Immune-Mediated Inflammatory Diseases Awareness and Management among Physicians Treating Patients with Inflammatory Bowel Disease: An IG-IBD Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Type of Study
2.2. The Survey
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Responding Physicians
3.2. Characteristics of Working Places of the Responding Physicians
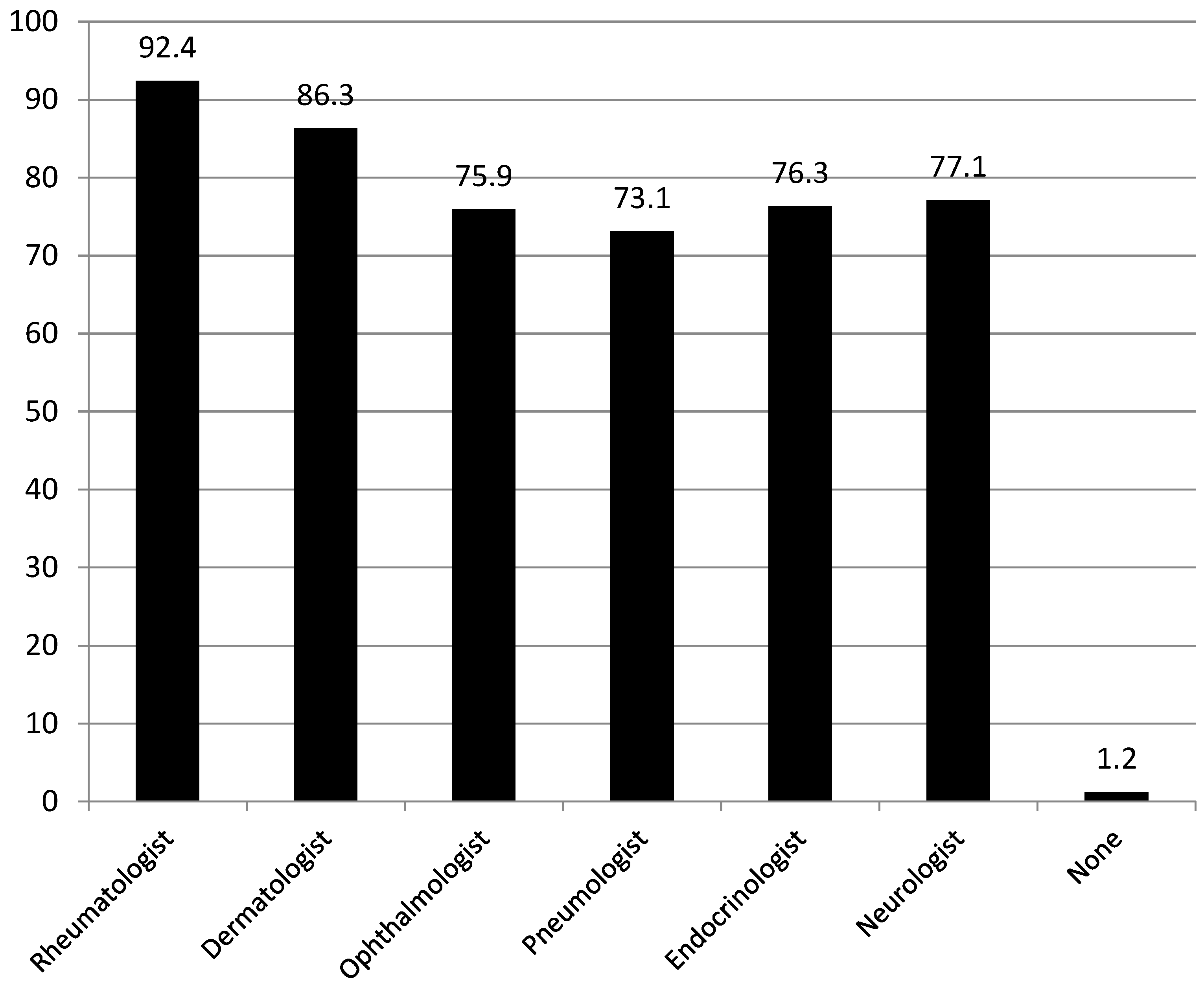
3.3. Presence of Specialists Potentially Involved in Management of IMIDs Associated with IBD and Modalities of Consultation
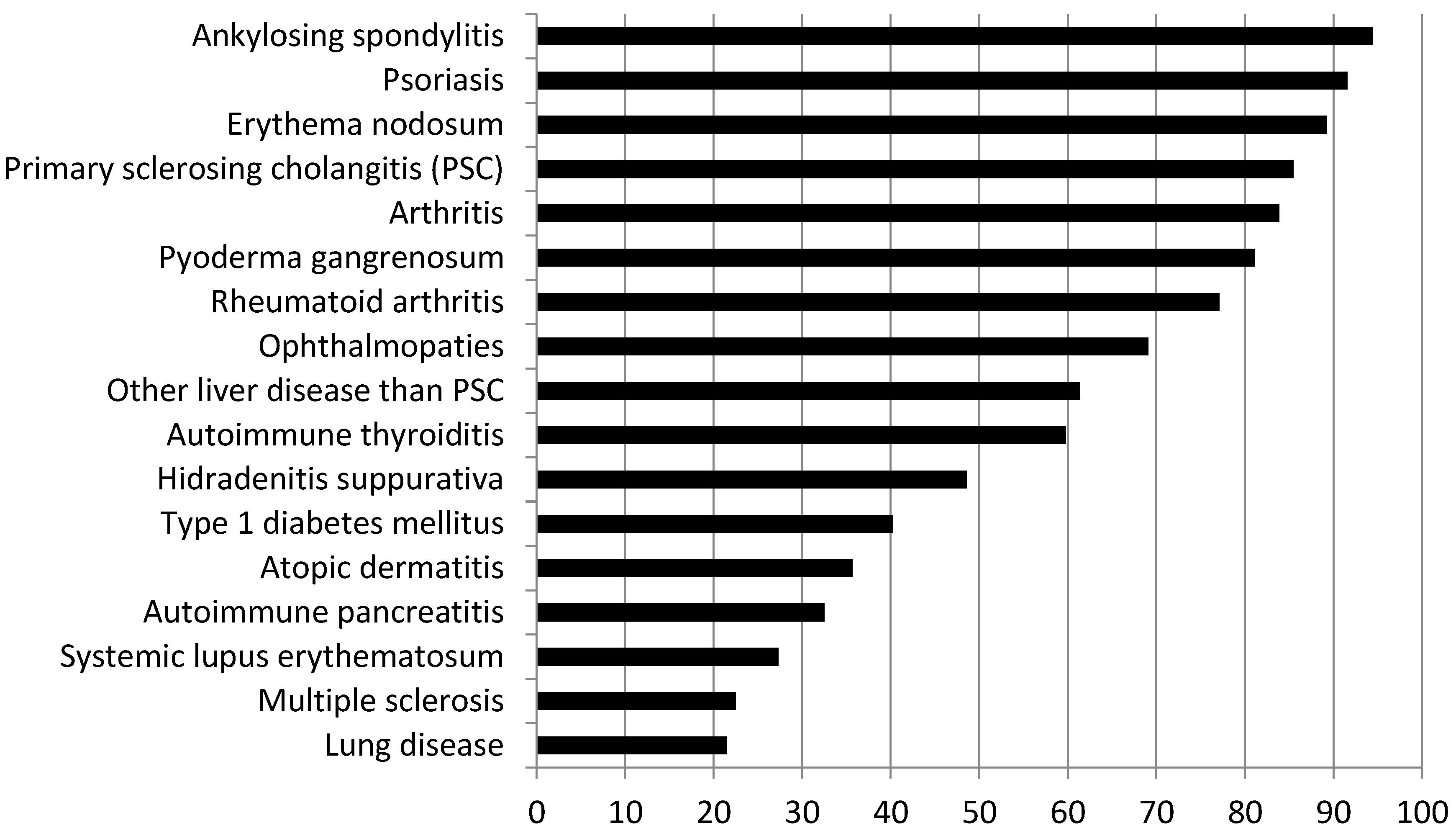
3.4. Attitudes and Feelings of Physicians Managing Patients with IBD toward IMIDs
3.5. Factors Influencing Physicians’ Answers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raine, T.; Bonovas, S.; Burisch, J.; Kucharzik, T.; Adamina, M.; Annese, V.; Bachmann, O.; Bettenworth, D.; Chaparro, M.; Czuber-Dochan, W.; et al. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Medical Treatment. J. Crohns Colitis 2022, 16, 2–17. [Google Scholar] [CrossRef]
- Adamina, M.; Bonovas, S.; Raine, T.; Spinelli, A.; Warusavitarne, J.; Armuzzi, A.; Bachmann, O.; Bager, P.; Biancone, L.; Bokemeyer, B.; et al. ECCO Guidelines on Therapeutics in Crohn’s Disease: Surgical Treatment. J. Crohns Colitis 2020, 14, 155–168. Available online: https://pubmed.ncbi.nlm.nih.gov/31742338/ (accessed on 21 November 2023). [CrossRef]
- Rogler, G.; Singh, A.; Kavanaugh, A.; Rubin, D.T. Extraintestinal Manifestations of Inflammatory Bowel Disease: Current Concepts, Treatment, and Implications for Disease Management. Gastroenterology 2021, 161, 1118–1132. [Google Scholar] [CrossRef]
- Bezzio, C.; Della Corte, C.; Vernero, M.; Di Luna, I.; Manes, G.; Saibeni, S. Inflammatory bowel disease and immune-mediated inflammatory diseases: Looking at the less frequent associations. Ther. Adv. Gastroenterol. 2022, 15, 17562848221115312. [Google Scholar] [CrossRef]
- Antonelli, E.; Bassotti, G.; Tramontana, M.; Hansel, K.; Stingeni, L.; Ardizzone, S.; Genovese, G.; Marzano, A.V.; Maconi, G. Dermatological Manifestations in Inflammatory Bowel Diseases. J. Clin. Med. 2021, 10, 364. [Google Scholar] [CrossRef]
- Fragoulis, G.E.; Liava, C.; Daoussis, D.; Akriviadis, E.; Garyfallos, A.; Dimitroulas, T. Inflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment. World J. Gastroenterol. 2019, 25, 2162–2176. [Google Scholar] [CrossRef] [PubMed]
