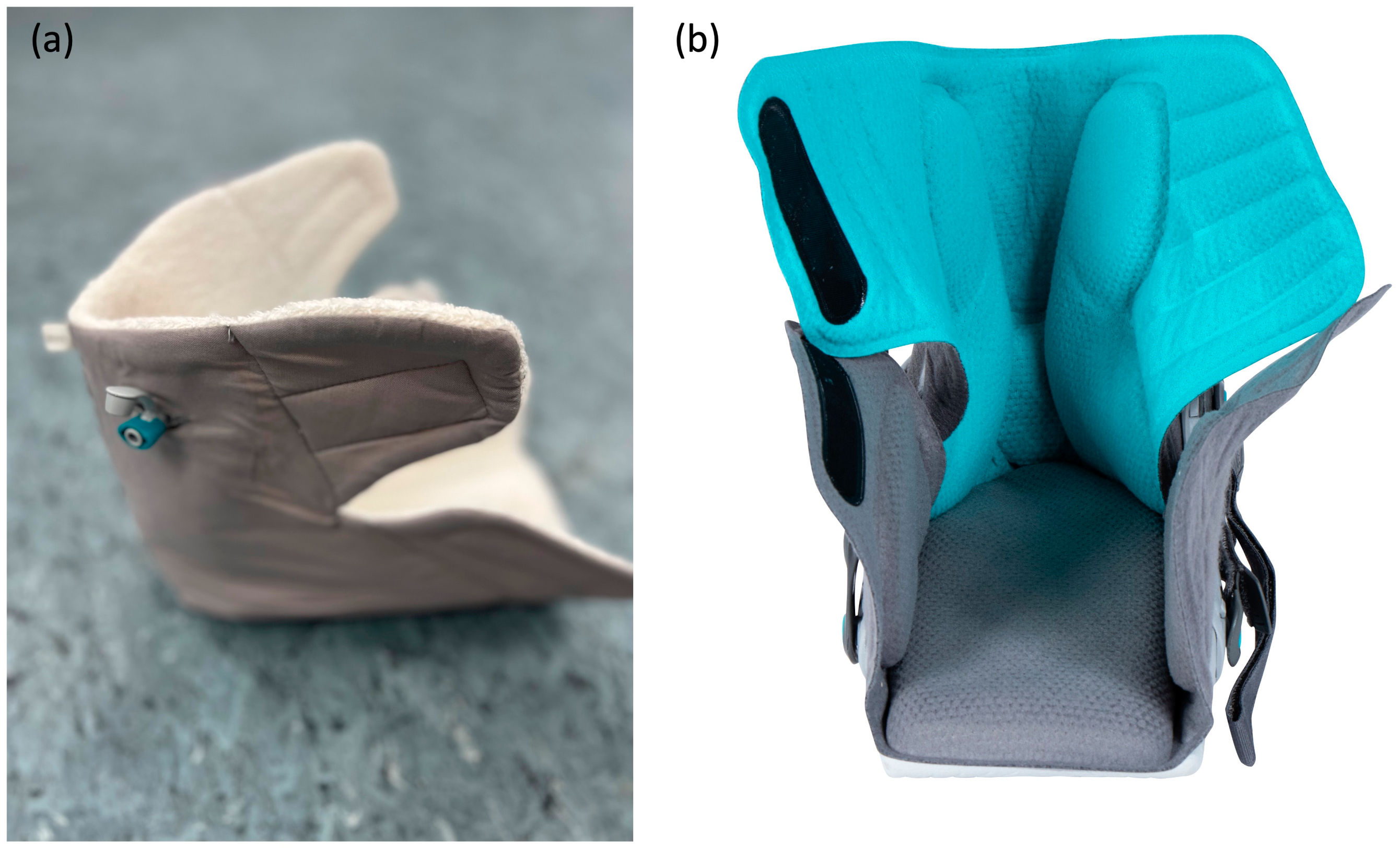
2. Materials and Methods
2.1. Subjects
2.2. Study Design
2.3. Statistics
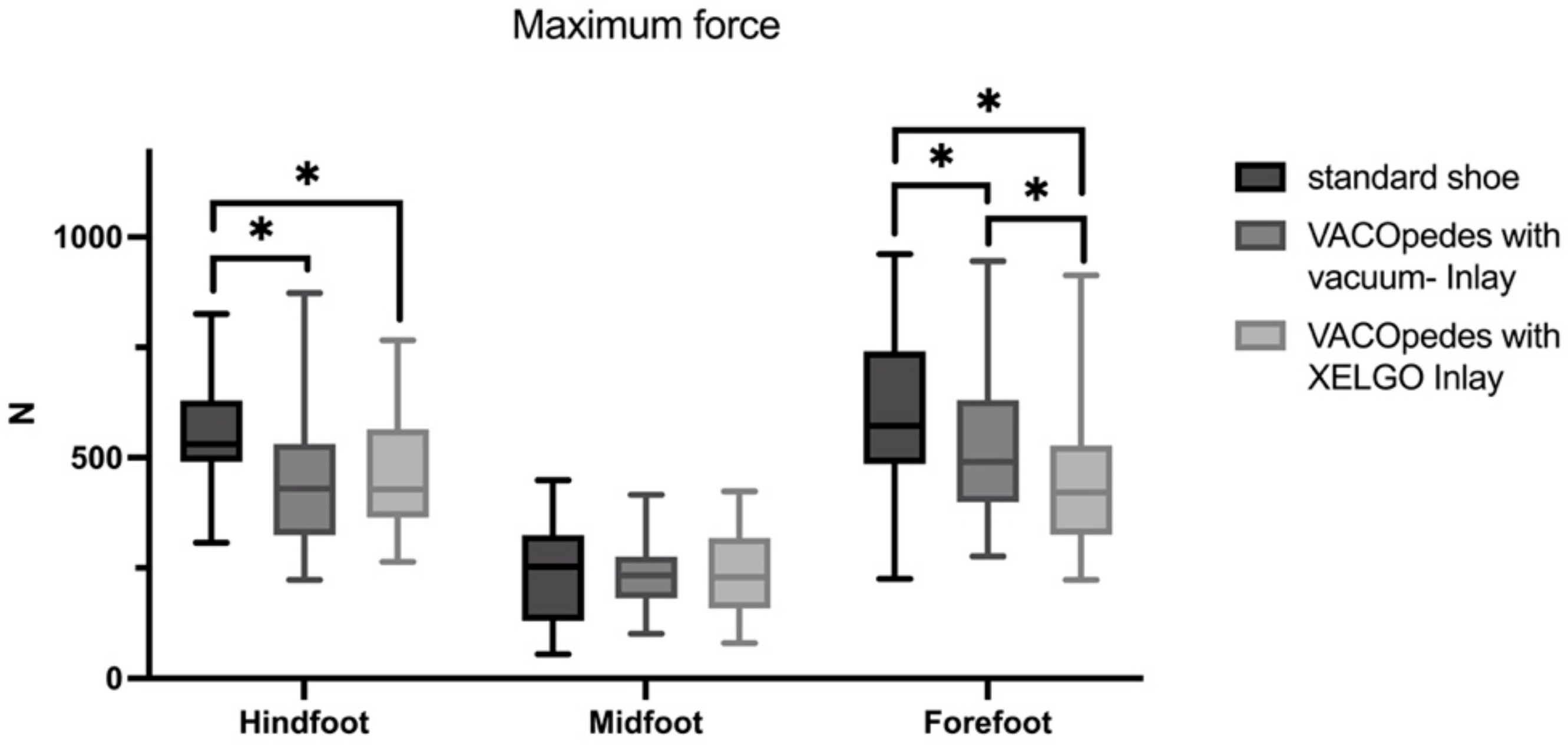
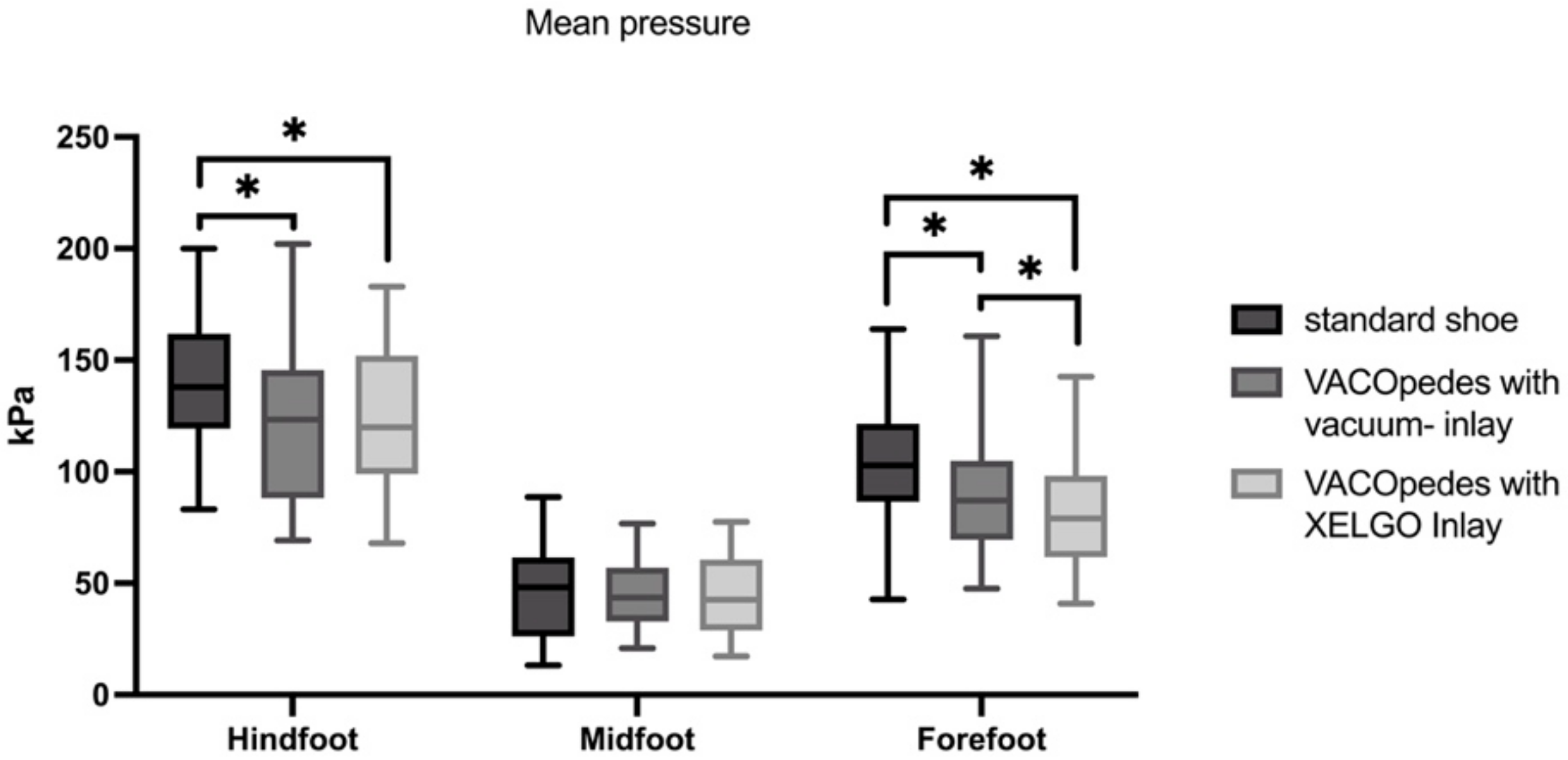
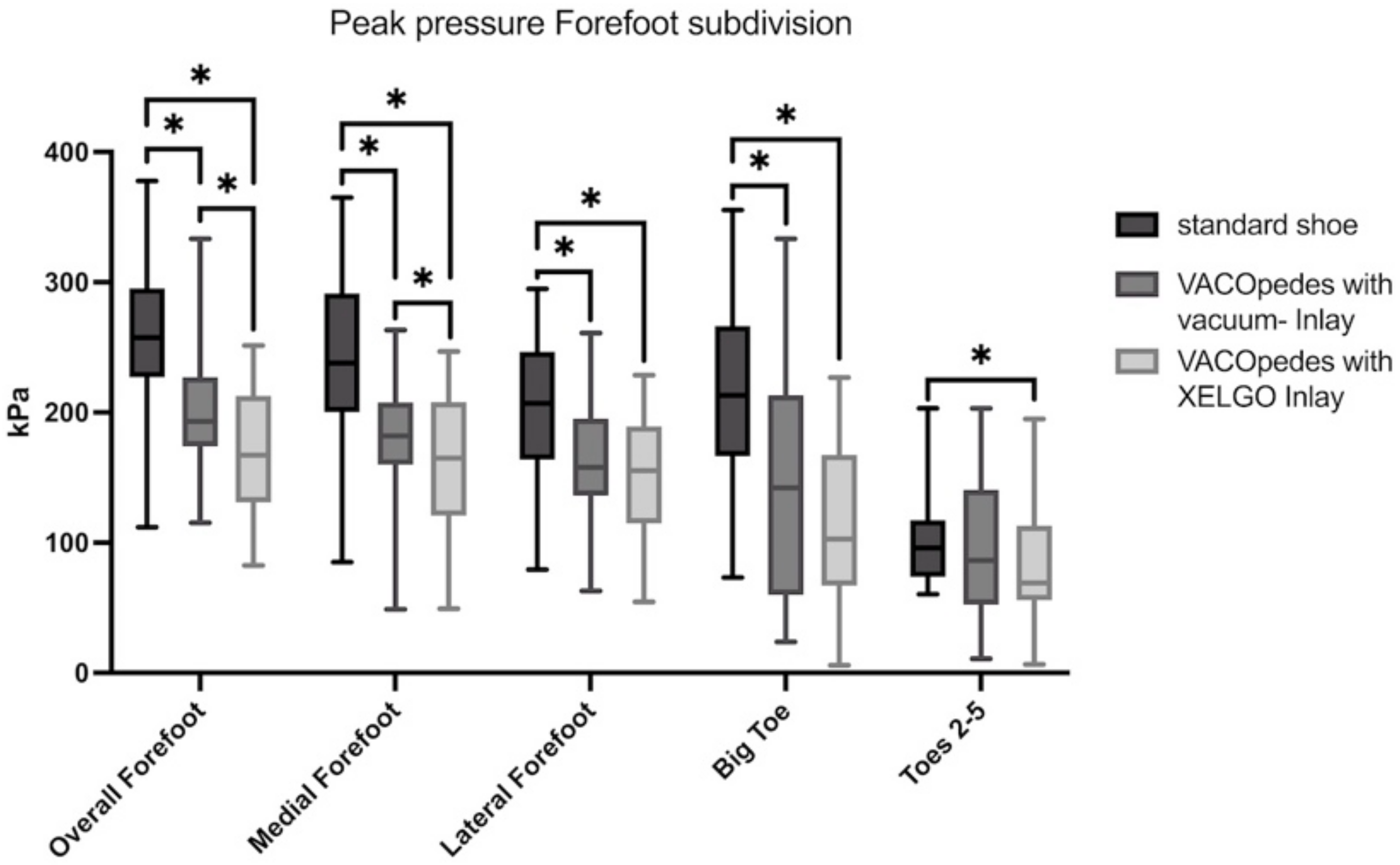
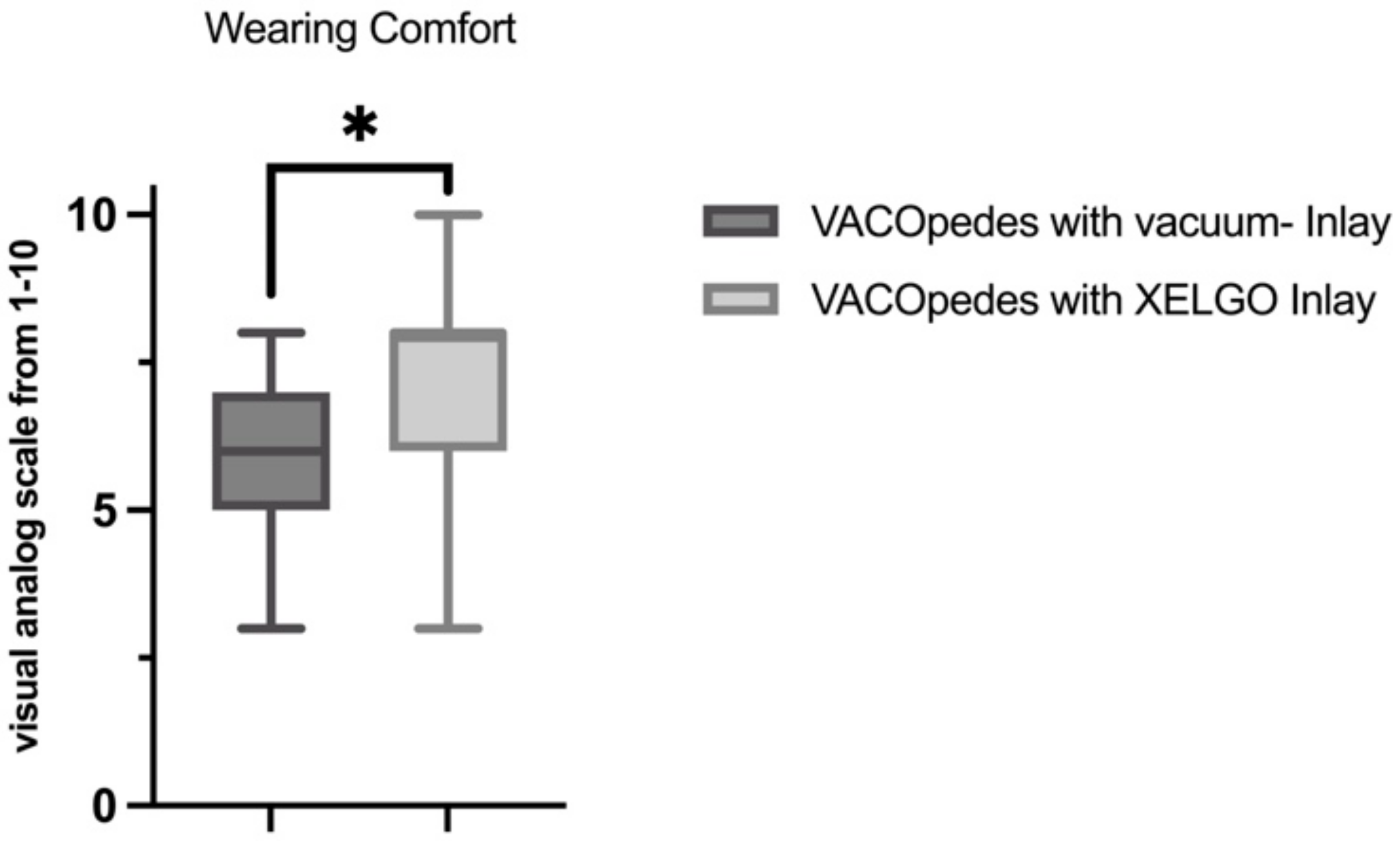
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| kPa | kiloPascal |
| N | Newton |
| OTS | Off-the-shelf shoe |
References
- Stöckle, U.; König, B.; Tempka, A.; Südkamp, N.P. Gipsruhigstellung versus Vakuumstützsystem Frühfunktionelle Ergebnisse Nach Osteosynthese von Sprunggelenksfrakturen. Unfallchirurg 2000, 103, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Deleu, P.-A.; Leemrijse, T.; Vandeleene, B.; Maldague, P.; Bevernage, B.D. Plantar Pressure Relief Using a Forefoot Offloading Shoe. Foot Ankle Surg. 2010, 16, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Carl, H.-D.; Pfander, D.; Swoboda, B. Assessment of Plantar Pressure in Forefoot Relief Shoes of Different Designs. Foot Ankle Int. 2006, 27, 117–120. [Google Scholar] [CrossRef]
