Early Cardiac Evaluation, Abnormal Test Results, and Associations with Outcomes in Patients with Acute Brain Injury Admitted to a Neurocritical Care Unit
Abstract
1. Introduction
2. Materials and Methods
2.1. Institutional Review Board Approval
2.2. Study Design, Participants, and Clinical Setting
2.3. Data Collection
2.4. Definition of Cardiac Abnormalities
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
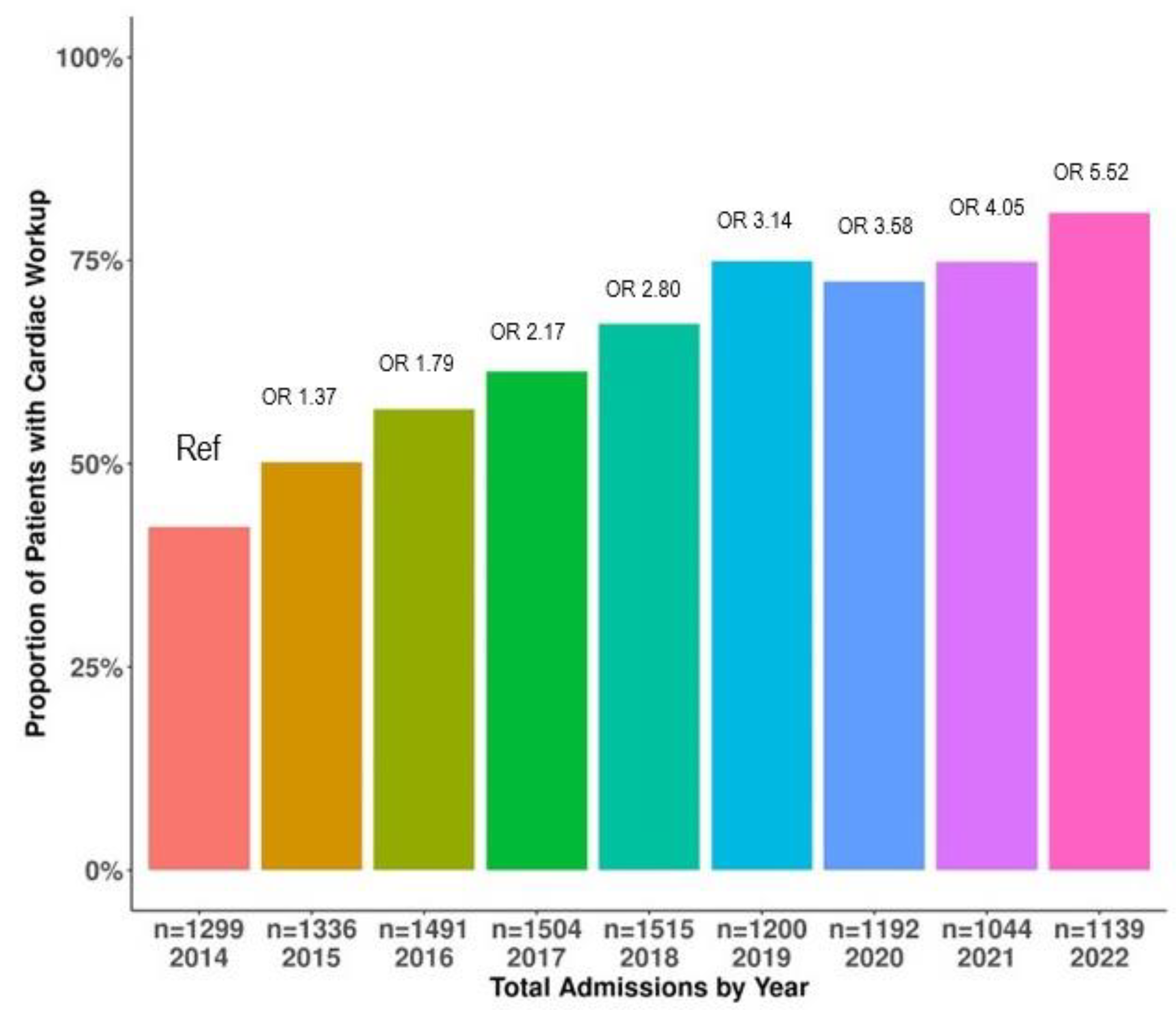
3.2. Trends in Cardiac Evaluation over the Study Period
3.3. Figure 2 Demonstrates the Trends in the Type of Cardiac Evaluation amongst ABI Types over the Study Period

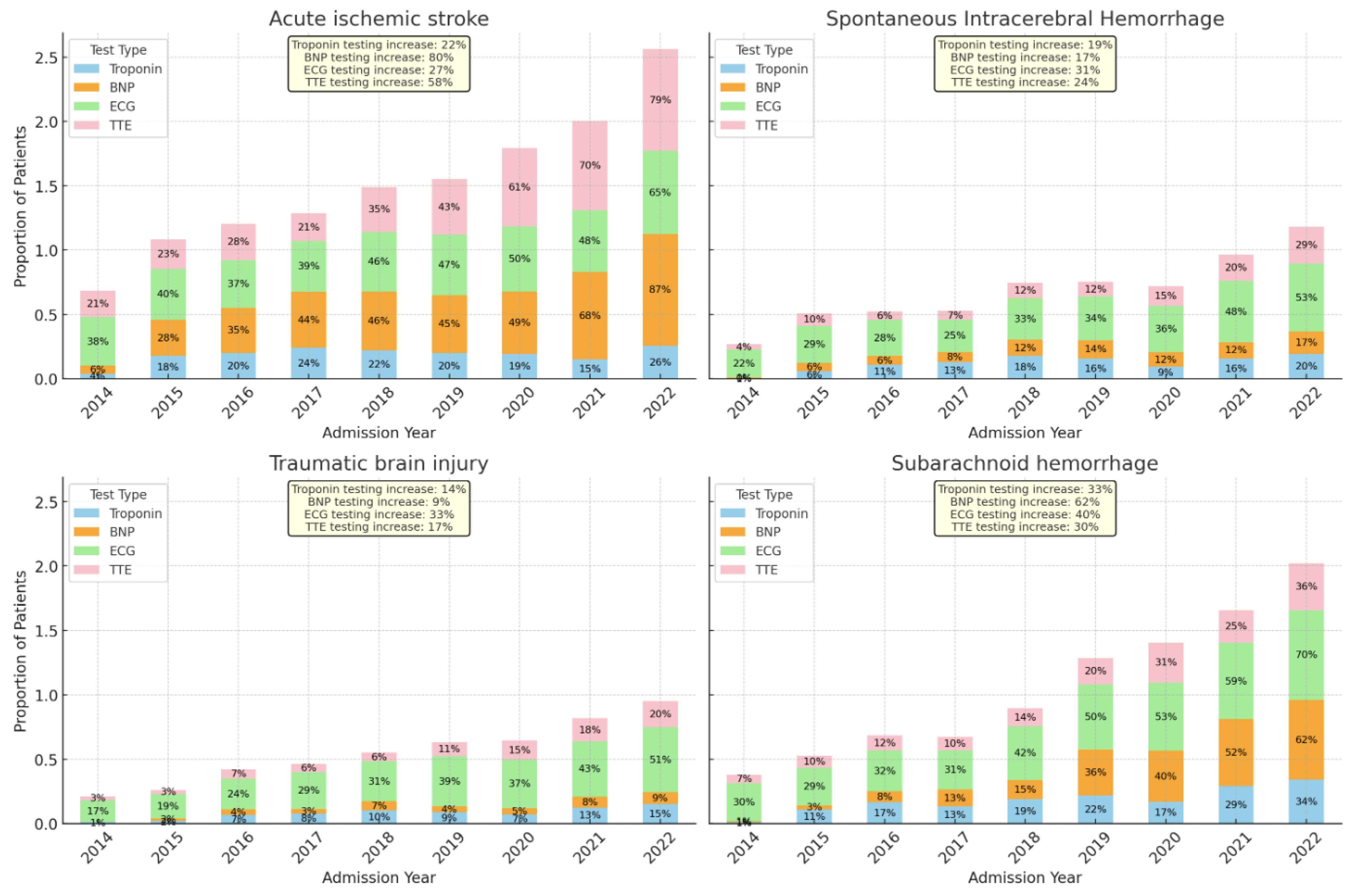
3.4. Trends in Specific Type of Cardiac Testing Stratified by ABI Type
3.4.1. Acute Ischemic Stroke and Cardiac Evaluation
3.4.2. Spontaneous Intracerebral Hemorrhage and Cardiac Evaluation
3.4.3. Spontaneous Subarachnoid Hemorrhage and Cardiac Evaluation
3.4.4. Traumatic Brain Injury and Cardiac Evaluation
3.5. Factors Associated with Cardiac Evaluation in ABI
3.6. Individual Cardiac Testing in ABI
3.7. Cardiovascular Test Abnormalities and Outcomes
3.7.1. Prevalence of Cardiovascular Test Abnormalities
3.7.2. Associations between Cardiovascular Test Abnormalities and Outcomes
3.8. Exploring the Association between cTnI, BNP, and EF < 40%
4. Discussion
Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suarez, J.I.; Martin, R.H.; Bauza, C.; Georgiadis, A.; Venkatasubba Rao, C.P.; Calvillo, E.; Hemphill, J.C., 3rd; Sung, G.; Oddo, M.; Taccone, F.S.; et al. Worldwide Organization of Neurocritical Care: Results from the PRINCE Study Part 1. Neurocrit. Care 2019, 32, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Venkatasubba Rao, C.P.; Suarez, J.I.; Martin, R.H.; Bauza, C.; Georgiadis, A.; Calvillo, E.; Hemphill, J.C., 3rd; Sung, G.; Oddo, M.; Taccone, F.S.; et al. Global Survey of Outcomes of Neurocritical Care Patients: Analysis of the PRINCE Study Part 2. Neurocrit. Care 2020, 32, 88–103. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, V.; Mackensen, G.B.; Gibbons, E.F.; Vavilala, M.S. Cardiac Dysfunction after Neurologic Injury: What Do We Know and Where Are We Going? Chest 2016, 149, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Sposato, L.A.; Hilz, M.J.; Aspberg, S.; Murthy, S.B.; Bahit, M.C.; Hsieh, C.-Y.; Sheppard, M.N.; Scheitz, J.F.; World Stroke Organisation Brain & Heart Task Force. Post-Stroke Cardiovascular Complications and Neurogenic Cardiac Injury: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 2768–2785. [Google Scholar] [CrossRef] [PubMed]
