How Performing Chest Compressions Influences Mental Arithmetic Capabilities: A Randomized Cross-Over Trial
Abstract
1. Introduction
2. Materials and Methods
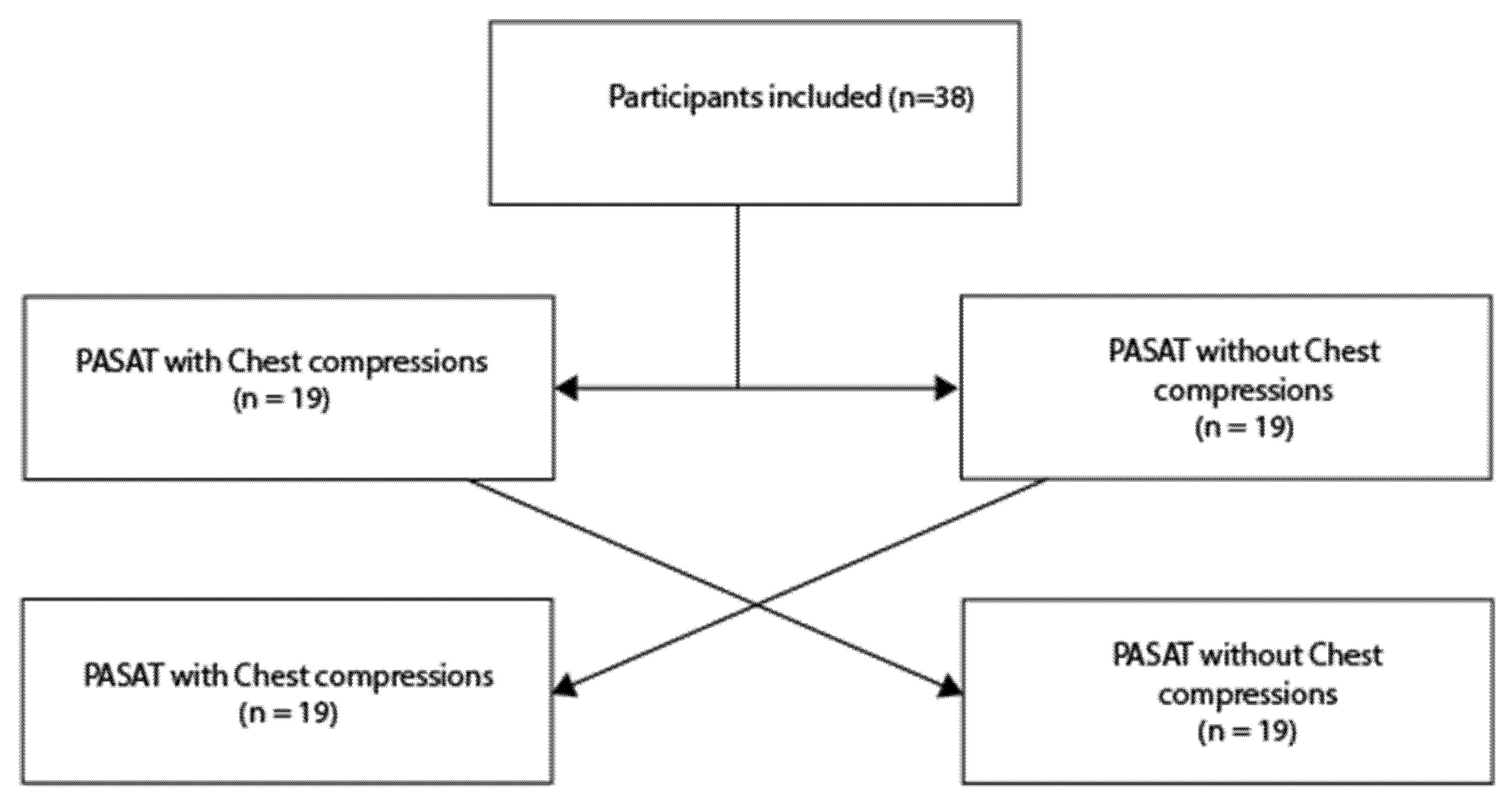
2.1. Study Design
2.2. Inclusion/Exclusion Criteria
2.3. Variables
2.4. Methodology
2.5. Randomization
2.6. Outcome
2.7. Sample Size Calculation
2.8. Statistical Analysis
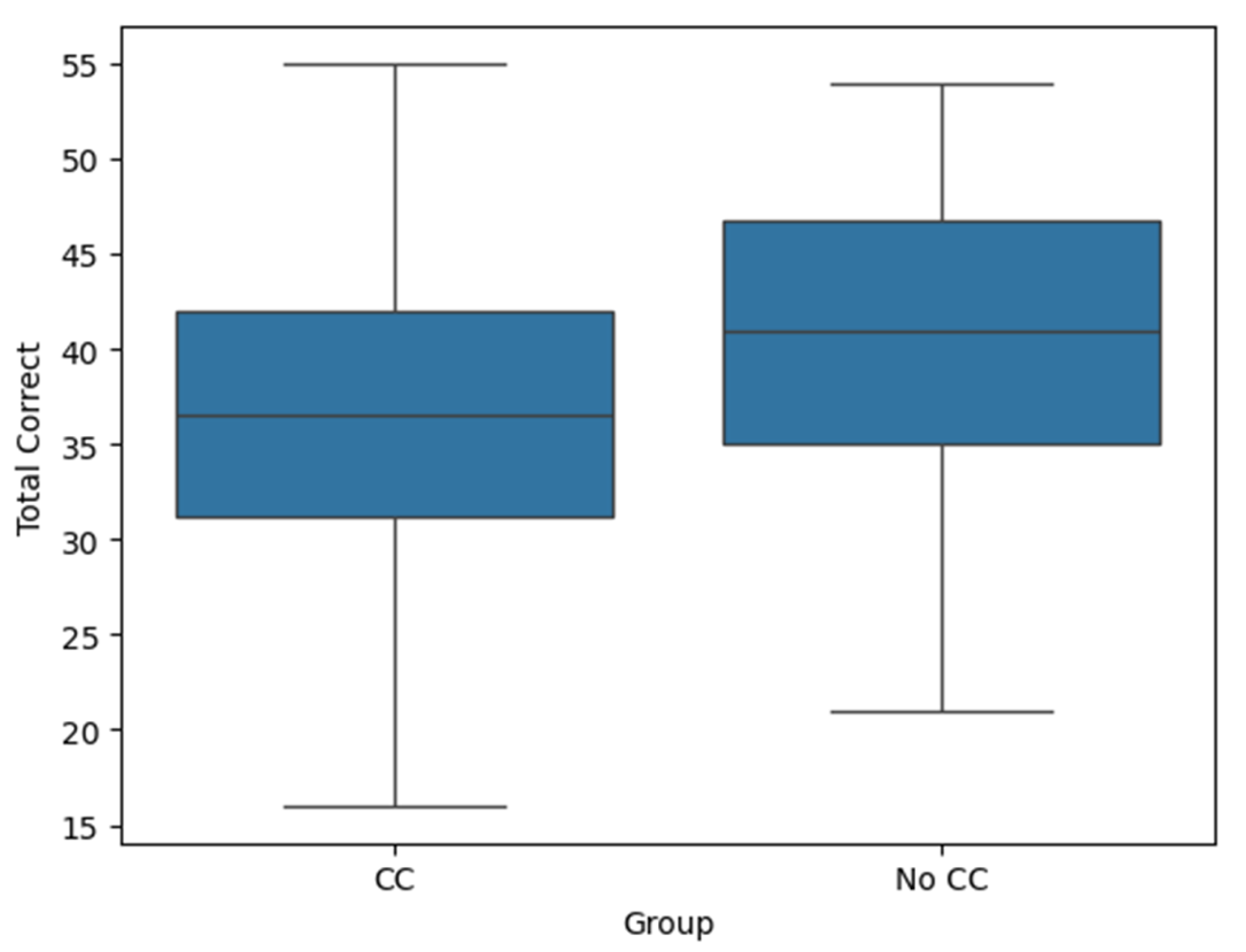
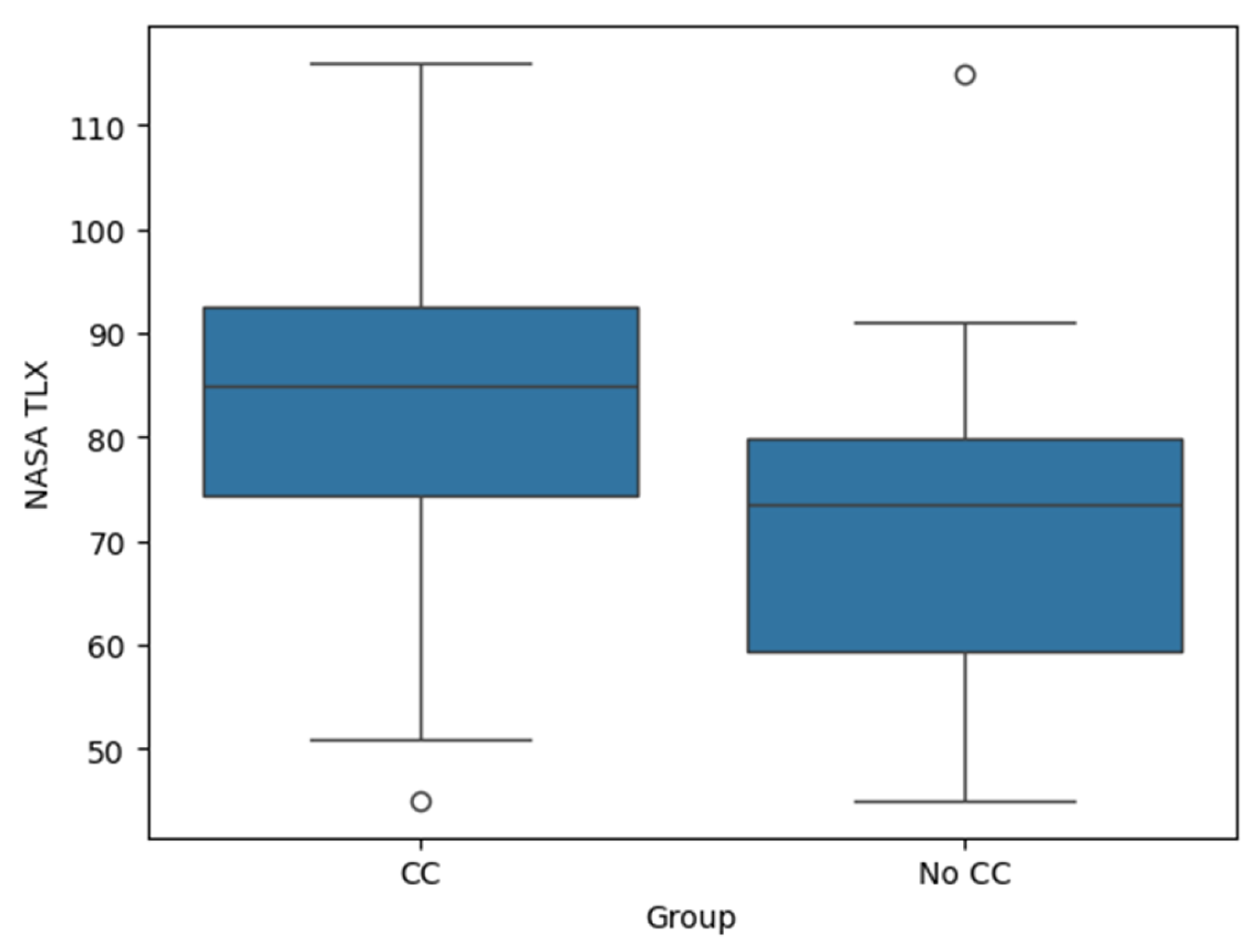
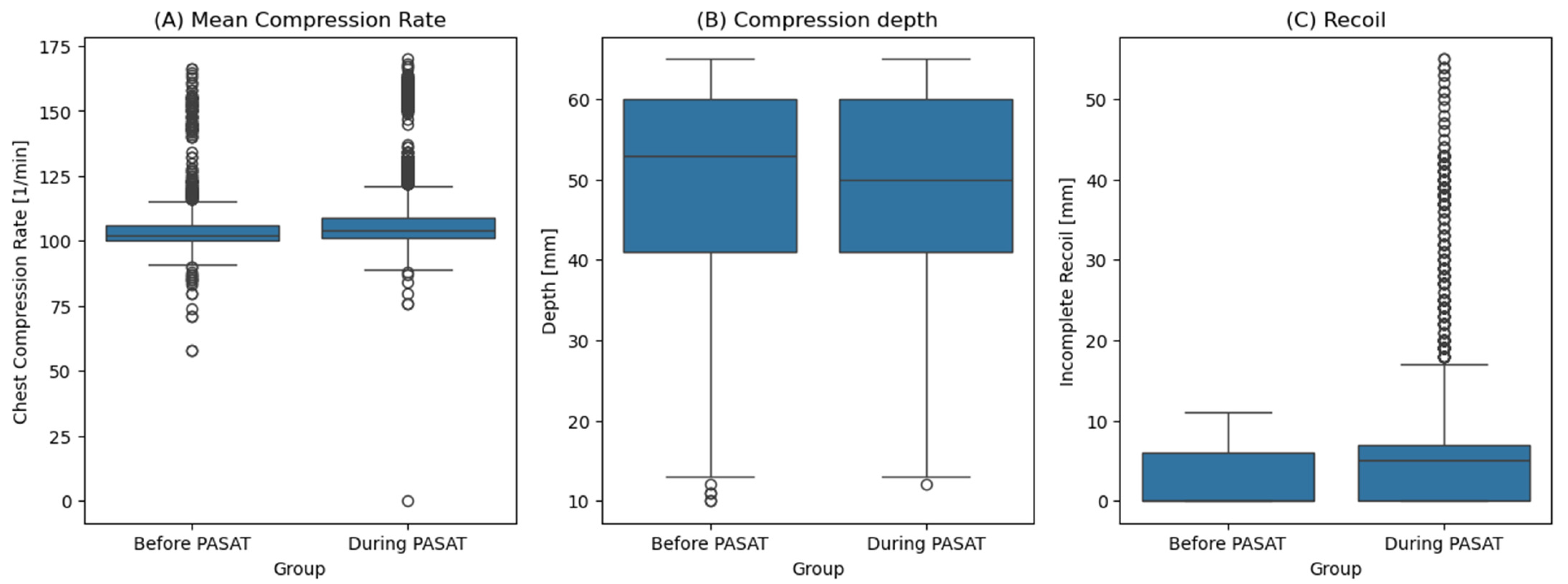
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PASAT | Paced Auditory Serial Addition Test |
| CC | Chest compression |
| NASA-TLX | National Aeronautics and Space Administration Task Load Index |
| CPR | Cardiopulmonary resuscitation |
| ERC | European Resuscitation Council |
| AHA | American Heart Association |
References
- Pashler, H. Dual-Task Interference in Simple Tasks: Data and Theory. Psychol. Bull. 1994, 116, 220–244. [Google Scholar] [CrossRef] [PubMed]
- Ward, N.; Hussey, E.K.; Cunningham, E.C.; Paul, E.J.; McWilliams, T.; Kramer, A.F. Building the Multitasking Brain: An Integrated Perspective on Functional Brain Activation During Task-Switching and Dual-Tasking. Neuropsychologia 2019, 132, 107149. [Google Scholar] [CrossRef] [PubMed]
- Worringer, B.; Langner, R.; Koch, I.; Eickhoff, S.B.; Eickhoff, C.R.; Binkofski, F.C. Common and Distinct Neural Correlates of Dual-Tasking and Task-Switching: A Meta-Analytic Review and a Neuro-Cognitive Processing Model of Human Multitasking. Brain Struct. Funct. 2019, 224, 1845–1869. [Google Scholar] [CrossRef] [PubMed]
