Approach to Mental Health Through a Frequency Modulated Auditory Intervention: A Controlled and Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
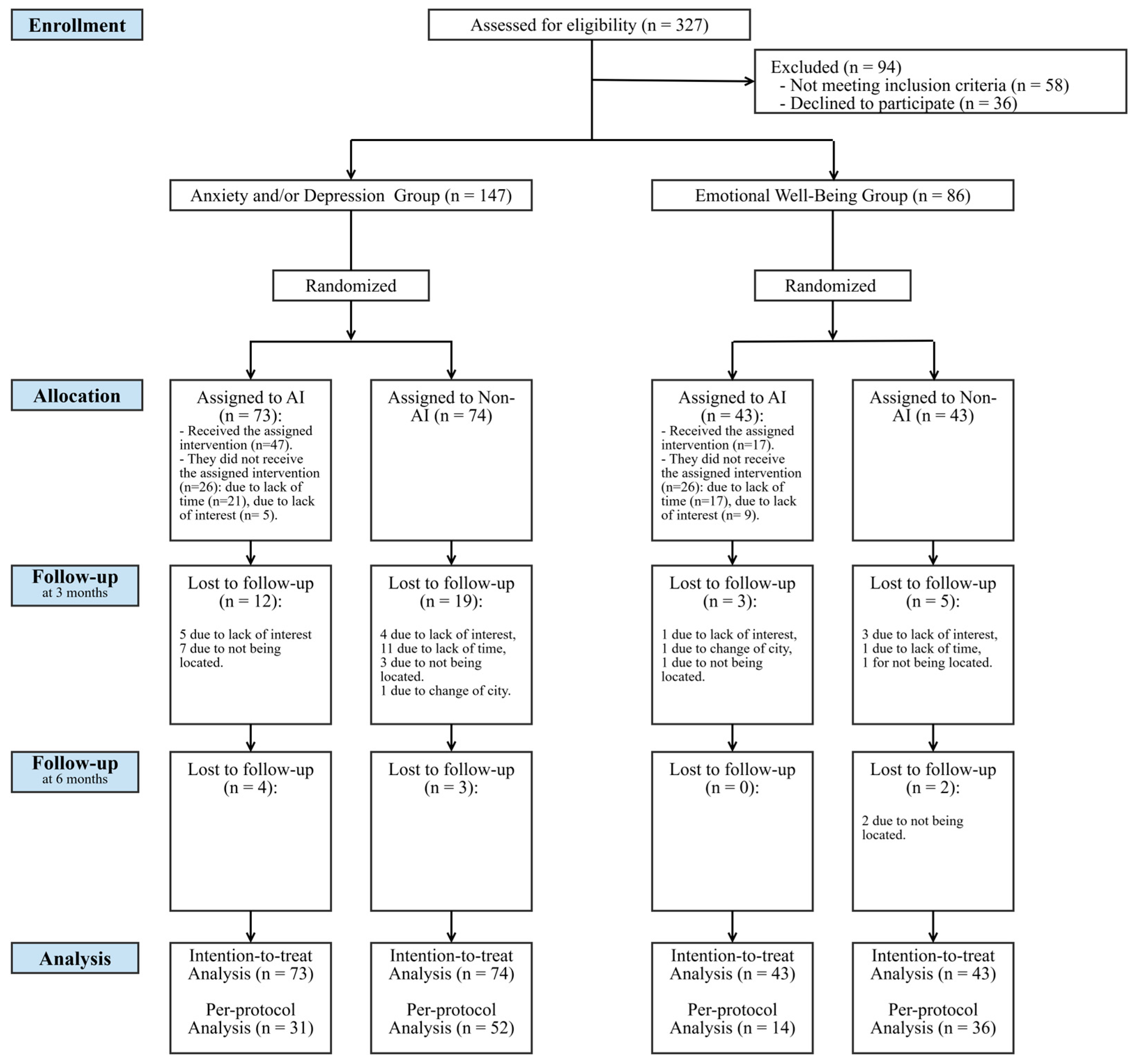
2.1. Study Type
2.2. Sample Size Determination
2.3. Population
2.4. Assignment to Study Groups
2.5. Auditory Intervention (AI)
2.6. Absence of Hearing Intervention
2.7. Study Variables
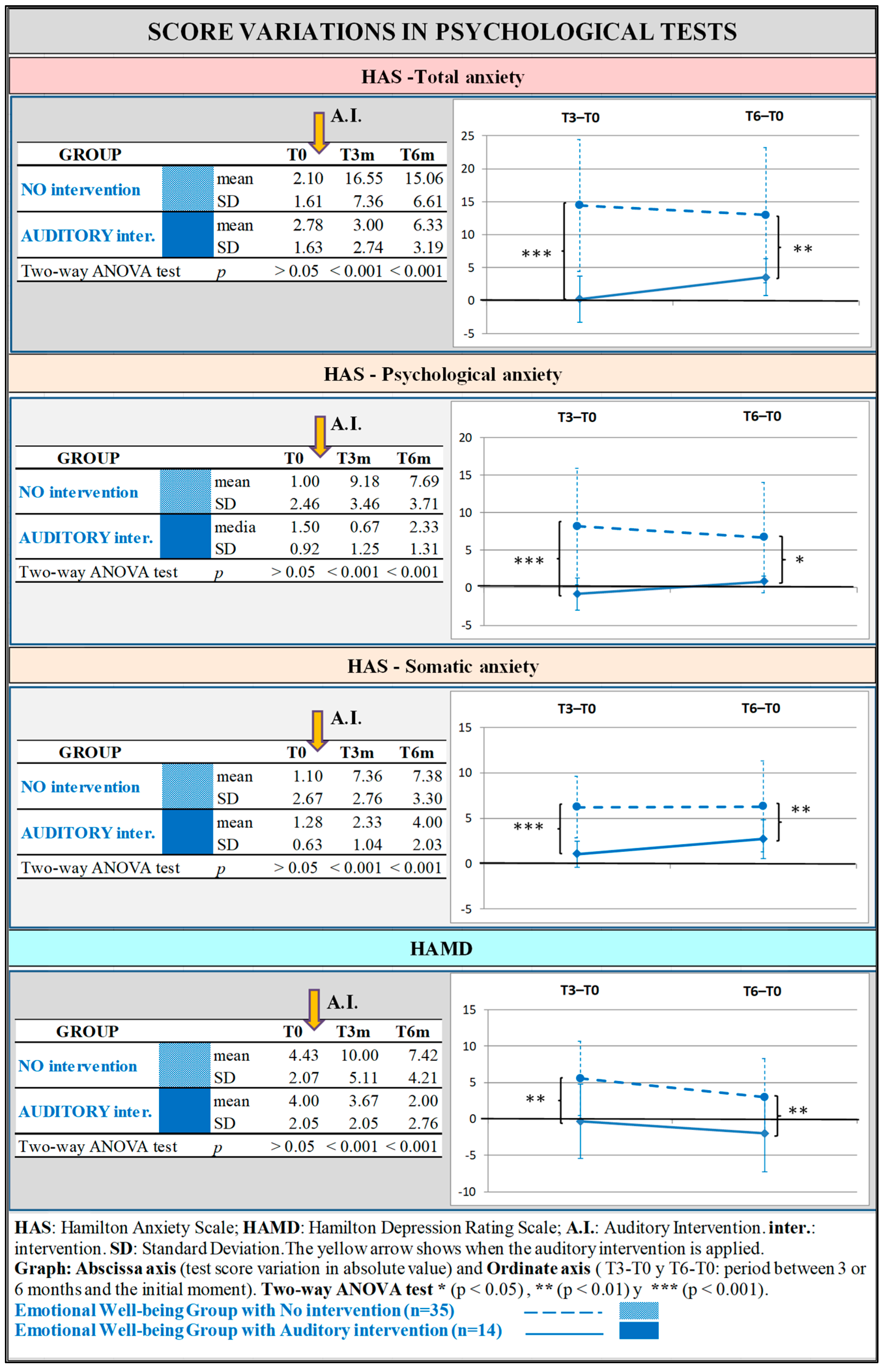
2.7.1. Hamilton Anxiety Scale—Total Anxiety
2.7.2. Hamilton Anxiety Scale—Psychological Anxiety
2.7.3. Hamilton Anxiety Scale—Somatic Anxiety
2.7.4. Hamilton Depression Scale
2.7.5. Sociodemographic Variables
2.8. Response Quantification
2.9. Statistical Analysis
3. Results
3.1. Demographic and Health Characteristics According to the Intervention Group
3.2. Internal Consistency of the Psychometric Scales
3.3. Effect of Hearing Intervention on Anxiety and Depression in the Two Emotional Groups
3.3.1. Comparison of Means at Different Time Milestones
3.3.2. Response to Treatment
3.3.3. Standardized Mean Difference
3.3.4. Epidemiological Factors Associated with a Better Response After Auditory Intervention