- Longhitano, Y.; Bottinelli, M.; Pappalardo, F.; Maj, G.; Audo, A.; Srejic, U.; Rasulo, F.A.; Zanza, C. Electrocardiogram Alterations in Non-Traumatic Brain Injury: A Systematic Review. J. Clin. Monit. Comput. 2023, 38, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Fujita, T.; Nakaoka, Y.; Hayashi, S.; Imai, R.-I.; Nishida, K.; Seki, S.-I.; Kubo, T.; Yamasaki, N.; Kitaoka, H.; Kubokawa, S.-I.; et al. Incidence and Clinical Characteristics of Takotsubo Syndrome in Patients with Subarachnoid Hemorrhage. Int. Heart J. 2022, 63, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Praveen, R.; Jayant, A.; Mahajan, S.; Jangra, K.; Panda, N.B.; Grover, V.K.; Tewari, M.K.; Bhagat, H. Perioperative Cardiovascular Changes in Patients with Traumatic Brain Injury: A Prospective Observational Study. Surg. Neurol. Int. 2021, 12, 174. [Google Scholar] [CrossRef]
- Lenstra, J.-J.; Kuznecova-Keppel Hesselink, L.; la Bastide-van Gemert, S.; Jacobs, B.; Nijsten, M.W.N.; van der Horst, I.C.C.; van der Naalt, J. The Association of Early Electrocardiographic Abnormalities with Brain Injury Severity and Outcome in Severe Traumatic Brain Injury. Front. Neurol. 2020, 11, 597737. [Google Scholar] [CrossRef] [PubMed]
- Yücetas, S.C.; Kaya, H.; Kafadar, S.; Kafadar, H.; Tibilli, H.; Akcay, A. Evaluation of Index of Cardiac-Electrophysiological Balance in Patients with Subarachnoid Hemorrhage. BMC Cardiovasc. Disord. 2022, 22, 477. [Google Scholar] [CrossRef]
- Sharma, A.K.; Singh, D.; Mahajan, B.; Tandon, M.; Singh, H. Role of High-Sensitivity Troponin-T and N-Terminal pro B-Type Natriuretic Peptide as an Early Predictor of Myocardial Dysfunction in Aneurysmal Subarachnoid Hemorrhage: A Prospective Observational Study. Neurol. India 2022, 70, 1475–1480. [Google Scholar] [CrossRef]
- Qin, G.; Dai, C.; Feng, S.; Wu, G. Changes of Electrocardiogram and Myocardial Enzymes in Patients with Intracerebral Hemorrhage. Dis. Markers 2022, 2022, 9309444. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, V.; Manley, G.T.; Jain, S.; Sun, S.; Foreman, B.; Komisarow, J.; Laskowitz, D.T.; Mathew, J.P.; Hernandez, A.; James, M.L.; et al. Incidence and Clinical Impact of Myocardial Injury Following Traumatic Brain Injury: A Pilot TRACK-TBI Study. J. Neurosurg. Anesthesiol. 2022, 34, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Zahid, T.; Eskander, N.; Emamy, M.; Ryad, R.; Jahan, N. Cardiac Troponin Elevation and Outcome in Subarachnoid Hemorrhage. Cureus 2020, 12, e9792. [Google Scholar] [CrossRef]
