Perioperative Risk in Adults with Congenital Heart Disease Undergoing Non-Cardiac Surgery: Challenges and Tailored Strategies
Abstract
1. Epidemiology
2. Risk Stratification
2.1. Surgery-Related Risk
2.2. Patient-Related Risk
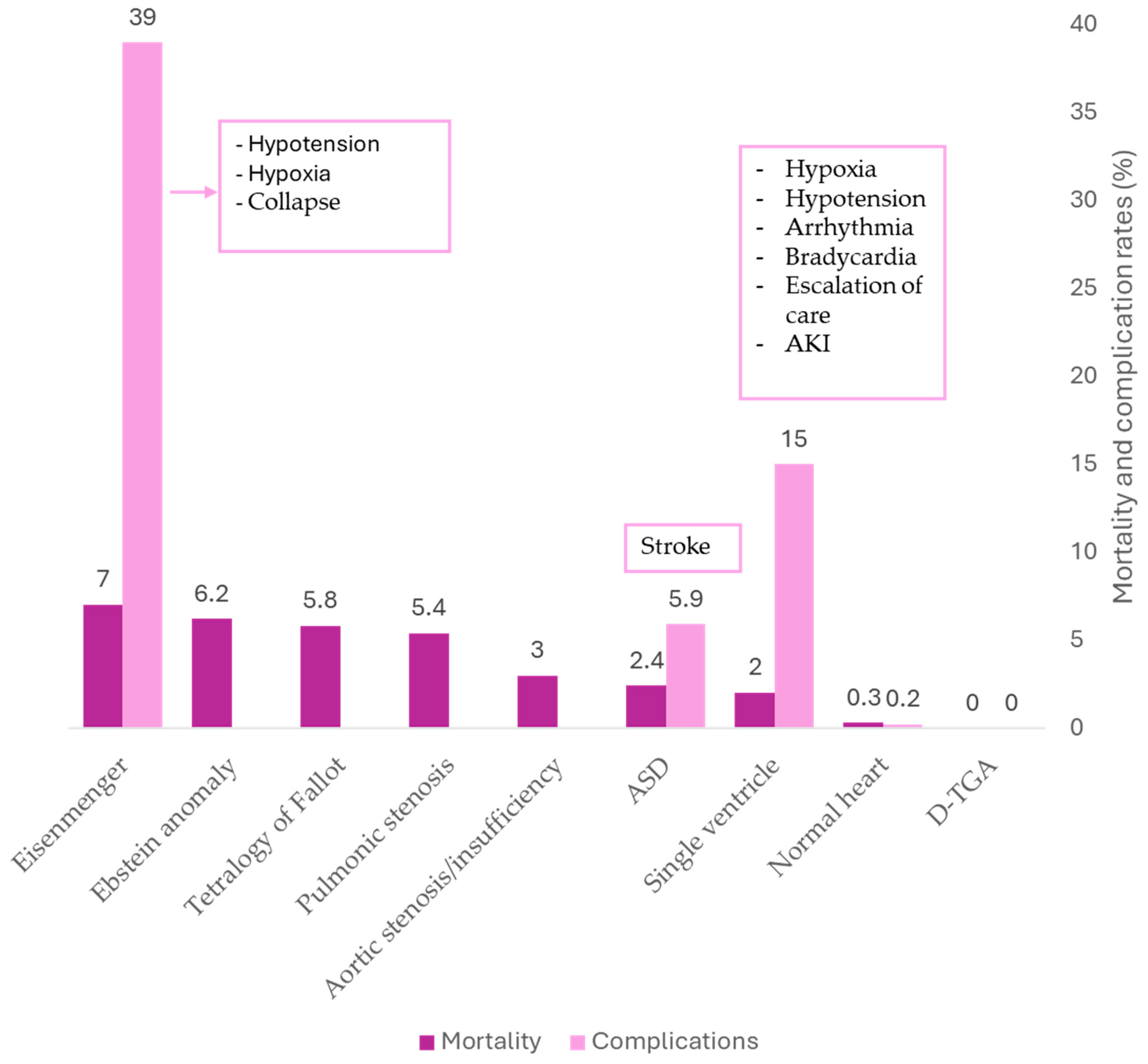
3. Risk in Specific CHD Lesions
3.1. Patients with ASD/PFO
3.2. Patients with Fontan Circulation
3.3. Patients with a Transposition of the Great Arteries
3.4. Patients with Cyanotic Congenital Heart Disease and Eisenmenger
3.5. Comorbidities in ACHD and Their Impact on Non-Cardiac Surgery
4. Perioperative Risk Stratification and Referral Strategy in ACHD Patients
5. Conclusions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACHD | Adult congenital heart disease |
| ACS-NSQIP | American College of Surgeons National Quality Improvement Program |
| ASD | Atrial septal defect |
| CAE, | Carotid artery endarterectomy |
| CAS | Carotid artery stenting |
| CCHD | Cyanotic congenital heart disease |
| CHD | Congenital heart disease |
| NC | Non-cardiac |
| RCRI | Revised Cardiac Risk Index |
| SVR | Systemic vascular resistance |
| TGA | Transposition of the great arteries |
| VATS | Video-assisted thoracoscopic surgery |
References
- Mandalenakis, Z.; Giang, K.W.; Eriksson, P.; Liden, H.; Synnergren, M.; Wåhlander, H.; Fedchenko, M.; Rosengren, A.; Dellborg, M. Survival in Children with Congenital Heart Disease: Have We Reached a Peak at 97%? J. Am. Heart. Assoc. 2020, 9, e017704. [Google Scholar] [CrossRef] [PubMed]
- Moons, P.; Bovijn, L.; Budts, W.; Belmans, A.; Gewillig, M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 2010, 122, 2264–2272. [Google Scholar] [CrossRef] [PubMed]
- Benziger, C.P.; Stout, K.; Zaragoza-Macias, E.; Bertozzi-Villa, A.; Flaxman, A.D. Projected growth of the adult congenital heart disease population in the United States to 2050: An integrative systems modeling approach. Popul. Health Metr. 2015, 13, 29. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, B.G.; Wong, J.K.; Kin, C.; Lobato, R.L. Perioperative outcomes of major noncardiac surgery in adults with congenital heart disease. Anesthesiology 2013, 119, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Williamson, C.G.; Ebrahimian, S.; Ascandar, N.; Sanaiha, Y.; Sakowitz, S.; Biniwale, R.M.; Benharash, P. Major elective non-cardiac operations in adults with congenital heart disease. Heart 2023, 109, 202–207. [Google Scholar] [CrossRef]
- Maxwell, B.G.; Wong, J.K.; Lobato, R.L. Perioperative morbidity and mortality after noncardiac surgery in young adults with congenital or early acquired heart disease: A retrospective cohort analysis of the National Surgical Quality Improvement Program database. Am. Surg. 2014, 80, 321–326. [Google Scholar] [CrossRef]