3.3.5. Adverse Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Mental Disorders Collaborators Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [CrossRef] [PubMed]
- WHO. Comprehensive Mental Health Action Plan 2013–2030, 1st ed.; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-003102-9. [Google Scholar]
- COVID-19 Mental Disorders Collaborators Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet Lond. Engl. 2021, 398, 1700–1712. [CrossRef]
- la Torre, J.A.; Vilagut, G.; Ronaldson, A.; Serrano-Blanco, A.; Martín, V.; Peters, M.; Valderas, J.M.; Dregan, A.; Alonso, J. Prevalence and Variability of Current Depressive Disorder in 27 European Countries: A Population-Based Study. Lancet Public Health 2021, 6, e729–e738. [Google Scholar] [CrossRef] [PubMed]
- Ghebreyesus, T.A.; Fore, H.; Birtanov, Y.; Jakab, Z. Primary Health Care for the 21st Century, Universal Health Coverage, and the Sustainable Development Goals. Lancet 2018, 392, 1371–1372. [Google Scholar] [CrossRef] [PubMed]
- Koppner, J.; Chatziarzenis, M.; Faresjö, T.; Theodorsson, E.; Thorsell, A.; Nilsson, S.; Olsen, O.; Faresjö, Å. Stress and Perceived Health among Primary Care Visitors in Two Corners of Europe: Scandinavia and Greece. Int. J. Health Geogr. 2020, 19, 55. [Google Scholar] [CrossRef]
- Ruiz-Rodríguez, P.; Cano-Vindel, A.; Muñoz Navarro, R.; Medrano, L.; Moriana, J.A.; Buiza Aguado, C.; Jiménez Cabré, G.; González-Blanch, C. Impacto económico y carga de los trastornos mentales comunes en España: Una revisión sistemática y crítica. Ansiedad Estrés 2017, 23, 118–123. [Google Scholar] [CrossRef]
- Reneses, B.; Garrido, S.; Navalón, A.; Martín, O.; Ramos, I.; Fuentes, M.; Moreno, J.; López-Ibor, J.J. Psychiatric Morbidity and Predisposing Factors in a Primary Care Population in Madrid. Int. J. Soc. Psychiatry 2015, 61, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Wiegner, L.; Hange, D.; Björkelund, C.; Ahlborg, G. Prevalence of Perceived Stress and Associations to Symptoms of Exhaustion, Depression and Anxiety in a Working Age Population Seeking Primary Care--an Observational Study. BMC Fam. Pract. 2015, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Generalised Anxiety Disorder and Panic Disorder in Adults: Management; National Institute for Health and Care Excellence: Guidelines; National Institute for Health and Care Excellence (NICE): London, UK, 2019; ISBN 978-1-4731-2854-5.
