Effects of Hippotherapy and Horse-Riding Simulators on Gross Motor Function in Children with Cerebral Palsy: A Systematic Review
Abstract
1. Introduction
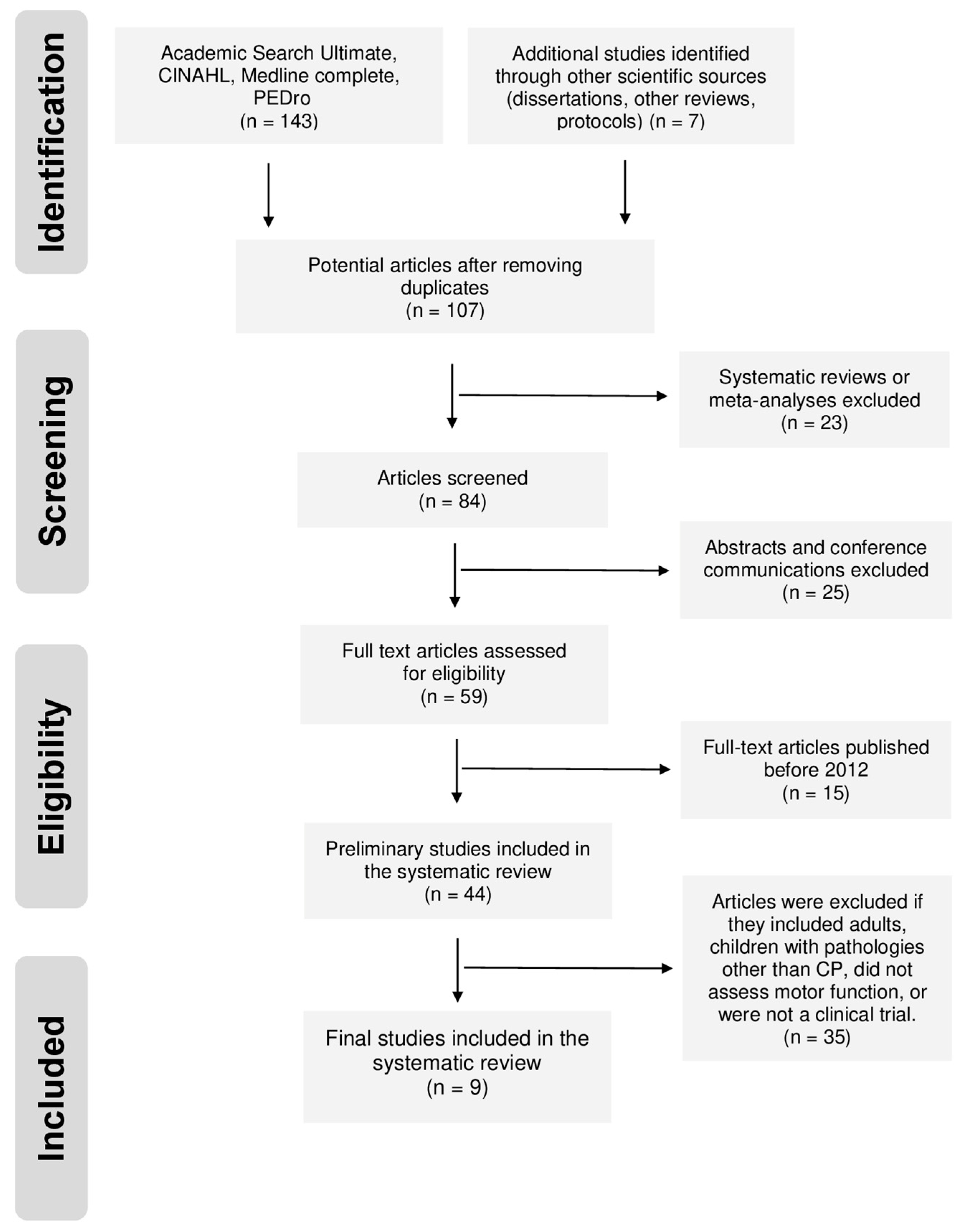
2. Materials and Methods
2.1. Search Strategy
2.2. Selection of Studies
2.2.1. Types of Studies
2.2.2. Type of Participants
2.2.3. Data Extraction
2.3. Quality of Studies
3. Results
3.1. Selection of Studies
3.2. Characteristics of the Studies
3.3. Quality of Studies
3.4. Data from Studies
3.4.1. Measurement of Variables
3.4.2. Characteristics of the Interventions
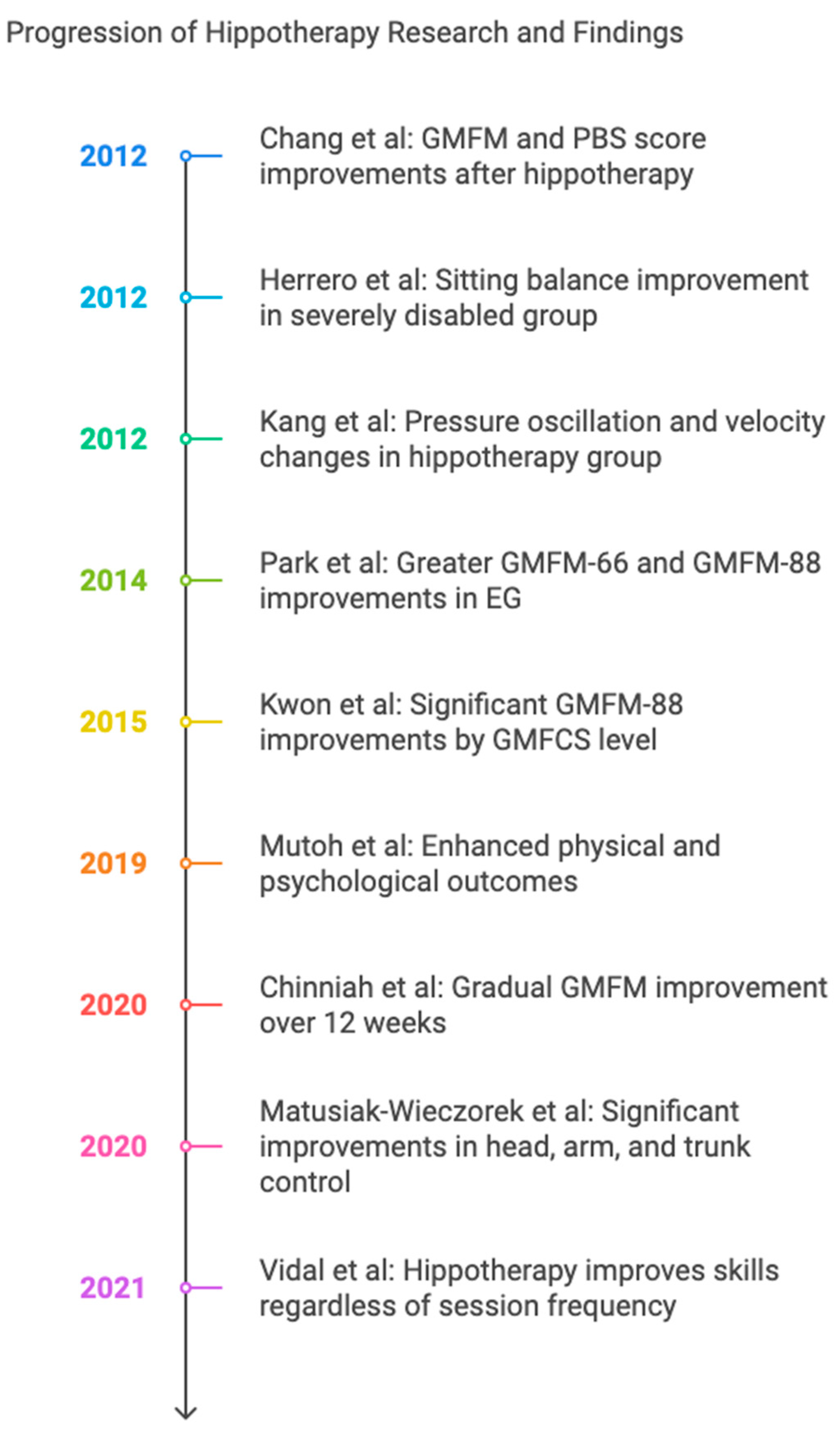
3.4.3. Effects of Hippotherapy
4. Discussion
Applications for Clinical Practice and Future Research Lines
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abuin-Porras, V.; Pedersini, P.; Berjano, P.; Villafañe, J.H. The efficacy of physical therapy on the improvement of the motor components of visual attention in children with cerebral palsy: A case series study. J. Exerc. Rehabil. 2019, 15, 103. [Google Scholar] [CrossRef]
- Longo, E.; Regalado, I.C.R.; Galvão, E.R.V.P.; Ferreira, H.N.C.; Badia, M.; Baz, B.O. I Want to play: Children with cerebral palsy talk about their experiences on barriers and facilitators to participation in leisure activities. Pediatr. Phys. Ther. 2020, 32, 190–200. [Google Scholar] [CrossRef]
- Stavsky, M.; Mor, O.; Mastrolia, S.A.; Greenbaum, S.; Than, N.G.; Erez, O. Cerebral palsy—Trends in epidemiology and recent development in prenatal mechanisms of disease, treatment, and prevention. Front. Pediatr. 2017, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Korzeniewski, S.J.; Slaughter, J.; Lenski, M.; Haak, P.; Paneth, N. The complex aetiology of cerebral palsy. Nat. Rev. Neurol. 2018, 14, 528–543. [Google Scholar] [CrossRef]
- Michael-Asalu, A.; Taylor, G.; Campbell, H.; Lelea, L.L.; Kirby, R.S. Cerebral palsy: Diagnosis, epidemiology, genetics, and clinical update. Adv. Pediatr. 2019, 66, 189–208. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Escolano-Pérez, E.; Herrero-Nivela, M.L.; Losada, J.L. Association between preschoolers’ specific fine (but not gross) motor skills and later academic competencies: Educational implications. Front. Psychol. 2020, 11, 1044. [Google Scholar] [CrossRef] [PubMed]
- Pillastrini, P.; Ferrari, S.; Rattin, S.; Cupello, A.; Villafañe, J.H.; Vanti, C. Exercise and tropism of the multifidus muscle in low back pain: A short review. J. Phys. Ther. Sci. 2015, 27, 943–945. [Google Scholar] [CrossRef] [PubMed]
- Paulson, A.; Vargus-Adams, J. Overview of four functional classification systems commonly used in cerebral palsy. Children 2017, 4, 30. [Google Scholar] [CrossRef]
- De Guindos-Sanchez, L.; Lucena-Anton, D.; Moral-Munoz, J.A.; Salazar, A.; Carmona-Barrientos, I. The effectiveness of hippotherapy to recover gross motor function in children with cerebral palsy: A systematic review and meta-analysis. Children 2020, 7, 106. [Google Scholar] [CrossRef]