- Bosch, K.; Nagel, A.; Weigend, L.; Rosenbaum, D. From “First” to “Last” Steps in Life—Pressure Patterns of Three Generations. Clin. Biomech. 2009, 24, 676–681. [Google Scholar] [CrossRef]
- Queen, R.M.; Vap, A.; Moorman, C.T.; Garrett, W.E.; Butler, R.J. Gender Differences in Plantar Loading During an Unanticipated Side Cut on FieldTurf. Clin. J. Sport. Med. 2016, 26, 157–161. [Google Scholar] [CrossRef]
- Kirmizi, M.; Sengul, Y.S.; Angin, S. The Effects of Gait Speed on Plantar Pressure Variables in Individuals with Normal Foot Posture and Flatfoot. Acta Bioeng. Biomech. 2020, 22, 161–168. [Google Scholar] [CrossRef]
- Catan, L.; Amaricai, E.; Onofrei, R.R.; Popoiu, C.M.; Iacob, E.R.; Stanciulescu, C.M.; Cerbu, S.; Horhat, D.I.; Suciu, O. The Impact of Overweight and Obesity on Plantar Pressure in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6600. [Google Scholar] [CrossRef]
- Stacoff, A.; Quervain, I.K.; Dettwyler, M.; Wolf, P.; List, R.; Ukelo, T.; Stüssi, E. Biomechanical Effects of Foot Orthoses during Walking. Foot 2007, 17, 143–153. [Google Scholar] [CrossRef]
- Hähni, M.; Hirschmüller, A.; Baur, H. The Effect of Foot Orthoses with Forefoot Cushioning or Metatarsal Pad on Forefoot Peak Plantar Pressure in Running. J. Foot Ankle Res. 2016, 9, 44. [Google Scholar] [CrossRef]