- Skaugset, L.M.; Farrell, S.; Carney, M.; Wolff, M.; Santen, S.A.; Perry, M.; Cico, S.J. Can You Multitask? Evidence and Limitations of Task Switching and Multitasking in Emergency Medicine. Ann. Emerg. Med. 2016, 68, 189–195. [Google Scholar] [CrossRef]
- Augenstein, T.; Schneider, A.; Wehler, M.; Weigl, M. Multitasking Behaviors and Provider Outcomes in Emergency Department Physicians: Two Consecutive, Observational and Multi-Source Studies. Scand. J. Trauma. Resusc. Emerg. Med. 2021, 29, 14. [Google Scholar] [CrossRef]
- Kass, S.J.; Cole, K.S.; Stanny, C.J. Effects of Distraction and Experience on Situation Awareness and Simulated Driving. Transp. Res. Part. Traffic Psychol. Behav. 2007, 10, 321–329. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Raban, M.Z.; Walter, S.R.; Douglas, H. Task Errors by Emergency Physicians Are Associated with Interruptions, Multitasking, Fatigue and Working Memory Capacity: A Prospective, Direct Observation Study. BMJ Qual. Saf. 2018, 27, 655–663. [Google Scholar] [CrossRef]
- Sherbino, J.; Norman, G. Task Switching, Multitasking, and Errors: A Psychologic Perspective on the Impact of Interruptions. Ann. Emerg. Med. 2021, 78, 425–428. [Google Scholar] [CrossRef]
- Enz, S.; Hall, A.C.G.; Williams, K.K. The Myth of Multitasking and What It Means for Future Pharmacists. Am. J. Pharm. Educ. 2021, 85, 8267. [Google Scholar] [CrossRef]
- Guyette, F.X.; Reynolds, J.C.; Frisch, A. Post Cardiac Arrest Service Cardiac Arrest Resuscitation. Emerg. Med. Clin. North. Am. 2015, 33, 669–690. [Google Scholar] [CrossRef]