- Egbe, A.C.; Khan, A.R.; Ammash, N.M.; Barbara, D.W.; Oliver, W.C.; Said, S.M.; Akintoye, E.; Warnes, C.A.; Connolly, H.M. Predictors of procedural complications in adult Fontan patients undergoing non-cardiac procedures. Heart 2017, 103, 1813–1820. [Google Scholar] [CrossRef]
- Halvorsen, S.; Mehilli, J.; Cassese, S.; Hall, T.S.; Abdelhamid, M.; Barbato, E.; De Hert, S.; de Laval, I.; Geisler, T.; Hinterbuchner, L.; et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur. Heart J. 2022, 43, 3826–3924. [Google Scholar]
- Sakowitz, S.; Bakhtiyar, S.S.; Ali, K.; Mallick, S.; Williamson, C.; Benharash, P. Outcomes following major thoracoabdominal cancer resection in adults with congenital heart disease. PLoS ONE 2024, 19, e0295767. [Google Scholar] [CrossRef]
- Maxwell, B.G.; Posner, K.L.; Wong, J.K.; Oakes, D.A.; Kelly, N.E.; Domino, K.B.; Ramamoorthy, C. Factors contributing to adverse perioperative events in adults with congenital heart disease: A structured analysis of cases from the closed claims project. Congenit. Heart Dis. 2015, 10, 21–29. [Google Scholar] [CrossRef]
- Bennett, J.M.; Ehrenfeld, J.M.; Markham, L.; Eagle, S.S. Anesthetic management and outcomes for patients with pulmonary hypertension and intracardiac shunts and Eisenmenger syndrome: A review of institutional experience. J. Clin. Anesth. 2014, 26, 286–293. [Google Scholar] [CrossRef]
- Christensen, R.E.; Reynolds, P.I.; Bukowski, B.K.; Malviya, S. Anaesthetic management and outcomes in patients with surgically corrected D-transposition of the great arteries undergoing non-cardiac surgery. Br. J. Anaesth. 2010, 104, 12–15. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Villablanca, P.A.; Lemor, A.; So, C.Y.; Kang, G.; Jain, T.; Gupta, T.; Ando, T.; Mohananey, D.; Ranka, S.; Hernandez-Suarez, D.F.; et al. Increased Risk of Perioperative Ischemic Stroke in Patients Who Undergo Noncardiac Surgery with Preexisting Atrial Septal Defect or Patent Foramen Ovale. J. Cardiothorac. Vasc. Anesth. 2020, 34, 2060–2068. [Google Scholar] [CrossRef] [PubMed]
- Smilowitz, N.R.; Subashchandran, V.; Berger, J.S. Atrial Septal Defect and the Risk of Ischemic Stroke in the Perioperative Period of Noncardiac Surgery. Am. J. Cardiol. 2019, 124, 1120–1124. [Google Scholar] [CrossRef] [PubMed]
- Lui, G.K.; Saidi, A.; Bhatt, A.B.; Burchill, L.J.; Deen, J.F.; Earing, M.G.; Gewitz, M.; Ginns, J.; Kay, J.D.; Kim, Y.Y.; et al. Diagnosis and Management of Noncardiac Complications in Adults with Congenital Heart Disease: A Scientific Statement from the American Heart Association. Circulation 2017, 136, e348–e392. [Google Scholar] [CrossRef]
- McClain, C.D.; McGowan, F.X.; Kovatsis, P.G. Laparoscopic surgery in a patient with Fontan physiology. Anesth. Analg. 2006, 103, 856–858. [Google Scholar] [CrossRef]