- Moraes, A.G.; Copetti, F.; Angelo, V.R.; Chiavoloni, L.L.; David, A.C. The effects of hippotherapy on postural balance and functional ability in children with cerebral palsy. J. Phys. Ther. Sci. 2016, 28, 2220–2226. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Romero, J.G.; Molina-Aroca, A.; Moral-Munoz, J.A.; Luque-Moreno, C.; Lucena-Anton, D. Effectiveness of mechanical horse-riding simulators on postural balance in neurological rehabilitation: Systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 165. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.; Popat, H.; et al. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed]
- Hariohm, K.; Prakash, V.; Saravankumar, J. Quantity and quality of randomized controlled trials published by Indian physiotherapists. Perspect. Clin. Res. 2015, 6, 91. [Google Scholar] [CrossRef]
- Chinniah, H.; Natarajan, M.; Ramanathan, R.; Ambrose, J.W.F. Effects of horse riding simulator on sitting motor function in children with spastic cerebral palsy. Physiother. Res. Int. 2020, 25, e1870. [Google Scholar] [CrossRef] [PubMed]
- Herrero, P.; Gómez-Trullén, E.M.; Asensio, Á.; García, E.; Casas, R.; Monserrat, E.; Pandyan, A. Study of the therapeutic effects of a hippotherapy simulator in children with cerebral palsy: A stratified single-blind randomized controlled trial. Clin. Rehabil. 2012, 26, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Matusiak-Wieczorek, E.; Dziankowska-Zaborszczyk, E.; Synder, M.; Borowski, A. The influence of hippotherapy on the body posture in a sitting position among children with cerebral palsy. Int. J. Environ. Res. Public Health 2020, 17, 6846. [Google Scholar] [CrossRef]
- Mutoh, T.; Mutoh, T.; Tsubone, H.; Takada, M.; Doumura, M.; Ihara, M.; Shimomura, H.; Taki, Y.; Ihara, M. Impact of long-term hippotherapy on the walking ability of children with cerebral palsy and quality of life of their caregivers. Front. Neurol. 2019, 10, 834. [Google Scholar] [CrossRef]
- Vidal, A.; de Azevedo Fernandes, J.M.G.; da Rosa Gutierres, I.C.; da Silva, F.C.; Silva, R.; Gutierres Filho, P.J.B. Effects of weekly hippotherapy frequency on gross motor function and functional performance of children with cerebral palsy: A randomized controlled trial. Motricidade 2021, 17, 79–86. [Google Scholar]
- Kwon, J.Y.; Chang, H.J.; Yi, S.H.; Lee, J.Y.; Shin, H.Y.; Kim, Y.H. Effect of hippotherapy on gross motor function in children with cerebral palsy: A randomized controlled trial. J. Altern. Complement. Med. 2015, 21, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Park, E.S.; Rha, D.W.; Shin, J.S.; Kim, S.; Jung, S. Effects of hippotherapy on gross motor function and functional performance of children with cerebral palsy. Yonsei Med. J. 2014, 55, 1736–1742. [Google Scholar] [CrossRef]
- Chang, H.J.; Kwon, J.Y.; Lee, J.Y.; Kim, Y.H. The effects of hippotherapy on the motor function of children with spastic bilateral cerebral palsy. J. Phys. Ther. Sci. 2012, 24, 1277–1280. [Google Scholar] [CrossRef][Green Version]