- Fiorino, G.; Allez, M.; Malesci, A.; Danese, S. Review article: Anti TNF-alpha induced psoriasis in patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2009, 29, 921–927. [Google Scholar] [CrossRef] [PubMed]
- De Bandt, M. Anti-TNF-alpha-induced lupus. Arthritis Res. Ther. 2019, 21, 235. [Google Scholar] [CrossRef] [PubMed]
- Cortese, R.; Prosperini, L.; Stasolla, A.; Haggiag, S.; Villani, V.; Simone, I.L.; Gasperini, C.; Tortorella, C. Clinical course of central nervous system demyelinating neurological adverse events associated with anti-TNF therapy. J. Neurol. 2021, 268, 2895–2899. [Google Scholar] [CrossRef] [PubMed]
- Baena-Díez, J.M.; Garcia-Gil, M.; Comas-Cufí, M.; Ramos, R.; Prieto-Alhambra, D.; Salvador-González, B.; Elosua, R.; Dégano, I.R.; Peñafiel, J.; Grau, M. Association between chronic immune-mediated inflammatory diseases and cardiovascular risk. Heart Br. Card. Soc. 2018, 104, 119–126. [Google Scholar] [CrossRef]
- Marrie, R.A.; Walld, R.; Bolton, J.M.; Sareen, J.; Walker, J.R.; Patten, S.B.; Singer, A.; Lix, L.M.; Hitcho, C.A.; El-Gabalawy, R.; et al. Increased incidence of psychiatric disorders in immune-mediated inflammatory disease. J. Psychosom. Res. 2017, 101, 17–23. [Google Scholar] [CrossRef]
- Beyaert, R.; Beaugerie, L.; Van Assche, G.; Brochez, L.; Renauld, J.C.; Viguier, M.; Cocquyt, V.; Jerusalem, G.; Machiels, J.P.; Prenen, H.; et al. Cancer risk in immune-mediated inflammatory diseases (IMID). Mol. Cancer 2013, 12, 98. [Google Scholar] [CrossRef]
- Attauabi, M.; Zhao, M.; Bendtsen, F.; Burisch, J. Systematic Review with Meta-analysis: The Impact of Co-occurring Immune-mediated Inflammatory Diseases on the Disease Course of Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2021, 27, 927–939. [Google Scholar] [CrossRef]
- Pham, T.; Sokol, H.; Halioua, B.; Pourcel, G.; Brun, M.; Pain, E.; Testa, D. Immune-mediated inflammatory diseases and nutrition: Results from an online survey on patients’ practices and perceptions. BMC Nutr. 2021, 7, 38. [Google Scholar] [CrossRef]
- Bezzio, C.; Alimenti, E.; Saibeni, S. Letter: Immune-mediated inflammatory diseases and inflammatory bowel disease-are we ready for a Copernican revolution? Aliment. Pharmacol. Ther. 2022, 56, 1429–1430. [Google Scholar] [CrossRef]
