Frequency, Prognosis, and Clinical Features of Unexpected versus Expected Cardiac Arrest in the Emergency Department: A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
- A waiting area dedicated for patients classified as stable, who do not require any monitoring or acute therapy or who are waiting for their visit, results, or discharge;
- An observation area dedicated to patients classified as stable, requiring acute therapy or a low to moderate level of monitoring. This is also an area for patients waiting for boarding to other units (20 beds);
- A shock room dedicated to patients requiring immediate intensive therapy/resuscitation (e.g., victims of polytrauma or CA) (2 beds);
- An intensive-therapy room dedicated to patients requiring intensive monitoring and therapy because of their general instability (4 beds).
- Red (1) for patients requiring immediate resuscitation;
- Orange (2) for patients in the ED;
- Yellow (3) for patients in need of urgent visits;
- Green (4) for patients in need of a visit of low urgency;
- Blue (5) for patients without urgent conditions.
2.2. Definition of Unexpected Cardiac Arrest in the Emergency Department
2.3. Selection of Participants
2.4. Outcome Measures
2.5. Analysis
2.6. Ethics Approval and Consent to Participate
3. Results
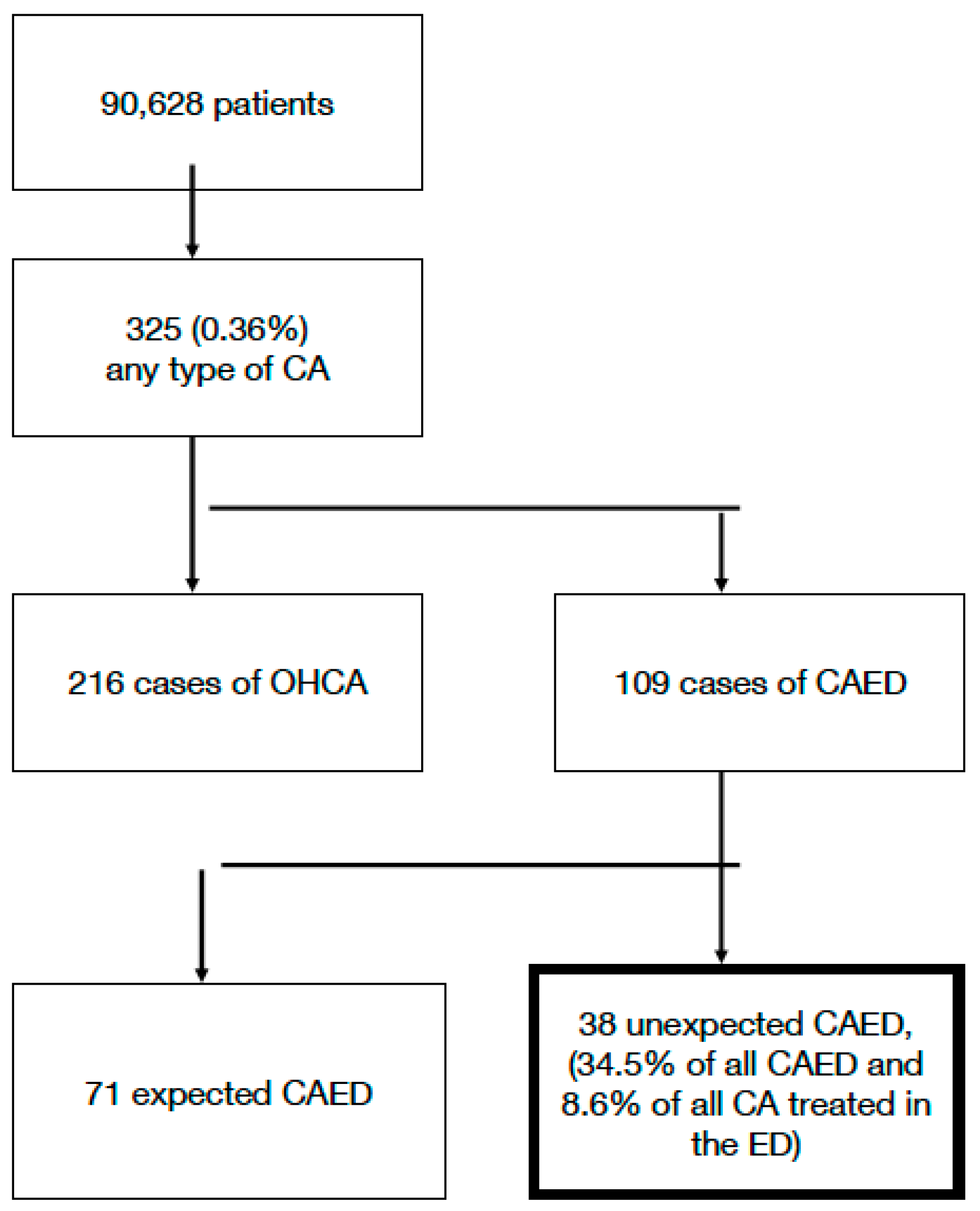
3.1. Characteristics of the Study Participants
3.2. Main Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adamski, J.; Nowakowski, P.; Gorynski, P.; Onichimowski, D.; Weigl, W. Incidence of in-hospital cardiac arrest in Poland. Anaesthesiol. Intensive Ther. 2016, 48, 288–293. [Google Scholar] [CrossRef]
- Mitchell, O.J.L.; Edelson, D.P.; Abella, B.S. Predicting cardiac arrest in the emergency department. J. Am. Coll. Emerg. Physicians Open 2020, 1, 321–326. [Google Scholar] [CrossRef]
- Kayser, R.G.; Ornato, J.P.; Peberdy, M.A. American Heart Association National Registry of Cardiopulmonary Resuscitation. Cardiac arrest in the emergency department: A report from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2008, 78, 151–160. [Google Scholar] [CrossRef]
- Sittichanbuncha, Y.; Prachanukool, T.; Sawanyawisuth, K. A 6-year experience of CPR outcomes in an emergency department in Thailand. Ther. Clin. Risk Manag. 2013, 9, 377–381. [Google Scholar]
- Mir, T.; Qureshi, W.T.; Uddin, M.; Soubani, A.; Saydain, G.; Rab, T.; Kakouros, N. Predictors and outcomes of cardiac arrest in the emergency department and in-patient settings in the United States (2016–2018). Resuscitation 2022, 170, 100–106. [Google Scholar] [CrossRef]
- Miranzadeh, S.; Adib-Hajbaghery, M.; Hosseinpour, N. A prospective study of survival after in-hospital cardiopulmonary resuscitation and its related factors. Trauma Mon. 2016, 21, e31796. [Google Scholar] [CrossRef] [PubMed]