- Kraus, T.M.; Graf, F.; Mitternacht, J.; Döbele, S.; Stöckle, U.; Siebenlist, S. Abrollende Vakuumstützorthese versus Vorfußentlastungsschuh Zur Behandlung von Metatarsalefrakturen. MMW-Fortschritte Med. 2014, 156, 11–17. [Google Scholar] [CrossRef]
- Sint, A.; Baumbach, S.F.; Böcker, W.; Kammerlander, C.; Kanz, K.-G.; Braunstein, M.; Polzer, H. Influence of Age and Level of Activity on the Applicability of a Walker Orthosis—A Prospective Study in Different Cohorts of Healthy Volunteers. BMC Musculoskelet. Disord. 2018, 19, 453. [Google Scholar] [CrossRef] [PubMed]
- Putti, A.B.; Arnold, G.P.; Cochrane, L.; Abboud, R.J. The Pedar® In-Shoe System: Repeatability and Normal Pressure Values. Gait Posture 2007, 25, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Barnett, S.; Cunningham, J.L.; West, S. A Comparison of Vertical Force and Temporal Parameters Produced by an In-Shoe Pressure Measuring System and a Force Platform. Clin. Biomech. 2001, 16, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Nagel, A.; Rosenbaum, D. Vacuum Cushioned Removable Cast Walkers Reduce Foot Loading in Patients with Diabetes Mellitus. Gait Posture 2009, 30, 11–15. [Google Scholar] [CrossRef]