- Di Carlo, M.; Luchetti, M.M.; Benfaremo, D.; Di Donato, E.; Mosca, P.; Maltoni, S.; Benedetti, A.; Gabrielli, A.; Grassi, W.; Salaffi, F. The DETection of Arthritis in Inflammatory boweL diseases (DETAIL) questionnaire: Development and preliminary testing of a new tool to screen patients with inflammatory bowel disease for the presence of spondyloarthritis. Clin. Rheumatol. 2018, 37, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Ribaldone, D.G.; Vernero, M.; Parisi, S.; Ditto, M.C.; Pellicano, R.; Morino, M.; Saracco, G.M.; Fusaro, E.; Astegiano, M. Risk factors of suspected spondyloarthritis among inflammatory bowel disease patients. Scand. J. Gastroenterol. 2019, 54, 1233–1236. [Google Scholar] [CrossRef] [PubMed]
- Felice, C.; Leccese, P.; Scudeller, L.; Lubrano, E.; Cantini, F.; Castiglione, F.; Gionchetti, P.; Orlando, A.; Salvarani, C.; Scarpa, R.; et al. Red flags for appropriate referral to the gastroenterologist and the rheumatologist of patients with inflammatory bowel disease and spondyloarthritis. Clin. Exp. Immunol. 2019, 196, 123–138. [Google Scholar] [CrossRef] [PubMed]
- Saibeni, S.; Kohn, A.; Meucci, G.; Papi, C. Italian Group for Inflammatory Bowel Disease. How thiopurines are used for the treatment of inflammatory bowel diseases: An Italian survey. Dig. Liver Dis. 2015, 47, 170–173. [Google Scholar] [CrossRef]
- Saibeni, S.; Zanetti, M.; Bezzio, C.; Pironi, L.; Armuzzi, A.; Riso, S.; Caprioli, F.; Lezo, A.; Macaluso, F.S.; Pugliese, D.; et al. Nutritional care at centres managing patients with inflammatory bowel disease: A nationwide survey in Italy. Dig. Liver Dis. 2023, 55, 1028–1033. [Google Scholar] [CrossRef] [PubMed]
- Fascì-Spurio, F.; Meucci, G.; Papi, C.; Saibeni, S.; IG-IBD (Italian Group for Inflammatory Bowel Disease). The use of oral corticosteroids in inflammatory bowel diseases in Italy: An IG-IBD survey. Dig. Liver Dis. 2017, 49, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Robinson, D.; Paramore, C.; Fraeman, K.; Renahan, K.; Bala, M. Autoimmune disease concomitance among inflammatory bowel disease patients in the United States, 2001–2002. Inflamm. Bowel Dis. 2008, 14, 738–743. [Google Scholar] [CrossRef] [PubMed]