- Kornegay, J.G.; Daya, M.R. Emergency department cardiac arrests: Who, when, and why? Insights from Sweden. Resuscitation 2022, 175, 44–45. [Google Scholar] [CrossRef] [PubMed]
- Kimblad, H.; Marklund, J.; Riva, G.; Rawshani, A.; Lauridsen, K.G.; Djärv, T. Adult cardiac arrest in the emergency department—A Swedish cohort study. Resuscitation 2022, 175, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Funakoshi, H.; Shiga, T.; Homma, Y.; Nakashima, Y.; Takahashi, J.; Kamura, H.; Ikusaka, M. Validation of the modified Japanese Triage and Acuity Scale-based triage system emphasizing the physiologic variables or mechanism of injuries. Int. J. Emerg. Med. 2016, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Hodgetts, T.J.; Kenward, G.; Vlackonikolis, I.; Payne, S.; Castle, N.; Crouch, R.; Ineson, N.; Shaikh, L. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation 2002, 54, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Rogne, T.; Nordseth, T.; Marhaug, G.; Berg, E.M.; Tromsdal, A.; Sæther, O.; Gisvold, S.; Hatlen, P.; Hogan, H.; Solligård, E. Rate of avoidable deaths in a Norwegian hospital trust as judged by retrospective chart review. BMJ Qual. Saf. 2019, 28, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Mankidy, B.; Howard, C.; Morgan, C.K.; Valluri, K.A.; Giacomino, B.; Marfil, E.; Voore, P.; Ababio, Y.; Razjouyan, J.; Naik, A.D.; et al. Reduction of in-hospital cardiac arrest with sequential deployment of rapid response team and medical emergency team to the emergency department and acute care wards. PLoS ONE 2020, 15, e0241816. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-S.; Bae, H.-J.; Sohn, C.H.; Cho, S.E.; Hwang, J.; Kim, W.Y.; Kim, N.; Seo, D.W. Maximum emergency department overcrowding is correlated with occurrence of unexpected cardiac arrest. Crit. Care 2020, 24, 305. [Google Scholar] [CrossRef] [PubMed]
- Bircher, N.G.; Chan, P.S.; Xu, Y.; American Heart Association’s Get with the Guidelines–Resuscitation Investigators. Delays in cardiopulmonary resuscitation, defibrillation, and epinephrine administration all decrease survival in in-hospital cardiac arrest. Anesthesiology 2019, 130, 414–422. [Google Scholar] [CrossRef]
- Handolin, L.E.; Jääskeläinen, J. Pre-notification of arriving trauma patient at trauma centre: A retrospective analysis of the information in 700 consecutive cases. Scand. J. Trauma. Resusc. Emerg. Med. 2008, 16, 15. [Google Scholar] [CrossRef]
- Savage, M.L.; Poon, K.K.C.; Johnston, E.M.; Raffel, O.C.; Incani, A.; Bryant, J.; Rashford, S.; Pincus, M.; Walters, D.L. Pre-hospital ambulance notification and initiation of treatment of ST elevation myocardial infarction is associated with significant reduction in door-to-balloon time for primary PCI. Heart Lung Circ. 2014, 23, 435–443. [Google Scholar] [CrossRef]