- Brown, M.L.; Cradeur, M.; Staffa, S.J.; Nasr, V.G.; Hernandez, M.R.; DiNardo, J.A. Anaesthesia for non-cardiac surgery in children and young adults with Fontan physiology. Cardiol. Young 2023, 33, 1896–1901. [Google Scholar] [CrossRef]
- McCrindle, B.W.; Manlhiot, C.; Cochrane, A.; Roberts, R.; Hughes, M.; Szechtman, B.; Weintraub, R.; Andrew, M.; Monagle, P.; Fontan Anticoagulation Study Group. Factors associated with thrombotic complications after the Fontan procedure: A secondary analysis of a multicenter, randomized trial of primary thromboprophylaxis for 2 years after the Fontan procedure. J. Am. Coll. Cardiol. 2013, 61, 346–353. [Google Scholar] [CrossRef]
- Brida, M.; Diller, G.P.; Gatzoulis, M.A. Systemic Right Ventricle in Adults with Congenital Heart Disease. Circulation 2018, 137, 508–518. [Google Scholar] [CrossRef]
- Oechslin, E. Management of adults with cyanotic congenital heart disease. Heart 2015, 101, 485–494. [Google Scholar] [CrossRef]
- Hjortshøj, C.M.S.; Kempny, A.; Jensen, A.S.; Sørensen, K.; Nagy, E.; Dellborg, M.; Johansson, B.; Rudiene, V.; Hong, G.; Opotowsky, A.R. Past and current cause-specific mortality in Eisenmenger syndrome. Eur. Heart J. 2017, 38, 2060–2067. [Google Scholar] [CrossRef] [PubMed]
- Ammash, N.M.; Connolly, H.M.; Abel, M.D.; Warnes, C.A. Noncardiac surgery in Eisenmenger syndrome. J. Am. Coll. Cardiol. 1999, 33, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Ammash, N.; Warnes, C.A. Cerebrovascular events in adult patients with cyanotic congenital heart disease. J. Am. Coll. Cardiol. 1996, 28, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Niwa, K.; Perloff, J.K.; Kaplan, S.; Child, J.S.; Miner, P.D. Eisenmenger syndrome in adults: Ventricular septal defect, truncus arteriosus, univentricular heart. J. Am. Coll. Cardiol. 1999, 34, 223–232. [Google Scholar] [CrossRef]
- Cannesson, M.; Earing, M.G.; Collange, V.; Kersten, J.R. Anesthesia for noncardiac surgery in adults with congenital heart disease. Anesthesiology 2009, 111, 432–440. [Google Scholar] [CrossRef]
- Baum, V.C.; Perloff, J.K. Anesthetic implications of adults with congenital heart disease. Anesth. Analg. 1993, 76, 1342–1358. [Google Scholar] [CrossRef]
- Oechslin, E. Hematological management of the cyanotic adult with congenital heart disease. Int. J. Cardiol. 2004, 97 (Suppl. S1), 109–115. [Google Scholar] [CrossRef]
- El-Chouli, M.; Meddis, A.; Christensen, D.M.; Gerds, T.A.; Sehested, T.; Malmborg, M.; Phelps, M.; Bang, C.N.; Ahlehoff, O.; Torp-Pedersen, C.; et al. Lifetime risk of comorbidity in patients with simple congenital heart disease: A Danish nationwide study. Eur. Heart J. 2023, 44, 741–748. [Google Scholar] [CrossRef]
- Bracher, I.; Padrutt, M.; Bonassin, F.; Santos Lopes, B.; Gruner, C.; Stämpfli, S.F.; Oxenius, A.; De Pasquale, G.; Seeliger, T.; Lüscher, T.F.; et al. Burden and impact of congenital syndromes and comorbidities among adults with congenital heart disease. Int. J. Cardiol. 2017, 240, 159–164. [Google Scholar] [CrossRef]