- Conway, G.; Velonias, G.; Andrews, E.; Garber, J.J.; Yajnik, V.; Ananthakrishnan, A.N. The impact of co-existing immune-mediated diseases on phenotype and outcomes in inflammatory bowel diseases. Aliment. Pharmacol. Ther. 2017, 45, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Felice, C.; Pugliese, D.; Papparella, L.G.; Pizzolante, F.; Onori, E.; Gasbarrini, A.; Lodovico Rapaccini, G.; Guidi, L.; Armuzzi, A. Clinical management of rheumatologic conditions co-occurring with inflammatory bowel diseases. Expert. Rev. Clin. Immunol. 2018, 14, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Salgado-Boquete, L.; Romaní, J.; Carrión, L.; Marín-Jiménez, I. Epidemiology of hidradenitis suppurativa and inflammatory bowel disease: Are these two disease associated? Actas Dermosifiliogr. 2016, 107 (Suppl. S2), 8–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Lee, J.H.; Koh, S.J.; Park, H. Bidirectional relationship between atopic dermatitis and inflammatory bowel disease: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2020, 83, 1385–1394. [Google Scholar] [CrossRef]
- Blair, H.A. Secukinumab: A Review in Psoriatic Arthritis. Drugs 2021, 81, 483–494. [Google Scholar] [CrossRef]
- Onac, I.A.; Clarke, B.D.; Tacu, C.; Lloyd, M.; Hajela, V.; Batty, T.; Thoroughgood, J.; Smith, S.; Irvine, H.; Hill, D.; et al. Secukinumab as a potential trigger of inflammatory bowel disease in ankylosing spondylitis or psoriatic arthritis patients. Rheumatology 2021, 60, 5233–5238. [Google Scholar] [CrossRef]
- Hu, Q.; Tang, X.Z.; Liu, F.; Liu, D.W.; Cao, B. Vedolizumab subcutaneous formulation maintenance therapy for patients with IBD: A systematic review and meta-analysis. Ther. Adv. Gastroenterol. 2023, 16, 17562848231166227. [Google Scholar] [CrossRef]
- Wetwittayakhlang, P.; Lakatos, P.L. Current Evidence for Combined Targeted Therapy for the Treatment of Inflammatory Bowel Disease. J. Can. Assoc. Gastroenterol. 2024, 7, 22–29. [Google Scholar] [CrossRef]
| n (%) | ||
| SEX | Men | 135 (54.3) |
| Women | 114 (45.7) | |
| AGE | 25–34 years old | 73 (29.3) |
| 35–44 years old | 74 (29.7) | |
| >45 years old | 102 (41.0) | |
| PART OF ITALY | North | 118 (47.4) |
| Center | 79 (31.7) | |
| South | 51 (20.5) | |
| TIME IN IBD FIELD | <5 years | 70 (28.1) |
| 5–15 years | 77 (30.9) | |
| >15 years | 102 (41.0) | |
| SPECIALIZATION | Gastroenterology | 225 (90.4) |