- Miketic, J.K.; Hravnak, M.; Sereika, S.M.; Crago, E.A. Elevated Cardiac Troponin I and Functional Recovery and Disability in Patients after Aneurysmal Subarachnoid Hemorrhage. Am. J. Crit. Care 2010, 19, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Naidech, A.M.; Kreiter, K.T.; Janjua, N.; Ostapkovich, N.D.; Parra, A.; Commichau, C.; Fitzsimmons, B.-F.M.; Connolly, E.S.; Mayer, S.A. Cardiac Troponin Elevation, Cardiovascular Morbidity, and Outcome after Subarachnoid Hemorrhage. Circulation 2005, 112, 2851–2856. [Google Scholar] [CrossRef] [PubMed]
- Tung, P.; Kopelnik, A.; Banki, N.; Ong, K.; Ko, N.; Lawton, M.T.; Gress, D.; Drew, B.; Foster, E.; Parmley, W.; et al. Predictors of Neurocardiogenic Injury after Subarachnoid Hemorrhage. Stroke 2004, 35, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Cai, S.S.; Bonds, B.W.; Hu, P.F.; Stein, D.M. The Role of Cardiac Troponin I in Prognostication of Patients with Isolated Severe Traumatic Brain Injury. J. Trauma. Acute Care Surg. 2016, 80, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Lele, A.; Lakireddy, V.; Gorbachov, S.; Chaikittisilpa, N.; Krishnamoorthy, V.; Vavilala, M.S. A Narrative Review of Cardiovascular Abnormalities After Spontaneous Intracerebral Hemorrhage. J. Neurosurg. Anesthesiol. 2018, 31, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Prathep, S.; Sharma, D.; Hallman, M.; Joffe, A.; Krishnamoorthy, V.; Mackensen, G.B.; Vavilala, M.S. Preliminary Report on Cardiac Dysfunction after Isolated Traumatic Brain Injury. Crit. Care Med. 2014, 42, 142–147. [Google Scholar] [CrossRef]
- Rimaz, S.; Ashraf, A.; Marzban, S.; Haghighi, M.; Zia Ziabari, S.M.; Biazar, G.; Rimaz, S.; Omidi, S. Significance of Cardiac Troponin I Elevation in Traumatic Brain Injury Patients. Anesth. Pain. Med. 2019, 9, e90858. [Google Scholar] [CrossRef]
- ICD-ICD-9-CM-International Classification of Diseases, Ninth Revision, Clinical Modification. Available online: https://www.cdc.gov/nchs/icd/icd9cm.htm (accessed on 18 January 2024).