- Rodríguez Tejada, A.; Torres Tejera, M.E. Estrategias no farmacológicas en el tratamiento de la ansiedad. Aten. Primaria Práctica 2024, 6, 100193. [Google Scholar] [CrossRef]
- Miró Barrachina, M.T.; Perestelo Pérez, L.; Pérez Ramos, J.; Rivero Santana, A.; González Lorenzo, M.; de la Fuente Portero, J.A.; Serrano Castro, P.J. Eficacia de los tratamientos psicológicos basados en mindfulness para los trastornos de ansiedad y depresión: Una revisión sistemática. Rev. Psicopatol. Psicol. Clín. 2011, 16, 1–14. [Google Scholar]
- Larun, L.; Nordheim, L.V.; Ekeland, E.; Hagen, K.B.; Heian, F. Exercise in Prevention and Treatment of Anxiety and Depression among Children and Young People. Cochrane Database Syst. Rev. 2006, 3, CD004691. [Google Scholar] [CrossRef] [PubMed]
- Mera-Posligua, M.; Arredondo-Aldana, K.; Ponce Alencastro, J. Trastorno de Ansiedad Generalizada Abordado Desde La Terapia de Aceptación y Compromiso: Caso Clínico. Rev. Científica Arbitr. Investig. Salud GESTAR 2021, 4, 73–85. [Google Scholar] [CrossRef]
- Zaatar, M.T.; Alhakim, K.; Enayeh, M.; Tamer, R. The Transformative Power of Music: Insights into Neuroplasticity, Health, and Disease. Brain Behav. Immun.—Health 2024, 35, 100716. [Google Scholar] [CrossRef] [PubMed]
- Kushner, M.G.; Maurer, E.W.; Thuras, P.; Donahue, C.; Frye, B.; Menary, K.R.; Hobbs, J.; Haeny, A.M.; Van Demark, J. Hybrid Cognitive Behavioral Therapy versus Relaxation Training for Co-Occurring Anxiety and Alcohol Disorder: A Randomized Clinical Trial. J. Consult. Clin. Psychol. 2013, 81, 429–442. [Google Scholar] [CrossRef] [PubMed]
- Depression in Adults: Treatment and Management; National Institute for Health and Care Excellence: Guidelines; National Institute for Health and Care Excellence (NICE): London, UK, 2022; ISBN 978-1-4731-4622-8.
- Grupo de Trabajo de Revisión de la Guía de Práctica Clínica Sobre el Manejo de la Depresión en el Adulto 2014. Revisión de la Guía de Práctica Clínica Sobre el Manejo de la Depresión en el Adulto (2014) del Programa de GPC en el SNS; Ministerio de Sanidad, Agencia Gallega para la Gestión del Conocimiento en Salud, ACIS, Unidad de Asesoramiento Científico-Técnico, Avalia-t: Santiago de Compostela, Spain, 2023; Guías de Práctica Clínica en el SNS. [Google Scholar]
- Farah, W.H.; Alsawas, M.; Mainou, M.; Alahdab, F.; Farah, M.H.; Ahmed, A.T.; Mohamed, E.A.; Almasri, J.; Gionfriddo, M.R.; Castaneda-Guarderas, A.; et al. Non-Pharmacological Treatment of Depression: A Systematic Review and Evidence Map. Evid. Based Med. 2016, 21, 214–221. [Google Scholar] [CrossRef]
- Golden, T.L.; Springs, S.; Kimmel, H.J.; Gupta, S.; Tiedemann, A.; Sandu, C.C.; Magsamen, S. The Use of Music in the Treatment and Management of Serious Mental Illness: A Global Scoping Review of the Literature. Front. Psychol. 2021, 12, 649840. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.G.; Iversen, J.R.; Kao, M.H.; Loui, P.; Patel, A.D.; Zatorre, R.J.; Edwards, E. Music and Brain Circuitry: Strategies for Strengthening Evidence-Based Research for Music-Based Interventions. J. Neurosci. 2022, 42, 8498–8507. [Google Scholar] [CrossRef]
- Guest, M.; Boggess, M.; D’Este, C.; Attia, J.; Brown, A. An Observed Relationship between Vestibular Function and Auditory Thresholds in Aircraft-Maintenance Workers. J. Occup. Environ. Med. Am. Coll. Occup. Environ. Med. 2011, 53, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Estalayo-Gutiérrez, B.; Álvarez-Pasquín, M.J.; Germain, F. Modulation of Auditory Perception Laterality under Anxiety and Depression Conditions. Symmetry 2022, 14, 24. [Google Scholar] [CrossRef]