- Bailey, C.H.; Gesch, J.D. Team Strategies and Dynamics During Resuscitation. Emerg. Med. Clin. N. Am. 2023, 41, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Haerkens, M.H.T.M.; Kox, M.; Lemson, J.; Houterman, S.; van der Hoeven, J.G.; Pickkers, P. Crew Resource Management in the Intensive Care Unit: A Prospective 3-Year Cohort Study. Acta Anaesthesiol. Scand. 2015, 59, 1319–1329. [Google Scholar] [CrossRef] [PubMed]
- Kern, P.; Tschan, F.; Semmer, N.K.; Marsch, S. Effects of Team Leaders’ Position in Cardiopulmonary Resuscitation Teams on Leadership Behavior and Team Performance: A Prospective Randomized Interventional Cross-Over Simulation-Based Trial. Medicine 2023, 102, e34235. [Google Scholar] [CrossRef] [PubMed]
- Hunziker, S.; Johansson, A.C.; Tschan, F.; Semmer, N.K.; Rock, L.; Howell, M.D.; Marsch, S. Teamwork and Leadership in Cardiopulmonary Resuscitation. J. Am. Coll. Cardiol. 2011, 57, 2381–2388. [Google Scholar] [CrossRef]
- Lee, K.; Kim, M.J.; Park, J.; Park, J.M.; Kim, K.H.; Shin, D.W.; Kim, H.; Jeon, W.; Kim, H. The Effect of Distraction by Dual Work on a CPR Practitioner’s Efficiency in Chest Compression: A Randomized Controlled Simulation Study. Medicine 2017, 96, e8268. [Google Scholar] [CrossRef]
- Larraga-García, B.; Ruiz Bejerano, V.; Oregui, X.; Rubio-Bolívar, J.; Quintana-Díaz, M.; Gutiérrez, Á. Physiological and Performance Metrics During a Cardiopulmonary Real-Time Feedback Simulation to Estimate Cognitive Load. Displays 2024, 84, 102780. [Google Scholar] [CrossRef]