- Ehrnthaller, C.; Rellensmann, K.; Baumbach, S.F.; Wuehr, M.; Schniepp, R.; Saller, M.M.; Böcker, W.; Polzer, H. Pedobarographic Evaluation of Five Commonly Used Orthoses for the Lower Extremity. Arch. Orthop. Trauma. Surg. 2022, 143, 4249–4256. [Google Scholar] [CrossRef]
- Puszczalowska-Lizis, E.; Koziol, K.; Omorczyk, J. Perception of Footwear Comfort and Its Relationship with the Foot Structure among Youngest-Old Women and Men. PeerJ 2021, 9, e12385. [Google Scholar] [CrossRef]
- Puszczalowska-Lizis, E.; Mikulakova, W.; Lizis, S.; Koziol, K.; Omorczyk, J. Relationships between the Perception of Footwear Comfort and the Fear of Falls in People at the Early Period of Old Age. Int. J. Environ. Res. Public Health 2022, 19, 6267. [Google Scholar] [CrossRef]
- Gerrard, J.M.; Bonanno, D.R.; Whittaker, G.A.; Landorf, K.B. Effect of Different Orthotic Materials on Plantar Pressures: A Systematic Review. J. Foot Ankle Res. 2020, 13, 35. [Google Scholar] [CrossRef]