- Yovell, Y.; Sackeim, H.A.; Epstein, D.G.; Prudic, J.; Devanand, D.P.; McElhiney, M.C.; Settembrino, J.M.; Bruder, G.E. Hearing Loss and Asymmetry in Major Depression. J. Neuropsychiatry Clin. Neurosci. 1995, 7, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Estalayo-Gutiérrez, B.; Álvarez-Pasquín, M.J.; Germain, F. Modulation of Asymmetry in Auditory Perception through a Bilateral Auditory Intervention. Symmetry 2022, 14, 2490. [Google Scholar] [CrossRef]
- Bérard, G.; Brockett, S. Hearing Equals Behavior: Updated and Expanded; eBooks2go: Schaumburg, IL, USA, 2014; ISBN 978-1-61813-035-8. [Google Scholar]
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting Anxiety and Depression in General Medical Settings. BMJ 1988, 297, 897–899. [Google Scholar] [CrossRef]
- Carrobles, J.; Costa, M.; Del Ser, T.; Bartolomé, P. La Práctica de La Terapia de Conducta.; Promolibro: Valencia, CA, USA, 1986. [Google Scholar]
- Montón, C.; Pérez Echeverría, M.J.; Campos, R.; García Campayo, J.; Lobo, A. Escalas de ansiedad y depresión de Goldberg: Una guía de entrevista eficaz para la detección del malestar psíquico. Atencion Primaria Soc. Esp. Med. Fam. Comunitaria 1993, 12, 345–349. [Google Scholar]
- Ramos-Brieva, J.A.; Cordero Villafáfila, A. Validación de la versión castellana de la escala de Hamilton para la depresión. Actas Luso-Esp. Neurol. Psiquiatr. Cienc. Afines 1986, 14, 324–334. [Google Scholar] [PubMed]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016, 8, CD006911. [Google Scholar] [CrossRef] [PubMed]
- Aalbers, S.; Fusar-Poli, L.; Freeman, R.E.; Spreen, M.; Ket, J.C.; Vink, A.C.; Maratos, A.; Crawford, M.; Chen, X.-J.; Gold, C. Music Therapy for Depression. Cochrane Database Syst. Rev. 2017, 11, CD004517. [Google Scholar] [CrossRef] [PubMed]
- Woolf, S.H. The Power of Prevention and What It Requires. JAMA 2008, 299, 2437–2439. [Google Scholar] [CrossRef]
- Orueta, R.; Toledano, P.; Gómez-Calcerrada, R.M. Actualización en Medicina de Familia: Cumplimiento terapéutico. Med. Fam. SEMERGEN 2008, 34, 235–243. [Google Scholar] [CrossRef]
- Hall, J.E. Capítulo 59. Mecanismos Encefálicos Del Comportamiento y La Motivación: El Sistema Límbico y El Hipotálamo. In Guyton y Hall. Tratado de Fisiología Médica; Elsevier: Amsterdam, The Netherlands, 2016; pp. e38958–e39466. [Google Scholar]
- Sadock, V.A.; Sadock, B.J.; Ruiz, P. Comorbilidad de Los Trastornos Del Estado de Ánimo. In Kaplan & Sadock. Sinopsis de Psiquiatría; Wolters Kluwer: Barcelona, Spain, 2015; pp. e17702–e17712. [Google Scholar]
- Aragonès, E.; Piñol, J.L.; Labad, A. Comorbilidad de la depresión mayor con otros trastornos mentales comunes en pacientes de atención primaria. Aten. Primaria 2009, 41, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Franco, B.; Turabián-Fernández, J.L. ¿Es válido el abordaje ortodoxo de la depresión en atención primaria? Aten. Primaria 2006, 37, 37–39. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Salazar Fraile, J. Sempere Verdú E Malestar Emocional: Manual Práctico Para Una Respuesta En Atención Primaria; Conselleria de Sanitat: Generalitat Valenciana, Spain, 2012. [Google Scholar]
- Aragonès, E. Desacuerdos diagnósticos entre médicos generales y psiquiatras. Aten. Primaria 2008, 40, 644. [Google Scholar] [CrossRef] [PubMed]