- Chang, Y.-H.; Shih, H.-M.; Chen, C.-Y.; Chen, W.-K.; Huang, F.-W.; Muo, C.-H. Association of sudden in-hospital cardiac arrest with emergency department crowding. Resuscitation 2019, 138, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.; Boyle, A.; Holroyd, B.; Phillips, G.; Benger, J.; Chartier, L.B.; Lecky, F.; Vaillancourt, S.; Cameron, P.; Waligora, G.; et al. Updated framework on quality and safety in emergency medicine. Emerg. Med. J. 2020, 37, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Alishahi Tabriz, A.; Trogdon, J.G.; Fried, B.J. Association between adopting emergency department crowding interventions and emergency departments’ core performance measures. Am. J. Emerg. Med. 2020, 38, 258–265. [Google Scholar] [CrossRef] [PubMed]
| Unex-CAED (n = 38) | CAED (n = 71) | p | |
|---|---|---|---|
| Sex (M/F) (n/n; %/%) | 20/18; 52.6%/47.4% | 35/36; 49.3%/50.7% | 0.8413 |
| Age, years, (mean ± SD) | 71.5 ± 15.6 | 72.7 ± 12.4 | 0.7186 |
| Comorbidities, n (%): | |||
| Cardiac insufficiency | 11 (28.9%) | 15 (21.1%) | 0.4797 |
| Chronic kidney disease | 9 (23.7%) | 10 (14.1%) | 0.2890 |
| Neoplastic disease | 10 (26.3%) | 16 (22.5%) | 0.6465 |
| Coronary disease | 6 (15.8%) | 14 (19.7%) | 0.7960 |
| Dementia | 1 (2.6%) | 4 (5.6%) | 0.6561 |
| Alcohol dependency | 1 (2.6%) | 7 (9.9%) | 0.2571 |
| Pathologic obesity | 1 (2.6%) | 4 (5.6%) | 0.6561 |
| Hypertension | 17 (44.7%) | 28 (39.4%) | 0.0001 |
| Atrial fibrillation | 7 (18.4%) | 11 (15.5%) | 0.0537 |
| Cardiomyopathy | 1 (2.63%) | 3 (4.2%) | 1.0000 |
| COPD 1 | 2 (5.3%) | 9 (12.7%) | 0.3229 |
| Chronic anaemia | 0 (0.0%) | 2 (2.8%) | 0.5416 |
| Hepatic cirrhosis | 0 (0.0%) | 5 (7.0%) | 0.1606 |
| Unex-CAED (n = 38) | CAED (n = 71) | p | |
|---|---|---|---|
| Successful ROSC, n (%) | 17 (44.7%) | 24 (33.8%) | 0.3025 |
| Deaths at ED, n (%) | 21 (55.3%) | 47 (66.2%) | 0.3025 |
| Death during hospitalisation, n (%) | 5 (13.2%) | 11 (15.5%) | 1 |
| Dependent at exception, n (%) | 10 (26.3%) | 20 (28.2%) | 1 |
| Time to resuscitation, minutes (mean ± SD) | 12.6 ± 20.2 | 14.6 ± 17.9 | 0.4084 |
| First observed cardiac rhythm | |||
| VF, n (%) | 4 (10.5%) | 3 (4.2%) | 0.2351 |
| VT, n (%) | 1 (2.6%) | 3 (4.2%) | 1 |
| PEA, n (%) | 24 (63.2%) | 28 (39.4%) | 0.0265 |
| Asystole, n (%) | 7(18.4%) | 35 (49.3%) | 0.0019 |
| Unknown, n (%) | 2 (5.3%) | 2 (2.8%) | 0.6096 |
| Defibrillation during CPR, n (%) | 5 (13.1%) | 6 (8.4%) | 0.5103 |
| Total number of deaths, n (%) | 26 (68.4%) | 58 (81.2%) | 0.1519 |
| Unex-CAED (n = 38) | CAED Group (n = 71) | |
|---|---|---|
| Triage results (colour given) | ||
| Red | 0 (0.0%) | 40 (56.3%) |