- Simonds, E.; Colton, J.; Kogler, G.; Chang, Y.-H. Design and Testing of a Prototype Foot Orthosis That Uses the Principle of Granular Jamming. Prosthet. Orthot. Int. 2021, 45, 240–245. [Google Scholar] [CrossRef]
- Crenshaw, S.J.; Pollo, F.E.; Brodsky, J.W. The Effect of Ankle Position on Plantar Pressure in a Short Leg Walking Boot. Foot Ankle Int. 2004, 25, 69–72. [Google Scholar] [CrossRef]
- Bus, S.A.; Waaijman, R.; Arts, M.; Manning, H. The Efficacy of a Removable Vacuum-Cushioned Cast Replacement System in Reducing Plantar Forefoot Pressures in Diabetic Patients. Clin. Biomech. 2009, 24, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Zirngibl, B.; Grifka, J.; Baier, C.; Götz, J. Hallux Valgus. Orthopäde 2017, 46, 283–296. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.T.; Robinson, H.; Jude, E.; Rajbhandari, S. The Real-Life Outcome of VACOped Boot in the Management of Diabetic Foot Ulcers. Int. J. Low. Extremity Wounds 2022, 21, 290–293. [Google Scholar] [CrossRef] [PubMed]




| Foot Region | Comparison | Mean ± SD First Comparator | Mean ± SD Second Comparator | p-Value |
|---|---|---|---|---|