- Neidenbach, R.C.; Lummert, E.; Vigl, M.; Zachoval, R.; Fischereder, M.; Engelhardt, A.; Pujol, C.; Oberhoffer, R.; Nagdyman, N.; Ewert, P. Non-cardiac comorbidities in adults with inherited and congenital heart disease: Report from a single center experience of more than 800 consecutive patients. Cardiovasc. Diagn. Ther. 2018, 8, 423–431. [Google Scholar] [CrossRef]
- Ginde, S.; Bartz, P.J.; Hill, G.D.; Danduran, M.J.; Biller, J.; Sowinski, J.; Tweddell, J.S.; Earing, M.G. Restrictive lung disease is an independent predictor of exercise intolerance in the adult with congenital heart disease. Congenit. Heart Dis. 2013, 8, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Harden, B.; Tian, X.; Giese, R.; Nakhleh, N.; Kureshi, S.; Francis, R.; Hanumanthaiah, S.; Li, Y.; Swisher, M.; Kuehl, K. Increased postoperative respiratory complications in heterotaxy congenital heart disease patients with respiratory ciliary dysfunction. J. Thorac. Cardiovasc. Surg. 2014, 147, 1291–1298.e2. [Google Scholar] [CrossRef]
- Swisher, M.; Jonas, R.; Tian, X.; Lee, E.S.; Lo, C.W.; Leatherbury, L. Increased postoperative and respiratory complications in patients with congenital heart disease associated with heterotaxy. J. Thorac. Cardiovasc. Surg. 2011, 141, 637–644.e1–3. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, K.; Diller, G.P.; Koltsida, E.; Pijuan-Domenech, A.; Papadopoulou, S.A.; Babu-Narayan, S.V.; Salukhe, T.V.; Piepoli, M.F.; Poole-Wilson, P.A.; Best, N.; et al. Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation 2008, 117, 2320–2328. [Google Scholar] [CrossRef] [PubMed]
- Daelman, B.; Van Bulck, L.; Luyckx, K.; Kovacs, A.H.; Van De Bruaene, A.; Ladouceur, M.; Yang, H.-L.; Moon, J.R.; Schmidt, A.; Lykkeberg, B.; et al. Frailty and Cognitive Function in Middle-Aged and Older Adults with Congenital Heart Disease. J. Am. Coll. Cardiol. 2024, 83, 1149–1159. [Google Scholar] [CrossRef]
- Hornor, M.A.; Ma, M.; Zhou, L.; Cohen, M.E.; Rosenthal, R.A.; Russell, M.M.; Ko, C.Y. Enhancing the American College of Surgeons NSQIP Surgical Risk Calculator to Predict Geriatric Outcomes. J. Am. Coll. Surg. 2020, 230, 88–100.e1. [Google Scholar] [CrossRef]
- Diller, G.P.; Lammers, A.E.; Fischer, A.; Orwat, S.; Nienhaus, K.; Schmidt, R.; Radke, R.M.; De-Torres-Alba, F.; Kaleschke, G.; Marschall, U.; et al. Immunodeficiency is prevalent in congenital heart disease and associated with increased risk of emergency admissions and death. Eur. Heart J. 2023, 44, 3250–3260. [Google Scholar] [CrossRef]
- Wienecke, L.M.; Cohen, S.; Bauersachs, J.; Mebazaa, A.; Chousterman, B.G. Immunity and inflammation: The neglected key players in congenital heart disease? Heart Fail Rev. 2022, 27, 1957–1971. [Google Scholar] [CrossRef]