- Kang, H.; Jung, J.; Yu, J. Effects of hippotherapy on the sitting balance of children with cerebral palsy: A randomized control trial. J. Phys. Ther. Sci. 2012, 24, 833–836. [Google Scholar] [CrossRef]
- Park, E.Y. Gross motor function and activities of daily living in children and adolescents with cerebral palsy: A longitudinal study. J. Dev. Phys. Disabil. 2018, 30, 189–203. [Google Scholar] [CrossRef]
- Menor-Rodríguez, M.J.; Sevilla Martín, M.; Sánchez-García, J.C.; Montiel-Troya, M.; Cortés-Martín, J.; Rodríguez-Blanque, R. Role and Effects of Hippotherapy in the Treatment of Children with Cerebral Palsy: A Systematic Review of the Literature. J. Clin. Med. 2021, 10, 2589. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.H.; Fields, B.E. Hippotherapy: A systematic mapping review of peer-reviewed research, 1980 to 2018. Disabil. Rehabil. 2021, 43, 1463–1487. [Google Scholar] [CrossRef]
- Jonsson, U.; Eek, M.N.; Sunnerhagen, K.S.; Himmelmann, K. Cerebral palsy prevalence, subtypes, and associated impairments: A population-based comparison study of adults and children. Dev. Med. Child Neurol. 2019, 61, 1162–1167. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, M.; Sarecka-Hujar, B.; Kopyta, I. Cerebral palsy: Current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr. Dis. Treat. 2020, 16, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Noble, J.J.; Gough, M.; Shortland, A.P. Selective motor control and gross motor function in bilateral spastic cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Hyun, C.; Kim, K.; Lee, S.; Ko, N.; Lee, I.S.; Koh, S.E. The short-term effects of hippotherapy and therapeutic horseback riding on spasticity in children with cerebral palsy: A meta-analysis. Pediatr. Phys. Ther. 2022, 34, 172. [Google Scholar] [CrossRef] [PubMed]
- Stergiou, A.; Tzoufi, M.; Ntzani, E.; Varvarousis, D.; Beris, A.; Ploumis, A. Therapeutic effects of horseback riding interventions: A systematic review and meta-analysis. Am. J. Phys. Med. Rehabil. 2017, 96, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Mi, Y.S.; Young, L.J.; Yeon, S.H.; Sik, S.Y.; Yi, K.J. Factors influencing motor outcome of hippotherapy in children with cerebral palsy. Neuropediatrics 2019, 50, 170–177. [Google Scholar]
| Author and Year | Location of Study | Aim of the Study | Study Design | Population |
|---|---|---|---|---|
| Chang et al., 2012 [22] | South Korea | To investigate whether hippotherapy could improve the functional performance of preschool- and school-aged children with spastic bilateral CP | Clinical trial | n: 33 children with CP Type of CP: spastic (quadriplegia and diplegia) Gender: 19 M/14 F Age: 6 years (Mean) GMFCS level: I–IV |
| Herrero et al., 2012 [16] | Spain | To investigate whether hippotherapy (when applied by a simulator) improves postural control and balance in children with CP | RCT | n: 38 children with CP Type of CP: not specified Gender: 24 M/14 F Age: entre 4–18 years GMFCS level: I–V |