- ICD-ICD-10-International Classification of Diseases, Tenth Revision. Available online: https://www.cdc.gov/nchs/icd/icd10.htm (accessed on 18 January 2024).
- Chaikittisilpa, N.; Kiatchai, T.; Liu, S.Y.; Kelly-Hedrick, M.; Vavilala, M.S.; Lele, A.V.; Komisarow, J.; Ohnuma, T.; Colton, K.; Krishnamoorthy, V. Incidence of Myocardial Injury and Cardiac Dysfunction After Adult Traumatic Brain Injury: A Systematic Review and Meta-Analysis. J. Neurosurg. Anesthesiol. 2023. [Google Scholar] [CrossRef]
- Salem, R.; Vallée, F.; Dépret, F.; Callebert, J.; Maurice, J.P.S.; Marty, P.; Matéo, J.; Madadaki, C.; Houdart, E.; Bresson, D.; et al. Subarachnoid Hemorrhage Induces an Early and Reversible Cardiac Injury Associated with Catecholamine Release: One-Week Follow-up Study. Crit. Care 2014, 18, 558. [Google Scholar] [CrossRef]
- Kumar, P.V.; Vannemreddy, P.; Kumar, D.; Nanda, A.; Reddy, P. Cardiac Troponin I Levels Are a Marker of Myocardial Dysfunction in Subarachnoid Hemorrhage and Predicts Poor Neurologic Outcome. J. La. State Med. Soc. 2011, 163, 257–260. [Google Scholar]
- Parekh, N.; Venkatesh, B.; Cross, D.; Leditschke, A.; Atherton, J.; Miles, W.; Winning, A.; Clague, A.; Rickard, C. Cardiac Troponin I Predicts Myocardial Dysfunction in Aneurysmal Subarachnoid Hemorrhage. J. Am. Coll. Cardiol. 2000, 36, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Deibert, E.; Barzilai, B.; Braverman, A.C.; Edwards, D.F.; Aiyagari, V.; Dacey, R.; Diringer, M. Clinical Significance of Elevated Troponin I Levels in Patients with Nontraumatic Subarachnoid Hemorrhage. J. Neurosurg. 2003, 98, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Bulsara, K.R.; McGirt, M.J.; Liao, L.; Villavicencio, A.T.; Borel, C.; Alexander, M.J.; Friedman, A.H. Use of the Peak Troponin Value to Differentiate Myocardial Infarction from Reversible Neurogenic Left Ventricular Dysfunction Associated with Aneurysmal Subarachnoid Hemorrhage. J. Neurosurg. 2003, 98, 524–528. [Google Scholar] [CrossRef]
- Coppalini, G.; Salvagno, M.; Peluso, L.; Bogossian, E.G.; Quispe Cornejo, A.; Labbé, V.; Annoni, F.; Taccone, F.S. Cardiac Injury after Traumatic Brain Injury: Clinical Consequences and Management. Neurocrit. Care 2023, 40, 477–485. [Google Scholar] [CrossRef]
- Hays, A.; Diringer, M.N. Elevated Troponin Levels Are Associated with Higher Mortality Following Intracerebral Hemorrhage. Neurology 2006, 66, 1330–1334. [Google Scholar] [CrossRef]
- Esteak, T.; Hasan, M.; Atiqur Rahman, M.; Islam, D.M.K.; Ray, S.K.; Hosain, A.; Alam, S.; Zannat, T.; Hasan, A.H.; Khan, S.U. Elevated Troponin I as a Marker for Unfavorable Outcomes in Acute Ischemic Stroke. Cureus 2023, 15, e49568. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Jiang, M.; Gong, D.; Man, C.; Chen, Y. Cardiac Troponin for Predicting All-Cause Mortality in Patients with Acute Ischemic Stroke: A Meta-Analysis. Biosci. Rep. 2018, 38. [Google Scholar] [CrossRef]
- Kishima, H.; Mine, T.; Ando, T.; Yamada, Y.; Tsuji, M.; Ohmura, T.; Miyake, H.; Ishihara, M. Plasma Brain Natriuretic Peptide Level on Admission Predicts Long-Term Outcome in Patients with Non-Traumatic Subarachnoid Hemorrhage. J. Clin. Neurosci. 2020, 79, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, B.; Qi, S. Impact of Echocardiographic Wall Motion Abnormality and Cardiac Biomarker Elevation on Outcome after Subarachnoid Hemorrhage: A Meta-Analysis. Neurosurg. Rev. 2020, 43, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Sviri, G.E.; Soustiel, J.F.; Zaaroor, M. Alteration in Brain Natriuretic Peptide (BNP) Plasma Concentration Following Severe Traumatic Brain Injury. Acta Neurochir. 2006, 148, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, J.; Tang, Z.; Zhang, P. Association of Natriuretic Peptide with Adverse Outcomes and Disease Severity after Intracerebral Hemorrhage: A Systematic Review. Front. Neurol. 2021, 12, 775085. [Google Scholar] [CrossRef] [PubMed]