- Sadock, V.A.; Sadock, B.J.; Ruiz, P. Anxiety Disorders. In Kaplan And Sadock’s Synopsis of Psychiatry. Behavioral Sciences/Clinical Psychiatry; Wolters Kluwer: Philadelphia, PA, USA, 2015; pp. e19290–e19567. [Google Scholar]
- Sadock, V.A.; Sadock, B.J.; Ruiz, P. Mood Disorders. In Kaplan And Sadock’s Synopsis of Psychiatry. Behavioral Sciences/Clinical Psychiatry; Wolters Kluwer: Philadelphia, PA, USA, 2015; pp. e17600–e19258. [Google Scholar]
- Kim, T.J.; von dem Knesebeck, O. Is an Insecure Job Better for Health than Having No Job at All? A Systematic Review of Studies Investigating the Health-Related Risks of Both Job Insecurity and Unemployment. BMC Public Health 2015, 15, 985. [Google Scholar] [CrossRef]
- Deniel Rosanas, J.; Bosch Molas, M.; Culí Borràs, N.; Olmeda Brea, C. Influencia del paro sobre los problemas de salud men-tal. Aten. Primaria 1996, 18, 379–382. [Google Scholar] [PubMed]
- Haro, J.M.; Palacín, C.; Vilagut, G.; Martínez, M.; Bernal, M.; Luque, I.; Codony, M.; Dolz, M.; Alonso, J. Grupo ESEMeD-España Prevalencia de los trastornos mentales y factores asociados: Resultados del estudio ESEMeD-España. Med. Clin. 2006, 126, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Kyle, M.E.; Wang, J.C.; Shin, J.J. Impact of Nonaspirin Nonsteroidal Anti-Inflammatory Agents and Acetaminophen on Sensorineural Hearing Loss: A Systematic Review. Otolaryngol.–Head Neck Surg. 2015, 152, 393–409. [Google Scholar] [CrossRef] [PubMed]
- Thorp, S.L.; Suchy, T.; Vadivelu, N.; Helander, E.M.; Urman, R.D.; Kaye, A.D. Functional Connectivity Alterations: Novel Therapy and Future Implications in Chronic Pain Management. Pain Physician 2018, 21, E207–E214. [Google Scholar] [CrossRef] [PubMed]
- Sadock, V.A.; Sadock, B.J.; Ruiz, P. Capítulo 9. Trastornos de Ansiedad. In Kaplan & Sadock. Sinopsis de psiquiatría. Ciencias de la conducta/Psiquiatría Clínica; Wolters Kluwer: Barcelona, Spain, 2015; pp. e19290–e19567. [Google Scholar]
- Wittchen, H.U.; Kessler, R.C.; Pfister, H.; Lieb, M. Why Do People with Anxiety Disorders Become Depressed? A Prospective-Longitudinal Community Study. Acta Psychiatr. Scand. Suppl. 2000, 102, 14–23. [Google Scholar] [CrossRef]
- Bittner, A.; Goodwin, R.D.; Wittchen, H.-U.; Beesdo, K.; Höfler, M.; Lieb, R. What Characteristics of Primary Anxiety Disorders Predict Subsequent Major Depressive Disorder? J. Clin. Psychiatry 2004, 65, 618–626, quiz 730. [Google Scholar] [CrossRef]
- Bérard, G. Audition Égale Comportement; Maisonneuve: Sainte-Ruffine (Lorena), Brazil, 1982; ISBN 978-2-7160-0097-0. [Google Scholar]
- Sinha, Y.; Silove, N.; Wheeler, D.; Williams, K. Auditory Integration Training and Other Sound Therapies for Autism Spectrum Disorders: A Systematic Review. Arch. Dis. Child. 2006, 91, 1018–1022. [Google Scholar] [CrossRef]
- Sinha, Y.; Silove, N.; Hayen, A.; Williams, K. Auditory Integration Training and Other Sound Therapies for Autism Spectrum Disorders (ASD). Cochrane Database Syst. Rev. 2011, 12, CD003681. [Google Scholar] [CrossRef] [PubMed]

| Anxiety and/or Depression Group (n = 83) | Emotional Well-Being Group (n = 50) | |||
|---|---|---|---|---|
| Auditory Interv. (n = 31) | Non-Intervention (n = 52) | Auditory Interv. (n = 14) | Non-Intervention (n = 36) | |
| Age (years old) | 50.40 (11.30) | 42.49 (12.02) | 40.33 (22.50) | 46 (12.91) |
| Gender (female) | 23 (74.19) | 39 (75) | 5 (35.71) | 17(47.22) |
| Nationality | ||||
| Spanish | 29 (93.54) | 45 (86.53) | 14 (100) | 33 (91.66) |