| Kang et al., 2012 [23] | South Korea | To verify the effect of hippotherapy on the sitting balance of children with severe CP by comparing hippotherapy, physical therapy, and a control | RCT | n: 43 children with CP Type of CP: spastic (hemiplegia and diplegia) Gender: 22 M/21 F Age: 8 years (Mean) GMFCS level: not specified |
| Park et al., 2014 [21] | South Korea | To investigate the effects of hippotherapy on gross motor function and functional performance in children with spastic CP | RCT | n: 55 children with CP Type of CP: spastic (bilateral -most frequent- and unilateral) Gender: 25 M/30 F Age: between 3–12 years GMFCS level: I–IV |
| Kwon et al., 2015 [20] | South Korea | To examine whether hippotherapy has a clinically significant effect on gross motor function in children with CP | RCT | n: 91 children with CP Type of CP: spastic (most frequent), dyskinetic and ataxic Gender: 49 M/42 F Age: between 4–10 years GMFCS level: I–IV |
| Mutoh et al., 2019 [18] | Japan | To determine how hippotherapy affects the gross motor and gait functions in children with CP and how it may also impact the quality of life of patients’ caregivers | RCT | n: 24 children with CP Type of CP: spastic (bilateral -diplegia-) Gender: 11 M/13 F Age: entre 4–14 years GMFCS level: II–III |
| Chinniah et al., 2020 [15] | India | To investigate the therapeutic effects of horse-riding simulator on sitting motor function in children with spastic diplegia | RCT | n: 30 children with CP Type of CP: spastic (diplegia) Gender: 13 M/17 F Age: between 2–4 years GMFCS level: I–III |
| Matusiak-Wieczorek et al., 2020 [17] | Poland | To assess the influence of hippotherapy on posture and body function among children with CP | RCT | n: 45 children with CP Type of CP: spastic (diplegia and hemiplegia -most frequent-) Gender: 25 M/20 F Age: between 6–12 years GMFCS level: I–II |
| Vidal et al., 2021 [19] | Brazil | To verify whether hippotherapy once or twice a week has a different effect on gross motor function and functional performance in children with CP | RCT | n: 20 children with CP Type of CP: not specified Gender: 12 M/8 F Age: between 2–5 years and 11 months GMFCS level: II–V |
| Study | C1 * | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chang et al., 2012 [22] | 1 * | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 5/10 |
| Herrero et al., 2012 [16] | 0 * | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7/10 |
| Kang et al., 2012 [23] | 1 * | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Park et al., 2014 [21] | 1 * | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5/10 |
| Kwon et al., 2015 [20] | 1 * | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 |
| Mutoh et al., 2019 [18] | 1 * | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 7/10 |
| Chinniah et al., 2020 [15] | 1 * | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 8/10 |