- Juliano, J.M.; Schweighofer, N.; Liew, S.-L. Increased Cognitive Load in Immersive Virtual Reality During Visuomotor Adaptation Is Associated with Decreased Long-Term Retention and Context Transfer. J. Neuroeng. Rehabil. 2022, 19, 106. [Google Scholar] [CrossRef]
- Gronwall, D.M. Paced Auditory Serial-Addition Task: A Measure of Recovery from Concussion. Percept. Mot. Ski. 1977, 44, 367–373. [Google Scholar] [CrossRef]
- Tombaugh, T.N. A Comprehensive Review of the Paced Auditory Serial Addition Test (PASAT). Arch. Clin. Neuropsychol. 2006, 21, 53–76. [Google Scholar] [CrossRef]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Advances in Psychology; Hancock, P.A., Meshkati, N., Eds.; Human Mental Workload; Elsevier: Amsterdam, The Netherlands, 1988; Volume 52, pp. 139–183. [Google Scholar]
- Favre-Félix, J.; Dziadzko, M.; Bauer, C.; Duclos, A.; Lehot, J.-J.; Rimmelé, T.; Lilot, M. High-Fidelity Simulation to Assess Task Load Index and Performance: A Prospective Observational Study. Turk. J. Anaesthesiol. Reanim. 2022, 50, 282–287. [Google Scholar] [CrossRef]
- Tubbs-Cooley, H.L.; Mara, C.A.; Carle, A.C.; Gurses, A.P. The NASA Task Load Index as a Measure of Overall Workload Among Neonatal, Paediatric and Adult Intensive Care Nurses. Intensive Crit. Care Nurs. 2018, 46, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.W.; Kong, J.C.H.; Clark, D.A.; Carne, P.; Skinner, S.; Pillinger, S.; Burton, P.; Brown, W. The National Aeronautics and Space Administration-Task Load Index: NASA-TLX: Evaluation of Its Use in Surgery. ANZ J. Surg. 2022, 92, 3022–3028. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, G.; Drake, F.L., Jr. Python Tutorial; Centrum voor Wiskunde en Informatica Amsterdam: Amsterdam, The Netherlands, 1995. [Google Scholar]