| Rest of Europe | 1 (3.22) | 4 (7.69) | 0 (0) | 3 (8.33) |
| African | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Hispanic American | 1 (3.22) | 3 (5.76) | 0 (0) | 0 (0) |
| Education Level | ||||
| Without | 0 (0) | 3 (5.76) | 1 (7.14) | 0 (0) |
| Primary studies | 6 (19.35) | 27 (51.92) | 10 (71.43) | 16 (44.44) |
| Secondary studies | 0 (0) | 12 (23.07) | 0 (0) | 6 (16.66) |
| Professional training | 13 (41.93) | 7 (13.46) | 3 (21.43) | 12 (33.33) |
| University studies | 12 (38.7) | 3 (5.76) | 0 (0) | 2 (5.55) |
| Employment situation | ||||
| Student | 0 (0) | 3 (5.77) | 1 (7.14) | 0 (0) |
| Active | 7 (22.64) | 25 (48.08) | 4 (28.57) | 23 (63.88) |
| Unemployed | 18 (58.01) | 23 (44.23) | 8 (57.15) | 11 (30.56) |
| Retired | 6 (19.35) | 1 (1.92) | 1 (7.14) | 2 (5.56) |
| Noise exposure | ||||
| No | 28 (90.33) | 28 (53.85) | 13 (92.86) | 18 (50) |
| Yes, only in the past | 0 (0) | 15 (28.85) | 1 (7.14) | 8 (22.22) |
| Yes, currently | 3 (9.67) | 9 (17.30) | 0 (0) | 10 (27.78) |
| Use of hearing protectors | ||||
| No | 29 (93.55) | 45 (86.54) | 10 (71.43) | 31 (86.11) |
| Yes, partially | 2 (6.45) | 5 (9.62) | 4 (28.57) | 5 (13.89) |
| Yes, always | 0 (0) | 2 (3.84) | 0 (0) | 0 (0) |
| F.H. of depression | 2 (6.45) | 9 (17.3) | 1 (7.14) | 4 (11.11) |
| F.H. of early deafness | 1 (3.22) | 10 (19.23) | 1 (7.14) | 4 (11.11) |
| Right laterality | 31 (100) | 46 (88.46) | 14 (100) | 34 (94.44) |
| P.H. of significant pain | ||||
| No | 18 (58.07) | 26 (50) | 9 (64.29) | 19 (52.77) |
| Yes, only in the past | 7 (22.58) | 6 (11.54) | 5 (35,71) | 14 (38.88) |
| Yes, currently | 6 (19.35) | 20 (38.46) | 0 (0) | 3 (8.33) |
| P.H. of immunological alteration | ||||
| No | 18 (58.07) | 35 (67.30) | 9 (64.29) | 25 (69.44) |
| Yes, only in the past | 7 (22.58) | 5 (9.62) | 0 (0) | 4 (11.11) |
| Yes, currently | 6 (19.35) | 12 (23.08) | 5 (35.71) | 7 (19.45) |
| P.H. of significant ENT pathology | ||||
| No | 31 (100) | 49 (94.23) | 14 (100) | 33 (91.67) |
| Yes, only in the past | 0 (0) | 3 (5.77) | 0 (0) | 3 (8.33) |
| P.H. of mental pathology | ||||
| No | 11 (35.48) | 26 (50) | 8 (57.14) | 17 (47.22) |
| Yes, only in the past | 20 (64.52) | 20 (38.46) | 6 (42.86) | 17 (47.22) |
| Yes, currently | 0 (0) | 6 (11.53) | 0 (0) | 2 (5.56) |
| Analgesics treatment | ||||
| No | 19 (61.29) | 36 (69.23) | 13 (92.86) | 31 (86.11) |
| Yes, only in the past | 0 (0) | 2 (3.85) | 0 (0) | 2 (5.55) |
| Yes, currently | 12 (38.71) | 14 (26.92) | 1 (7.14) | 3 (8.34) |
| Immune treatment | ||||
| No | 31 (100) | 49 (94.23) | 14 (100) | 33 (91.67) |
| Yes, only in the past | 0 (0) | 0 (0) | 0 (0) | 1 (2.77) |
| Yes, currently | 0 (0) | 3 (5.77) | 0 (0) | 2 (5.55) |
| Anxiolytics treatment | ||||
| No | 18 (58.07) | 37 (71.15) | 12 (85.71) | 32 (88.88) |
| Yes, only in the past | 3 (9.68) | 3 (5.77) | 0 (0) | 2 (5.56) |
| Yes, currently | 10 (32.25) | 12 (23.08) | 2 (14.29) | 2 (5.56) |
| Antidepressants treatment | ||||
| No | 21 (67.74) | 37 (71.15) | 14 (100) | 30 (83.32) |
| Yes, only in the past | 3 (9.68) | 5 (9.62) | 0 (0) | 3 (8.34) |
| Yes, currently | 7 (22.58) | 10 (19.23) | 0 (0) | 3 (8.34) |
| Psychological treatment | ||||
| No | 25 (80.65) | 35 (67.31) | 9 (64.29) | 30 (83.33) |
| Yes, only in the past | 6 (19.35) | 11 (21.15) | 5 (35.71) | 6 (16.66) |
| Yes, currently | 0 (0) | 6 (11.54) | 0 (0) | 0 (0) |
| Taste in music | ||||
| No | 0 (0) | 10 (19.23) | 0 (0) | 4 (11.11) |