| Hindfoot | OTS vs. VACOpedes with vacuum inlay | 235.5 ± 40.5 | 205.5 ± 48.4 | 0.003 |
| OTS vs. VACOpedes with XELGO inlay | 235.5 ± 40.5 | 197.8 ± 37.6 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 205.5 ± 48.4 | 197.8 ± 37.6 | 0.704 | |
| Midfoot | OTS vs. VACOpedes with vacuum inlay | 147.9 ± 58.5 | 123.4 ± 40.7 | 0.007 |
| OTS vs. VACOpedes with XELGO inlay | 147.9 ± 58.5 | 121.3 ± 38.8 | 0.009 | |
| VACOpedes with vacuum- inlay vs. VACOpedes with XELGO inlay | 123.4 ± 40.7 | 121.3 ± 38.8 | 0.919 | |
| Forefoot | OTS vs. VACOpedes with vacuum inlay | 262.9 ± 58.4 | 202.1 ± 45.5 | <0.001 |
| OTS vs. VACOpedes with XELGO inlay | 262.9 ± 58.4 | 171 ± 46.9 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 202.1 ± 45.5 | 171 ± 46.9 | <0.001 |
| Foot Region | Comparison | Mean ± SD First Comparator | Mean ± SD Second Comparator | p-Value |
|---|---|---|---|---|
| Overall Forefoot | OTS vs. VACOpedes with vacuum inlay | 264.1 ± 12.1 | 201 ± 9.4 | <0.001 |
| OTS vs. VACOpedes with XELGO inlay | 264.1 ± 12.1 | 171 ± 9.6 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 201 ± 9.4 | 171 ± 9.6 | <0.001 | |