| Matusiak-Wieczorek et al., 2020 [17] | 0 * | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6/10 |
| Vidal et al., 2021 [19] | 1 * | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7/10 |
| Study | Outcome Measures | Experimental Group—Control/Comparative Group | Reported Results |
|---|---|---|---|
| Chang et al., 2012 [22] | Gross motor function: GMFM-88 Balance: PBS | Group A (n = 19): GMFCS I–II Group B (n = 14): GMFCS III–IV Protocol in both groups: hippotherapy (2 sessions of 30 min · week/8 weeks) with riding specialists. The movements of each horse were modified during the treatment sessions according to the child’s needs (e.g., walking, changing rhythm or changing patterns and directions). | Results: the GMFM total score and the scores of dimensions C, D, and E increased after hippotherapy in group B (p < 0.05), while only dimension E and the GMFM total score improved in group A (p < 0.05). In both groups, the PBS score increased after hippotherapy (p < 0.01). Conclusions: hippotherapy can improve gross motor function and balance in pediatric patients with CP without adverse effects. This method is recommended for preschool- and school-aged children with spastic CP. |
| Herrero et al., 2012 [16] | Gross motor function: GMFM-66. Sitting balance: dimension B of GMFM and SAS | EG (n = 19): consisted of sitting on the hippotherapy simulator with active trunk extension while the simulator was turned on in TRAINING mode (1 session of 15 min × week/10 weeks). CG (n = 19): consisted of sitting on the hippotherapy simulator with active trunk extension while the simulator was turned off (1 session of 15 min × week/10 weeks). | Results: sitting balance (dimension B of the GMFM) improved significantly in the EG, and the effect was greater in the severely disabled group (p < 0.05). Improvements in sitting balance were not maintained over the follow-up period. In addition, changes in GMFM and SAS total score were not significant. Conclusions: simulator hippotherapy can improve sitting balance in children with CP who have higher levels of disability. |
| Kang et al., 2012 [23] | Sitting balance: Force plate | Hippotherapy group (n = 15): received hippotherapy and traditional physiotherapy (stretching program). Hippotherapy consisted of sitting and standing in the saddle, manipulating objects and maintaining posture while the horse moved (2 sessions of 30 min × week/8 weeks). Physiotherapy group (n = 14): received only traditional physiotherapy (2 sessions of 30 min × week/8 weeks). CG (n = 14): did not receive intervention. | Results: center of pressure oscillation and velocity decreased in the hippotherapy group compared to the physiotherapy group and CG (p < 0.05). The physiotherapy group showed differences in right/left trajectories and total trajectories as well as right/left velocity and final velocity compared to the CG (p < 0.05). Before and after the intervention, improvements in all variables were demonstrated in the hippotherapy group (p < 0.05). Conclusions: hippotherapy with traditional physical therapy improves sitting balance in children with severe CP (inability to walk) compared to traditional physical therapy alone. |