- Giudicessi, J.R.; Noseworthy, P.A.; Ackerman, M.J. The QT Interval. Circulation 2019, 139, 2711–2713. [Google Scholar] [CrossRef]
- Zeiler, F.A.; Ercole, A.; Beqiri, E.; Cabeleira, M.; Aries, M.; Zoerle, T.; Carbonara, M.; Stocchetti, N.; Smielewski, P.; Czosnyka, M.; et al. Cerebrovascular Reactivity Is Not Associated with Therapeutic Intensity in Adult Traumatic Brain Injury: A CENTER-TBI Analysis. Acta Neurochir. 2019, 161, 1955–1964. [Google Scholar] [CrossRef] [PubMed]
- RStudio. Available online: https://www.rstudio.com/ (accessed on 7 January 2022).
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, L.B.; Hemphill, J.C., 3rd; Anderson, C.; Becker, K.; Broderick, J.P.; Connolly, E.S., Jr.; Greenberg, S.M.; Huang, J.N.; MacDonald, R.L.; Messé, S.R.; et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2010, 41, 2108–2129. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.G.; Duffis, E.J.; Fisher, M. Cardiac Workup of Ischemic Stroke. Stroke 2009, 40, 2893–2898. [Google Scholar] [CrossRef]
- Monbailliu, T.; Goossens, J.; Hachimi-Idrissi, S. Blood Protein Biomarkers as Diagnostic Tool for Ischemic Stroke: A Systematic Review. Biomark. Med. 2017, 11, 503–512. [Google Scholar] [CrossRef]
- Patil, S.; Rossi, R.; Jabrah, D.; Doyle, K. Detection, Diagnosis and Treatment of Acute Ischemic Stroke: Current and Future Perspectives. Front. Med. Technol. 2022, 4, 748949. [Google Scholar] [CrossRef] [PubMed]
- Olma, M.C.; Tütüncü, S.; Fiessler, C.; Kunze, C.; Krämer, M.; Steindorf-Sabath, L.; Jawad-Ul-Qamar, M.; Kirchhof, P.; Laufs, U.; Schurig, J.; et al. In-Hospital ECG Findings, Changes in Medical Management, and Cardiovascular Outcomes in Patients with Acute Stroke or Transient Ischemic Attack. J. Am. Heart Assoc. 2023, 12, e027149. [Google Scholar] [CrossRef] [PubMed]
- ECG Monitoring after Acute Ischemic Stroke: Does Patient Selection Matter? Neurology 2019, 92, 65–66. Available online: https://www.neurology.org/doi/10.1212/wnl.0000000000006719 (accessed on 19 February 2024). [CrossRef] [PubMed]
- Yaghmoor, B.E.; Alotaibi, S.M.; Enani, M.Z.; AlQudsi, H.S.; Aljehani, M.A.; Althomali, M.H.; Hisan, F.M.; Sindi, G.J.; Alshoaibi, N.A.; Sabbagh, A.J. Electrocardiographic Changes Following Intracranial Haemorrhage: A Retrospective Cohort Study. Neurosci. J. 2020, 25, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, S.; Nagatani, K.; Otani, N.; Wada, K.; Mori, K. Electrocardiograph Abnormalities in Intracerebral Hemorrhage. J. Clin. Neurosci. 2015, 22, 1959–1962. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.-Q.; Zheng, L.-R. Myocardial Ischemic Changes of Electrocardiogram in Intracerebral Hemorrhage: A Case Report and Review of Literature. World J. Clin. Cases 2019, 7, 3603–3614. [Google Scholar] [CrossRef] [PubMed]
- Rosso, M.; Ramaswamy, S.; Mulatu, Y.; Little, J.N.; Kvantaliani, N.; Brahmaroutu, A.; Marczak, I.; Lewey, J.; Deo, R.; Messé, S.R.; et al. Rising Cardiac Troponin: A Prognostic Biomarker for Mortality After Acute Ischemic Stroke. J. Am. Heart Assoc. 2024, 13, e032922. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ouyang, M.; Qiu, J.; Cao, X.; Xu, B.; Sui, Y. Prognostic Value of Serum Cardiac Troponin in Acute Ischemic Stroke: An Updated Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2022, 31, 106444. [Google Scholar] [CrossRef]