| Medial Forefoot | OTS vs. VACOpedes with vacuum inlay | 244.4 ± 13.8 | 181.7 ± 9.1 | <0.001 |
| OTS vs. VACOpedes with XELGO inlay | 244.4 ± 13.8 | 158.6 ± 10.3 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 181.7 ± 9.1 | 158.6 ± 10.3 | 0.002 | |
| Lateral Forefoot | OTS vs. VACOpedes with vacuum inlay | 201.5 ± 11.4 | 161.3 ± 9.5 | <0.001 |
| OTS vs. VACOpedes with XELGO inlay | 201.5 ± 11.4 | 153.3 ± 9.3 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 161.3 ± 9.5 | 153.3 ± 9.3 | 0.108 | |
| Big Toe | OTS vs. VACOpedes with vacuum inlay | 213.7 ± 13.1 | 137.7 ± 16.6 | <0.001 |
| OTS vs. VACOpedes with XELGO inlay | 213.7 ± 13.1 | 116.7 ± 12.1 | <0.001 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 137.7 ± 16.6 | 116.7 ± 12.1 | 0.088 | |
| Toes 2–5 | OTS vs. VACOpedes with vacuum inlay | 102.5 ± 7.2 | 96.1 ± 10.4 | 0.542 |
| OTS vs. VACOpedes with XELGO inlay | 102.5 ± 7.2 | 85.8 ± 8.9 | 0.023 | |
| VACOpedes with vacuum inlay vs. VACOpedes with XELGO inlay | 96.1 ± 10.4 | 85.8 ± 8.9 | 0.233 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milstrey, A.; Horst, C.; Gartung, S.; Weigel, A.