- Hirsch, P.; Pears, K.; Klasen, M.; Kiefer, C.; Koch, I.; Sopka, S. The Effects of Cognitive-Motor Multitasking Demands on the Quality of Chest Compressions in CPR-A Randomized Controlled Trial. Front. Med. 2025, 12, 1536796. [Google Scholar] [CrossRef] [PubMed]
- Howard, S.K.; Gaba, D.M.; Fish, K.J.; Yang, G.; Sarnquist, F.H. Anesthesia Crisis Resource Management Training: Teaching Anesthesiologists to Handle Critical Incidents. Aviat. Space Environ. Med. 1992, 63, 763–770. [Google Scholar]
- Vincent, A.; Semmer, N.K.; Becker, C.; Beck, K.; Tschan, F.; Bobst, C.; Schuetz, P.; Marsch, S.; Hunziker, S. Does Stress Influence the Performance of Cardiopulmonary Resuscitation? A Narrative Review of the Literature. J. Crit. Care 2021, 63, 223–230. [Google Scholar] [CrossRef]
- Groombridge, C.J.; Kim, Y.; Maini, A.; Smit, D.V.; Fitzgerald, M.C. Stress and Decision-Making in Resuscitation: A Systematic Review. Resuscitation 2019, 144, 115–122. [Google Scholar] [CrossRef]
- Pammi, M.; Dempsey, E.M.; Ryan, C.A.; Barrington, K.J. Newborn Resuscitation Training Programmes Reduce Early Neonatal Mortality. Neonatology 2016, 110, 210–224. [Google Scholar] [CrossRef]
- Meaney, P.A.; Topjian, A.A.; Chandler, H.K.; Botha, M.; Soar, J.; Berg, R.A.; Nadkarni, V.M. Resuscitation Training in Developing Countries: A Systematic Review. Resuscitation 2010, 81, 1462–1472. [Google Scholar] [CrossRef]