- Kim, B.S.; Park, J.-J.; Chang, H.; Kim, S.H.; Kwon, C.H.; Chung, S.-M.; Kim, H.Y.; Kim, H.-J. Association of High-Sensitivity Troponin I with Cardiac and Cerebrovascular Events in Patient after Ischemic Stroke. Cerebrovasc. Dis. 2023, 52, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, Y.I.; Ahn, J.; Ryu, J.-A. Association between High-Sensitivity Cardiac Troponin I and Clinical Prognosis of Neurosurgical and Neurocritically Ill Patients. Diagnostics 2022, 12, 2259. [Google Scholar] [CrossRef]
- Vrtovec, B.; Knezevic, I.; Poglajen, G.; Sebestjen, M.; Okrajsek, R.; Haddad, F. Relation of B-Type Natriuretic Peptide Level in Heart Failure to Sudden Cardiac Death in Patients with and without QT Interval Prolongation. Am. J. Cardiol. 2013, 111, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Chihi, M.; Darkwah Oppong, M.; Pierscianek, D.; Dinger, T.F.; Ahmadipour, Y.; Gembruch, O.; Deuschl, C.; Li, Y.; Schmidt, B.; Wrede, K.H.; et al. Analysis of Brain Natriuretic Peptide Levels after Traumatic Acute Subdural Hematoma and the Risk of Post-Operative Cerebral Infarction. J. Neurotrauma 2021, 38, 3068–3076. [Google Scholar] [CrossRef] [PubMed]
- Chihi, M.; Jabbarli, R.; Parlak, A.; Darkwah-Oppong, M.; Gembruch, O.; Wrede, K.H.; Sure, U.; Maslehaty, H. Predictors of Brain Natriuretic Peptide Serum Level Elevation in Patients with Symptomatic Chronic Subdural Hematoma: A Prospective Study. J. Clin. Med. 2021, 10, 1791. [Google Scholar] [CrossRef] [PubMed]
- Chihi, M.; Darkwah Oppong, M.; Quesada, C.M.; Dinger, T.F.; Gembruch, O.; Pierscianek, D.; Ahmadipour, Y.; Uerschels, A.-K.; Wrede, K.H.; Sure, U.; et al. Role of Brain Natriuretic Peptide in the Prediction of Early Postoperative Seizures following Surgery for Traumatic Acute Subdural Hematoma: A Prospective Study. Neurol. Ther. 2021, 10, 847–863. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, D.H.; Lee, B.K.; Cho, Y.S.; Kim, D.K.; Jung, Y.H. Role of Electrocardiogram Findings in Predicting 48-h Mortality in Patients with Traumatic Brain Injury. BMC Neurol. 2022, 22, 190. [Google Scholar] [CrossRef]
- Venkata, C.; Kasal, J. Cardiac Dysfunction in Adult Patients with Traumatic Brain Injury: A Prospective Cohort Study. Clin. Med. Res. 2018, 16, 57–65. [Google Scholar] [CrossRef]
| Cardiac Troponin (ng/mL) | Median | <25th Quartile | 26–50th Quartile | >50–75th Quartile | >75th Quartile |
| AIS | 0.12 | 0–0.05 | 0.06–0.12 | 0.13–0.60 | 0.61–69 |
| sICH | 0.08 | 0.03–0.04 | 0.05–0.08 | 0.09–0.38 | 0.39–68 |
| SAH | 0.24 | 0.03–0.06 | 0.07–0.24 | 0.25–1.21 | 1.22–58 |
| TBI | 0.07 | 0.03–0.04 | 0.05–0.07 | 0.08–0.28 | 0.29–20.6 |
| Beta-Natriuretic Peptide (pg/mL) | Median | <25th Quartile | 26–50th Quartile | >50–75th Quartile | >75th Quartile |
| AIS | 144.5 | 3–58.75 | 58.76–144.5 | 145–347 | 348–22460 |
| sICH | 152 | 7–68 | 69–152 | 153–356 | 357–2982 |
| SAH | 133 | 11–58 | 59–133 | 134–253 | 254–5679 |
| TBI | 168 | 12–69 | 69–168 | 169–427 | 428–9480 |
| Overall | No Cardiac Evaluation | Cardiac Evaluation | aOR | |
|---|---|---|---|---|
| (n = 11,822) | (n = 4350) | (n = 7472) | [95% CI] | |
| Age in years | ||||
| 18–44 | 2406 (20.4%) | 1268 (29.1%) | 1138 (15.2%) | Reference |