| Park et al., 2014 [21] | Gross motor function: GMFM-66 y GMFM-88. Functional performance: PEDI-FSS | EG (n = 34): hippotherapy was used under the direction of a specialist and a trained assistant (2 sessions of 45 min × week/8 weeks). The child sat on the horse and performed activities that emphasized forward and upward movement to promote active postural control, trunk strength, balance, and trunk-pelvic dissociation. CG (n = 21): did not receive intervention. | Results: GMFM-66 and GMFM-88 scores improved in both groups (p < 0.05). However, EG compared to CG had greater improvement in dimension E and GMFM-66 total score (p < 0.05). GMFM-88 scores improved in all dimensions in the EG, but only in dimension B in the CG (p < 0.05). The PEDI-FSS total score and its 3 domain scores improved in the EG but not in the CG (p < 0.05). Conclusions: hippotherapy produces benefits in gross motor function and functional performance in children with CP compared to CG. |
| Kwon et al., 2015 [20] | Gross motor function: GMFM-66 and GMFM-88. Balance: PBS | EG (n = 45): received hippotherapy (2 sessions of 30 min × week/8 weeks) as well as conventional physiotherapy. A protocol was used that included muscle relaxation; optimal postural alignment of the head, trunk, and lower extremities; independent sitting; and active exercises (stretching, strengthening, dynamic balance and postural control). CG (n = 46): received aerobic exercise at home, such as walking or cycling, along with conventional physiotherapy (2 sessions of 30 min × week/8 weeks). | Results: The EG, in relation to the CG, showed significant improvements in total GMFM-88, GMFM-66, and GMFM dimensions B, C, D, and E (p < 0.05). The GMFM-88 dimensions improved significantly after hippotherapy according to the GMFCS level: dimension E in level I, dimensions D and E in level II, dimensions C and D in level III, and dimensions B and C in level IV. In addition, balance in EG showed improvements in PBS (p < 0.05), while no differences were observed in CG. Conclusions: hippotherapy has a positive effect on gross motor skills and balance in children with CP of different functional levels. |
| Mutoh et al., 2019 [18] | Physical function (Gait parameters): 5-m walk test Gross motor function: GMFM-66 Quality of life (QOL) of patients’ caregivers: WHOQOL-BREF | EG (n = 12): received a hippotherapy program (1 session of 30 min × week/48 weeks) that included muscle relaxation and maintaining optimal postural alignment of the head, trunk, and lower extremities with independent active and seated exercises (stretching, strengthening, dynamic balance and postural control). A 3-month follow-up was performed at the end. CG (n = 12): received a weekly recreational program (1 session of 30 min × week/48 weeks) with leisure activities and children’s games. A 3-month follow-up was conducted at the end of the program. All children continued their daily routines for the rest of the week, but none received physical therapy during the study. | Results: In addition to better GMFM-66 (p = 0.027) and GMFM-E (p = 0.044) scores, hippotherapy was associated with increased cadence, stride length, and mean acceleration (p < 0.001); better stabilized horizontal/vertical displacement (p = 0.009); and a better relationship between caregiver psychological state and quality of life (p < 0.05) compared to CG. In the EG, the improved step length of the children and the psychological quality of life domain of their caregivers were maintained for up to 3 months of follow-up (p < 0.05) compared to the CG. Conclusions: A 1-year program of once-weekly hippotherapy can improve the walking ability of children with CP and the psychological health and quality of life of their caregivers, compared to usual daycare recreational activities. |
| Chinniah et al., 2020 [15] | Motor function in sitting Positions: GMFM-88 dimension B. Measurements were taken every 4, 8, and 12 weeks. | EG (n = 15): received conventional therapy (30 min) and hippotherapy with the simulator (15 min). In the session (3 sessions × week/12 weeks), the children were placed in the saddle and asked to maintain a sitting posture. Mechanical riding therapy produced saddle movements at 3 levels: basic conditioning (flat), forward and backward tilting, and lateral tilting. CG (n = 15): received only conventional physiotherapy based on positioning, stretching, and sitting balance activities (30 min). | Results: GMFM improved in both groups over a period of 12 weeks. Sitting motor function improved gradually over time in both groups. The EG showed a greater improvement in relation to the CG at all weeks (p < 0.01). Conclusions: an improvement in sitting motor function was observed in both groups, although the children exposed to the simulator showed a greater improvement. The riding simulator was effective in improving sitting motor function in children with diplegia, and its administration for a longer duration provided more benefit than when used for a shorter duration. |
| Matusiak-Wieczorek et al., 2020 [17] | Posture and function of each part of the body: SAS | EG 1 (n = 15): 2 sessions of 30 min · week/12 weeks. EG 2 (n = 15): 1 session of 30 min · week/12 weeks. Program in EG 1 and EG 2: tasks when the horse is standing and then in motion, based on leaning forward and touching the horse’s right ear with the left hand (and vice versa), lifting the straight upper limbs forward, moving sideways and turning the trunk to the right and left, and placing the hands on the back of the head (with elbows apart) to maintain this position throughout the turn. CG (n = 15): did not receive intervention. | Results: improvements were seen in almost all categories evaluated in the children who participated in hippotherapy. In EG 1, statistically significant differences were observed in the assessment of head position control (p = 0.012), arm function (p = 0.012), and trunk control (p = 0.005), while in EG 2, improvements were observed in the assessment of trunk control (p = 0.028). Conclusions: hippotherapy has a positive effect on the posture and function of individual body parts in the seated position in children with CP. |