- Freisinger, E.; Gerß, J.; Makowski, L.; Marschall, U.; Reinecke, H.; Baumgartner, H.; Koeppe, J.; Diller, G.-P. Current use and safety of novel oral anticoagulants in adults with congenital heart disease: Results of a nationwide analysis including more than 44 000 patients. Eur. Heart J. 2020, 41, 4168–4177. [Google Scholar] [CrossRef]
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e637–e697. [Google Scholar] [CrossRef]
- Tafer, N.; Langouet, E.; Alacoque, X.; Amedro, P.; Bojan, M.; Bruyère, M.; Cholley, B.; Koffel, C.; Ladouceur, M.; Lebel, S.; et al. Guidelines for anaesthesia of adults with congenital heart disease in non-cardiac surgery. Anaesth. Crit. Care Pain Med. 2025, 29, 101540. [Google Scholar] [CrossRef]
- Maxwell, B.G.; Maxwell, T.G.; Wong, J.K. Decentralization of care for adults with congenital heart disease in the United States: A geographic analysis of outpatient surgery. PLoS ONE 2014, 9, e106730. [Google Scholar] [CrossRef]
| Procedure Type | Maxwell (2002–2009) [4] | Williamson (2010–2018) [5] | |
|---|---|---|---|
| General Surgery | 35.1% | Colectomy | 21.6% |
| Gastrectomy | 3.42% | ||
| Hepatectomy | 2.56% | ||
| Abdominal Aortic Aneurysm | 5.16% | ||
| Esophagectomy | 0.48% | ||
| Orthopedic Surgery | 29.9% | Hip Replacement | 48.7% |
| Thoracic Surgery | 13.9% | Lung Resection | 18.0% |
| Ear, Nose, Throat | 2.3% | - | - |
| Gynecologic Surgery | 7.7% | - | - |
| Neurosurgery | 12.0% | - | - |
| Urologic Surgery | 6.0% | - | - |
| Low Surgical Risk (<1%) | Intermediate Surgical Risk (1–5%) | High Surgical Risk (>5%) |
|---|---|---|
| Breast surgery | Carotid asymptomatic (CEA or CAS) | Adrenal resection |
| Dental procedures | Carotid symptomatic (CEA) | Aortic and major vascular surgery |
| Thyroid surgery | Endovascular aortic aneurysm repair | Carotid symptomatic (CAS) |
| Eye surgery | Head or neck surgery | Duodenal-pancreatic surgery |
| Gynecological: minor | Intraperitoneal: splenectomy, hiatal hernia repair, cholecystectomy | Liver resection, bile duct surgery |
| Orthopedic minor (meniscectomy) | Intrathoracic: nonmajor | Esophagectomy |
| Reconstructive surgery | Neurological or orthopedic: major (hip and spine surgery) | Open lower limb revascularization for acute limb ischemia or amputation |
| Superficial surgery | Peripheral arterial angioplasty | Pneumonectomy (VATS or open surgery) |
| Urological minor: transurethral resection of the prostate | Renal transplants | Pulmonary or liver transplant |
| VATS minor lung resection | Urological or gynecological: major | Repair of perforated bowel |
| Total cystectomy |
| CHD | Preoperative Risk | Intraoperative Risk | Postoperative Risk |
|---|---|---|---|