- Anderson, R.; Sebaldt, A.; Lin, Y.; Cheng, A. Optimal Training Frequency for Acquisition and Retention of High-Quality CPR Skills: A Randomized Trial. Resuscitation 2019, 135, 153–161. [Google Scholar] [CrossRef]
- Soar, J.; Böttiger, B.W.; Carli, P.; Couper, K.; Deakin, C.D.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult Advanced Life Support. Resuscitation 2021, 161, 115–151. [Google Scholar] [CrossRef]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Zuercher, M.; Hilwig, R.W.; Ranger-Moore, J.; Nysaether, J.; Nadkarni, V.M.; Berg, M.D.; Kern, K.B.; Sutton, R.; Berg, R.A. Leaning During Chest Compressions Impairs Cardiac Output and Left Ventricular Myocardial Blood Flow in Piglet Cardiac Arrest. Crit. Care Med. 2010, 38, 1141–1146. [Google Scholar] [CrossRef]
| Overall | CC First Group | No CC First Group | |
|---|---|---|---|
| Age group (%) | |||
| 20–25 | 5 (13.2%) | 3 (15.8%) | 2 (10.5%) |
| 25–30 | 8 (21.1%) | 5 (26.3%) | 3 (15.8%) |
| 30–35 | 11 (28.9%) | 5 (26.3%) | 6 (31.6%) |
| 35–40 | 11 (28.9%) | 5 (26.3%) | 6 (31.6%) |
| 40–45 | 1 (2.6%) | 0 | 1 (5.3%) |
| 50–55 | 1 (2.6%) | 0 | 1 (5.3%) |
| 55–60 | 1 (2.6%) | 1 (5.3%) | 0 |
| Female Sex (%) | 17 (44.7%) | 7 (36.8%) | 10 (52.6%) |
| Male Sex (%) | 21 (55.3%) | 12 (63.2%) | 9 (47.4%) |
| Specialty (%) | |||
| Physician (Anaesthesia) | 17 (44.7%) | 6 (31.6%) | 11 (57.9%) |
| Physician (Internal Medicine) | 7 (18.4%) | 4 (21.1%) | 3 (15.8%) |
| Nurse | 7 (18.4%) | 4 (21.1%) | 3 (15.8%) |
| Paramedic | 7 (18.4%) | 5 (26.3%) | 2 (10.5%) |