| Yes, listening to it regularly | 24 (77.42) | 30 (57.69) | 10 (71.43) | 22 (61.11) |
| Yes, but not listening to it regularly | 7 (22.58) | 12 (23.08) | 4 (28.57) | 10 (27.78) |
| Groups | TOTAL Response to: | PARTIAL Response to: |
|---|---|---|
| Emotional Well-being Group | HAS-Psychological at 3 months HAMD at 6 months | |
| Anxiety and/or Depression Group | HAS-Total at 3 months HAS-Psychological at 3 months HAS-Somatic at 3 months | HAS-Total at 6 months HAS-Somatic at 6 months HAMD at 3 months HAMD at 6 months |
| T3m | T6m | |||
|---|---|---|---|---|
| HAS-Total | HAMD | HAS-Total | HAMD | |
| Emotional Well-being groups with and without auditory intervention. | −1.16 | −0.74 | −0.68 | −0.51 |
| Anxiety and/or Depression groups with and without auditory intervention. | −0.20 | −0.09 | −0.01 | −0.02 |
| After 3 Months | After 6 Months | |
|---|---|---|
| HAS: Psychol. Anxiety | ||
| (Ω) | No findings | No findings |
| HAS: Somatic Anxiety | ||
| (Ω) | No findings | No findings |
| HAS: Total Anxiety (*) | ||
| Group without Intervention | ||
| Better results | Having university studies compared to the rest of studies variables. | |
| Worse results | Range 51–65 years old. Being retired. History of pain. History of mental pathology. Having taken antidepressants in the past. Having taken analgesics in the past. Having followed psychological treatment in the past. Being retired. | Family history of depression. |
| Group with Auditory Intervention | ||
| Better results | Being unemployed is better than working for someone else. | Age range 31–50 years old better than 51–65 years old. |
| Worse results | Having taken anti-anxiety or antidepressants in the past. | Having basic studies is worse than the rest of studies variables. Having taken anti-anxiety or antidepressants in the past. |
| HAMD (*) | ||
| Group without Intervention | ||
| Better results | ||
| Worse results | History of chronic pain. Having taken analgesics in the past. Having followed psychological treatment in the past. Being retired. | |
| Group with Auditory Intervention | ||
| Better results | Being unemployed is better than working for someone else. | |
| Worse results | The current history of mental pathology presents a worse outcome than having had it in the past or not having had it at all. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Estalayo-Gutiérrez, B.; Álvarez Pasquín, M.J.; Germain, F. Approach to Mental Health Through a Frequency Modulated Auditory Intervention: A Controlled and Randomized Clinical Trial. J. Clin. Med. 2025, 14, 288. https://doi.org/10.3390/jcm14010288
Estalayo-Gutiérrez B, Álvarez Pasquín MJ, Germain F. Approach to Mental Health Through a Frequency Modulated Auditory Intervention: A Controlled and Randomized Clinical Trial. Journal of Clinical Medicine. 2025; 14(1):288. https://doi.org/10.3390/jcm14010288
Chicago/Turabian StyleEstalayo-Gutiérrez, Beatriz, María José Álvarez Pasquín, and Francisco Germain. 2025. "Approach to Mental Health Through a Frequency Modulated Auditory Intervention: A Controlled and Randomized Clinical Trial" Journal of Clinical Medicine 14, no. 1: 288. https://doi.org/10.3390/jcm14010288
APA StyleEstalayo-Gutiérrez, B., Álvarez Pasquín, M. J., & Germain, F. (2025). Approach to Mental Health Through a Frequency Modulated Auditory Intervention: A Controlled and Randomized Clinical Trial. Journal of Clinical Medicine, 14(1), 288. https://doi.org/10.3390/jcm14010288