| Orange | 13 (34.2%) | 29 (40.8%) |
| Yellow | 15 (39.5%) | 2 (2.8%) |
| Green | 7 (18.4%) | 0 (0.0%) |
| Blue | 0 (0.0%) | 0 (0.0%) |
| CA before triage | 3 (7.9%) | 0 (0.0%) |
| Main symptoms | ||
| Dyspnoea | 15 (39.5%) | 34 (47.9%) |
| Disturbances of consciousness | 9 (23.7%) | 32 (45.1%) |
| Weakness | 8 (21.1%) | 22 (31.1%) |
| Chest pain | 7 (18.4%) | 12 (16.9%) |
| Abdominal pain | 6 (15.8%) | 6 (8.5%) |
| Lower limb pain | 4 (10.5%) | 0 (0.0%) |
| Vomiting | 5 (13.2%) | 6 (8.5%) |
| Fever | 4 (10.5%) | 3 (4.2%) |
| Head injury | 3 (7.9%) | 2 (2.8%) |
| Politrauma | 0 (0.0%) | 1 (1.4%) |
| Seizures | 0 (0.0%) | 1 (1.4%) |
| Final diagnoses | (13 cases were verified during autopsy) | (9 cases were verified during autopsy) |
| Acute myocardial infarction | 7 (18.4%) | 9 (12.7%) |
| Malignant neoplasms with metastases | 5 (13.2%) | 19 (26.8%) |
| Septic shock | 7 (18.4%) | 10 (14.1%) |
| Pulmonary embolism | 4 (10.5%) | 5 (7.0%) |
| Heart failure | 4 (10.5%) | 5 (7.0%) |
| Pneumonia | 3 (7.9%) | 0 (0.0%) |
| Ileus | 2 (5.3%) | 0 (0.0%) |
| Rupture of aortic aneurysm | 1 (2.6%) | 5 (7.0%) |
| Oesophageal varices bleeding | 1 (2.6%) | 4 (5.6%) |
| Cardiac tamponade | 1 (2.6%) | 0 (0.0%) |
| Takotsubo cardiomyopathy | 1 (2.6%) | 0 (0.0%) |
| Alcohol intoxication | 1 (2.6%) | 1 (1.4%) |
| Haemopneumothorax | 1 (2.6%) | 0 (0.0%) |
| Intracranial haemmorhage | 0 (0.0%) | 2 (2.8%) |
| Politrauma | 0 (0.0%) | 1 (1.4%) |
| Aspiration | 0 (0.0%) | 2 (2.8%) |
| Chronic renal disease | 0 (0.0%) | 1 (1.4%) |
| Senility | 0 (0.0%) | 7 (9.9%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szaruta-Raflesz, K.; Łopaciński, T.; Siemiński, M. Frequency, Prognosis, and Clinical Features of Unexpected versus Expected Cardiac Arrest in the Emergency Department: A Retrospective Analysis. J. Clin. Med. 2024, 13, 2509. https://doi.org/10.3390/jcm13092509
Szaruta-Raflesz K, Łopaciński T, Siemiński M. Frequency, Prognosis, and Clinical Features of Unexpected versus Expected Cardiac Arrest in the Emergency Department: A Retrospective Analysis. Journal of Clinical Medicine. 2024; 13(9):2509. https://doi.org/10.3390/jcm13092509
Chicago/Turabian StyleSzaruta-Raflesz, Karolina, Tomasz Łopaciński, and Mariusz Siemiński. 2024. "Frequency, Prognosis, and Clinical Features of Unexpected versus Expected Cardiac Arrest in the Emergency Department: A Retrospective Analysis" Journal of Clinical Medicine 13, no. 9: 2509. https://doi.org/10.3390/jcm13092509
APA StyleSzaruta-Raflesz, K., Łopaciński, T., & Siemiński, M. (2024). Frequency, Prognosis, and Clinical Features of Unexpected versus Expected Cardiac Arrest in the Emergency Department: A Retrospective Analysis. Journal of Clinical Medicine, 13(9), 2509. https://doi.org/10.3390/jcm13092509