-S.; Stange, R.; Ochman, S. Self-Adapting Foot Orthosis Inlay Facilitates Handling and Reduces Plantar Pressure Compared to Vacuum-Based Technology. J. Clin. Med. 2025, 14, 3384. https://doi.org/10.3390/jcm14103384
Milstrey A, Horst C, Gartung S, Weigel A-S, Stange R, Ochman S. Self-Adapting Foot Orthosis Inlay Facilitates Handling and Reduces Plantar Pressure Compared to Vacuum-Based Technology. Journal of Clinical Medicine. 2025; 14(10):3384. https://doi.org/10.3390/jcm14103384
Chicago/Turabian StyleMilstrey, Alexander, Carolin Horst, Stella Gartung, Ann-Sophie Weigel, Richard Stange, and Sabine Ochman. 2025. "Self-Adapting Foot Orthosis Inlay Facilitates Handling and Reduces Plantar Pressure Compared to Vacuum-Based Technology" Journal of Clinical Medicine 14, no. 10: 3384. https://doi.org/10.3390/jcm14103384
APA StyleMilstrey, A., Horst, C., Gartung, S., Weigel, A.-S., Stange, R., & Ochman, S. (2025). Self-Adapting Foot Orthosis Inlay Facilitates Handling and Reduces Plantar Pressure Compared to Vacuum-Based Technology. Journal of Clinical Medicine, 14(10), 3384. https://doi.org/10.3390/jcm14103384