| Time since last CPR Training [month] (IQR) | 4.3 (3.0, 7.1) | 4.3 (1.9, 5.6) | 4.4 (3.3, 12.5) |
| Before PASAT | During PASAT | |
|---|---|---|
| Compression Depth [mm] | 53.0, (41.0, 60.0) | 50.0, (41.0, 60.0) |
| Mean Compression Rate [/min] | 102.0, (100.0, 106.0) | 104.0, (101.0, 109.0) |
| Recoil [mm] | 0.0, (0.0, 6.0) | 5.0, (0.0, 7.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holaubek, C.; Maleczek, M.; Scheidl, M.; Maleczek, A.; Frimmel, N.; Goschin, J.; Roessler, B. How Performing Chest Compressions Influences Mental Arithmetic Capabilities: A Randomized Cross-Over Trial. J. Clin. Med. 2025, 14, 3366. https://doi.org/10.3390/jcm14103366
Holaubek C, Maleczek M, Scheidl M, Maleczek A, Frimmel N, Goschin J, Roessler B. How Performing Chest Compressions Influences Mental Arithmetic Capabilities: A Randomized Cross-Over Trial. Journal of Clinical Medicine. 2025; 14(10):3366. https://doi.org/10.3390/jcm14103366
Chicago/Turabian StyleHolaubek, Caroline, Mathias Maleczek, Maximilian Scheidl, Anna Maleczek, Nikolaus Frimmel, Julius Goschin, and Bernhard Roessler. 2025. "How Performing Chest Compressions Influences Mental Arithmetic Capabilities: A Randomized Cross-Over Trial" Journal of Clinical Medicine 14, no. 10: 3366. https://doi.org/10.3390/jcm14103366
APA StyleHolaubek, C., Maleczek, M., Scheidl, M., Maleczek, A., Frimmel, N., Goschin, J., & Roessler, B. (2025). How Performing Chest Compressions Influences Mental Arithmetic Capabilities: A Randomized Cross-Over Trial. Journal of Clinical Medicine, 14(10), 3366. https://doi.org/10.3390/jcm14103366