| ASD/PFO | Increased risk of perioperative ischemic stroke; echocardiographic screening may be needed | High stroke risk during major surgery due to paradoxical embolism | Elevated risk of stroke and mortality within 30 days |
| Fontan circulation | Severe hemodynamic vulnerability; cyanosis increases risk; frequent end-organ dysfunction | Hypoxia, hypotension, and arrhythmias common; anesthesia and mechanical ventilation reduce preload and cardiac output | Escalation of care, AKI, and heart failure in a small proportion of cases |
| Systemic right ventricle (D-TGA/ccTGA) | High risk of arrhythmias and systemic ventricular dysfunction | Bradycardia, bleeding, and failed extubation; systemic right ventricle may poorly tolerate anesthesia-induced changes, especially in severe dysfunction; limited outcome data in adults | Limited data; possible postoperative arrhythmia and heart failure |
| Cyanotic CHD/Eisenmenger syndrome | Fixed PVR, severe cyanosis, coagulopathy, and embolic risk; requires careful optimization | Profound hypotension and desaturation; highly sensitive to anesthetic induction and hemodynamic shifts; require use of vasopressor High risk of paradoxical embolism | High risk of decompensation and death |
| ACHD-related comorbidities | Frailty, restrictive lung disease, renal impairment, immune dysfunction, and genetic syndromes are prevalent | Increased ventilatory challenges; higher bleeding risk from anticoagulation or liver dysfunction | Risk of delirium, infections, thromboembolic or bleeding events, and prolonged recovery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ladouceur, M.; Valacco, L.; Ltaief, Z.; Rutz, T.; Hascoet, S.; Bouchardy, J. Perioperative Risk in Adults with Congenital Heart Disease Undergoing Non-Cardiac Surgery: Challenges and Tailored Strategies. J. Clin. Med. 2025, 14, 3340. https://doi.org/10.3390/jcm14103340
Ladouceur M, Valacco L, Ltaief Z, Rutz T, Hascoet S, Bouchardy J. Perioperative Risk in Adults with Congenital Heart Disease Undergoing Non-Cardiac Surgery: Challenges and Tailored Strategies. Journal of Clinical Medicine. 2025; 14(10):3340. https://doi.org/10.3390/jcm14103340
Chicago/Turabian StyleLadouceur, Magalie, Lena Valacco, Zied Ltaief, Tobias Rutz, Sébastien Hascoet, and Judith Bouchardy. 2025. "Perioperative Risk in Adults with Congenital Heart Disease Undergoing Non-Cardiac Surgery: Challenges and Tailored Strategies" Journal of Clinical Medicine 14, no. 10: 3340. https://doi.org/10.3390/jcm14103340
APA StyleLadouceur, M., Valacco, L., Ltaief, Z., Rutz, T., Hascoet, S., & Bouchardy, J. (2025). Perioperative Risk in Adults with Congenital Heart Disease Undergoing Non-Cardiac Surgery: Challenges and Tailored Strategies. Journal of Clinical Medicine, 14(10), 3340. https://doi.org/10.3390/jcm14103340