| Vidal et al., 2021 [19] | Gross motor function: GMFM–66 Functional performance: PEDI | Group 1 (n = 9): 1 session of 30–35 min × week/16 weeks. Group 2 (n = 11): 2 sessions of 30–35 min × week/16 weeks. Group 1 and 2: Children wore a protective helmet, sat on the horse, and performed activities to improve forward and upward movement to stimulate postural control, head, trunk, and pelvic movements, strength, and coordination. Activities were performed in sand and outdoor arenas, on tarmac and grass, on different slopes, and in different postures such as classical, lateral, inverted, or quadruped. | Results: A significant effect was observed in the measures for both groups before and after the evaluation (p < 0.05), although no significant differences were reflected when comparing the two groups (p > 0.05). Hippotherapy improved gross motor skills and functional performance in children with CP regardless of the frequency of weekly sessions. Conclusions: Significant benefits of hippotherapy were demonstrated in GMFM-66 and PEDI in children with CP; however, a greater effect was observed with twice-weekly treatment. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortega-Cruz, A.; Sánchez-Silverio, V.; Riquelme-Aguado, V.; Alonso-Perez, J.L.; Abuín-Porras, V.; Villafañe, J.H. Effects of Hippotherapy and Horse-Riding Simulators on Gross Motor Function in Children with Cerebral Palsy: A Systematic Review. J. Clin. Med. 2025, 14, 283. https://doi.org/10.3390/jcm14010283
Ortega-Cruz A, Sánchez-Silverio V, Riquelme-Aguado V, Alonso-Perez JL, Abuín-Porras V, Villafañe JH. Effects of Hippotherapy and Horse-Riding Simulators on Gross Motor Function in Children with Cerebral Palsy: A Systematic Review. Journal of Clinical Medicine. 2025; 14(1):283. https://doi.org/10.3390/jcm14010283
Chicago/Turabian StyleOrtega-Cruz, Antonio, Víctor Sánchez-Silverio, Víctor Riquelme-Aguado, Jose Luis Alonso-Perez, Vanesa Abuín-Porras, and Jorge Hugo Villafañe. 2025. "Effects of Hippotherapy and Horse-Riding Simulators on Gross Motor Function in Children with Cerebral Palsy: A Systematic Review" Journal of Clinical Medicine 14, no. 1: 283. https://doi.org/10.3390/jcm14010283
APA StyleOrtega-Cruz, A., Sánchez-Silverio, V., Riquelme-Aguado, V., Alonso-Perez, J. L., Abuín-Porras, V., & Villafañe, J. H. (2025). Effects of Hippotherapy and Horse-Riding Simulators on Gross Motor Function in Children with Cerebral Palsy: A Systematic Review. Journal of Clinical Medicine, 14(1), 283. https://doi.org/10.3390/jcm14010283