| 45–64 | 4093 (34.6%) | 1432 (32.9%) | 2661 (35.6%) | 1.74 [1.55, 1.95] |
| 65–79 | 3520 (29.8%) | 1093 (25.1%) | 2427 (32.5%) | 2.11 [1.88, 2.40] |
| ≥80 | 1803 (15.3%) | 557 (12.8%) | 1246 (16.7%) | 2.48 [2.14, 2.88] |
| Sex | ||||
| Female | 4795 (40.6%) | 1716 (39.4%) | 3079 (41.2%) | Reference |
| Male | 7027 (59.4%) | 2634 (60.6%) | 4393 (58.8%) | 1.16 [1.07, 1.27] |
| Race category | ||||
| White | 9007 (76.2%) | 3375 (77.6%) | 5632 (75.4%) | Reference |
| Non-white | 2815 (23.8%) | 975 (22.4%) | 1840 (24.6%) | 1.11 [1.01, 1.22] |
| Insurance | ||||
| Commercial | 2955 (25.0%) | 1244 (28.6%) | 1711 (22.9%) | Reference |
| Non-commercial | 8867 (75.0%) | 3106 (71.4%) | 5761 (77.1%) | 1.21 [1.09, 1.33] |
| Pre-admission cardiac disorder | ||||
| No | 5562 (47.0%) | 2460 (56.6%) | 3102 (41.5%) | Reference |
| Yes | 6260 (53.0%) | 1890 (43.4%) | 4370 (58.5%) | 1.21 [1.09, 1.34] |
| Admitting diagnosis | ||||
| Acute ischemic stroke | 4272 (36.1%) | 784 (18.0%) | 3488 (46.7%) | Reference |
| Spontaneous intracerebral hemorrhage | 2569 (21.7%) | 1186 (27.3%) | 1383 (18.5%) | 0.25 [0.22, 0.29] |
| Subarachnoid hemorrhage | 1708 (14.4%) | 605 (13.9%) | 1103 (14.8%) | 0.36 [0.30, 0.43] |
| Traumatic brain injury | 3273 (27.7%) | 1775 (40.8%) | 1498 (20.0%) | 0.19 [0.17, 0.24] |
| Admission GCS | ||||
| 13–15 | 6870 (58.1%) | 2710 (62.3%) | 4160 (55.7%) | Reference |
| 9–12 | 1455 (12.3%) | 396 (9.1%) | 1059 (14.2%) | 1.21 [1.05, 1.39] |
| 3–8 | 3497 (29.6%) | 1244 (28.6%) | 2253 (30.2%) | 0.75 [0.66, 0.80] |
| Mechanical ventilation | ||||
| No | 6641 (56.2%) | 2728 (62.7%) | 3913 (52.4%) | Reference |
| Yes | 5181 (43.8%) | 1622 (37.3%) | 3559 (47.6%) | 1.78 [1.57, 2.02] |
| Intracranial pressure monitoring | ||||
| No | 9595 (81.2%) | 3742 (86.0%) | 5853 (78.3%) | Reference |
| Yes | 2227 (18.8%) | 608 (14.0%) | 1619 (21.7%) | 1.68 [1.49, 1.89] |
| ECG n = 7263 | cTnI n = 4121 | BNP n = 2653 | TTE n = 3980 | All Four Tests | |
|---|---|---|---|---|---|
| aOR [95% CI] | aOR [95% CI] | aOR [95% CI] | aOR [95% CI] | aOR [95% CI] | |
| Age in years | |||||
| 18–44 | Reference | Reference | Reference | Reference | Reference |
| 45–64 | 1.32 [1.16; 1.49] | 2.17 [1.89; 2.50] | 1.81 [1.53; 2.15] | 1.74 [1.50; 2.02] | 1.76 [1.33, 2.36] |
| 65–79 | 1.59 [1.39; 1.82] | 2.79 [2.40; 3.24] | 2.46 [2.06; 2.96] | 2.67 [2.28; 3.13] | 2.33 [1.74, 3.15] |
| >80 | 1.82 [1.55; 2.14] | 3.28 [2.77; 3.90] | 2.47 [2.00; 3.05] | 2.74 [2.28; 3.30] | 2.30 [1.64, 3.25] |
| Male sex | 1.17 [1.07; 1.27] | 1.13 [1.04; 1.24] | 1.06 [0.95; 1.17] | 1.11 [1.01; 1.22] | 1.14 [0.97, 1.34] |
| Non-white race | 1.01 [0.91; 1.12] | 1.12 [1.01; 1.24] | 1.10 [0.97; 1.24] | 0.94 [0.84; 1.05] | 1.02 [0.84, 1.23] |
| Cardiac comorbidity | 1.02 [0.93; 1.11] | 1.35 [1.23; 1.48] | 0.88 [0.79; 0.98] | 1.18 [1.07; 1.30] | 0.93 [0.79, 1.10] |
| Non-commercial insurance | 1.14 [1.02; 1.27] | 1.12 [1.00; 1.25] | 0.92 [0.80; 1.05] | 1.09 [0.97; 1.24] | 1.07 [0.87, 1.33] |
| Admitting diagnosis | |||||
| Acute ischemic stroke | Reference | Reference | Reference | Reference | Reference |
| Spontaneous intracerebral hemorrhage | 0.73 [0.65; 0.81] | 0.59 [0.52; 0.66] | 0.13 [0.11; 0.16] | 0.16 [0.14; 0.18] | 0.2 [0.15, 0.26] |
| Subarachnoid hemorrhage | 0.86 [0.75; 0.98] | 1.02 [0.90; 1.17] | 0.40 [0.34; 0.46] | 0.21 [0.18; 0.25] | 0.43 [0.33, 0.55] |
| Traumatic brain injury | 0.57 [0.51; 0.64] | 0.52 [0.46; 0.58] | 0.06 [0.05; 0.08] | 0.13 [0.11; 0.14] | 0.16 [0.12, 0.21] |
| Admission GCS | |||||
| GCS 13–15 | Reference | Reference | Reference | Reference | Reference |
| GCS 9–12 | 1.07 [0.94; 1.21] | 1.43 [1.26; 1.62] | 1.19 [1.03; 1.37] | 1.06 [0.92; 1.21] | 1.36 [1.10, 1.68] |
| GCS 3–8 | 0.70 [0.61; 0.80] | 0.97 [0.84; 1.12] | 0.82 [0.69; 0.97] | 0.76 [0.66; 0.89] | 0.97 [0.76, 1.22] |
| Mechanical ventilation | 2.12 [1.90; 2.37] | 1.23 [1.09; 1.37] | 0.96 [0.84; 1.10] | 1.72 [1.52; 1.95] | 1.78 [1.47, 2.16] |
| Intracranial pressure monitoring | 1.52 [1.35; 1.72] | 1.55 [1.37; 1.76] | 1.04 [0.90; 1.21] | 1.01 [0.88; 1.17] | 1.24 [0.99, 1.54] |
| All-Cause in-Hospital Mortality | Death by Neurologic Criteria | Transition to Comfort Measures Only | Discharged to Home from the Hospital | |
|---|---|---|---|---|
| n = 1961 | n = 329 | n = 1426 | n = 4315 | |
| aOR [95% CI] | aOR [95% CI] | aOR [95% CI] | aOR [95% CI] | |
| Cardiac troponin | ||||
| <25th quartile | Reference | Reference | Reference | Reference |
| 25–50th quartile | 2.04 [0.62–6.71] | 1.65 [1.10–2.47] | 1.33 [0.83–2.14] | 1.13 [0.82–1.56] |
| >50th–75th quartile | 2.50 [0.83–7.50] | 1.79 [1.22–2.63] | 1.77 [1.14–2.73] | 1.26 [0.93–1.72] |
| >75th quartile | 4.38 [1.60–11.9] | 2.18 [1.49–3.17] | 1.81 [1.18–2.78] | 1.08 [0.79–1.49] |
| Beta-natriuretic peptide | ||||
| <25th quartile | Reference | Reference | Reference | Reference |
| 25–50th quartile | 0.52 [0.08–3.36] | 1.97 [0.85–4.54] | 2.18 [0.99–4.77] | 1.21 [0.76–1.92] |
| >50th–75th quartile | 2.98 [0.64–13.74] | 2.86 [1.28–6.40] | 1.75 [0.79–3.86] | 1.35 [0.83–2.21] |
| >75th quartile | 1.73 [0.39–7.66] | 4.54 [2.09–9.85] | 2.44 [1.13–5.22] | 0.91 [0.55–1.51] |
| Prolonged QTc | 2.09 [1.75; 2.50] | 3.41 [2.28; 5.30] | 1.71 [1.39; 2.12] | 0.66 [0.58; 0.76] |
| Ejection fraction < 40% | 1.70 [1.29; 2.23] | 2.47 [1.07; 5.14] | 1.39 [1.00; 1.91] | 0.93 [0.70; 1.23] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lele, A.V.; Liu, J.; Kunapaisal, T.; Chaikittisilpa, N.; Kiatchai, T.; Meno, M.K.; Assad, O.R.; Pham, J.; Fong, C.T.; Walters, A.M.; et al. Early Cardiac Evaluation, Abnormal Test Results, and Associations with Outcomes in Patients with Acute Brain Injury Admitted to a Neurocritical Care Unit. J. Clin. Med. 2024, 13, 2526. https://doi.org/10.3390/jcm13092526
Lele AV, Liu J, Kunapaisal T, Chaikittisilpa N, Kiatchai T, Meno MK, Assad OR, Pham J, Fong CT, Walters AM, et al. Early Cardiac Evaluation, Abnormal Test Results, and Associations with Outcomes in Patients with Acute Brain Injury Admitted to a Neurocritical Care Unit. Journal of Clinical Medicine. 2024; 13(9):2526. https://doi.org/10.3390/jcm13092526
Chicago/Turabian StyleLele, Abhijit V., Jeffery Liu, Thitikan Kunapaisal, Nophanan Chaikittisilpa, Taniga Kiatchai, Michael K. Meno, Osayd R. Assad, Julie Pham, Christine T. Fong, Andrew M. Walters, and et al. 2024. "Early Cardiac Evaluation, Abnormal Test Results, and Associations with Outcomes in Patients with Acute Brain Injury Admitted to a Neurocritical Care Unit" Journal of Clinical Medicine 13, no. 9: 2526. https://doi.org/10.3390/jcm13092526
APA StyleLele, A. V., Liu, J., Kunapaisal, T., Chaikittisilpa, N., Kiatchai, T., Meno, M. K., Assad, O. R., Pham, J., Fong, C. T., Walters, A. M., Nandate, K., Chowdhury, T., Krishnamoorthy, V., Vavilala, M. S., & Kwon, Y. (2024). Early Cardiac Evaluation, Abnormal Test Results, and Associations with Outcomes in Patients with Acute Brain Injury Admitted to a Neurocritical Care Unit. Journal of Clinical Medicine, 13(9), 2526. https://doi.org/10.3390/jcm13092526