| Internal medicine | 17 (6.8) | |
| Pediatrics | 4 (16) | |
| Surgery | 1 (0.4) | |
| Pathologist | 1 (0.4) |
| n (%) | ||
| Working hospital | Public community | 123 (49.4) |
| Public academic | 64 (25.7) | |
| Private community | 10 (4.0) | |
| Private academic | 22 (8.8) | |
| Private practice | 4 (1.6) | |
| Not reported | 26 (10.5) | |
| Age of patients | >18 years | 179 (71.9) |
| 14–18 years | 64 (25.7) | |
| <14 | 6 (2.4) | |
| Patient load | <500 patients | 62 (24.9) |
| 500–1000 | 87 (34.9%) | |
| 1000–3000 | 64 (25.7%) | |
| >3000 | 36 (14.5%) |
| n (%) | |
| SHARED AMBULATORY | |
| Rheumatologist | 127 (51.0) |
| Dermatologist | 79 (28.5) |
| Ophthalmologist | 17 (6.8) |
| Pneumologist | 9 (3.6) |
| Endocrinologist | 7 (2.8) |
| Neurologist | 5 (2.0) |
| None | 91 (36.5) |
| RESERVED SLOTS | |
| Rheumatologist | 180 (72.3) |
| Dermatologist | 145 (58.2) |
| Ophthalmologist | 56 (22.5) |
| Pneumologist | 32 (12.8) |
| Endocrinologist | 33 (13.2) |
| Neurologist | 26 (10.4) |
| None | 50 (20.1) |
| ON-DEMAND VISIT | |
| Rheumatologist | 209 (83.9) |
| Dermatologist | 188 (75.5) |
| Pneumologist | 112 (44.9) |
| Ophthalmologist | 145 (58.2) |
| Endocrinologist | 111 (44.6) |
| Neurologist | 107 (42.9) |
| None | 6 (2.4) |
| REMOTE CONSULTATION | |
| Rheumatologist | 178 (71.5) |
| Ophthalmologist | 99 (39.7) |
| Pneumologist | 91 (36.5) |
| Endocrinologist | 89 (35.7) |
| Dermatologist | 143 (57.4) |
| Neurologist | 81 (32.5) |
| None | 46 (18.5) |
| Outcome | Variable | OR (95% CI) | p Value |
|---|---|---|---|
| Importance of IMID (>6 on a scale from 0 to 10) | |||
| Male sex | 2.37 (0.12–4.17) | 0.70 | |
| Age > 45 | 0.16 (0.2–1.55) | 0.11 | |
| Location (Northern Italy) | 3.70 (0.34–33.0) | 0.24 | |
| Specialization (Gastroenterology) | Not assessable * | - | |
| Type of hospital (Academic) | 3.36 (0.34–30.5) | 0.28 | |
| Patient load (>1000 patients) | 0.43 (0.71–1.60) | 0.36 | |
| Estimated patients with concomitant IMID > 20% | |||
| Male sex | 0.76 (0.37–1.55) | 0.45 | |
| Age > 45 years | 1.1 (0.52–2.25) | 0.82 | |
| Location (Northern Italy) | 0.87 (0.43–1.77) | 0.70 | |
| Specialization (Gastroenterology) | 1.36 (0.51–3.52) | 0.52 | |
| Type of hospital (Academic) | 1.89 (0.90–3.9) | 0.09 | |
| Patient load (>1000 patients) | 3.40 (1.42–8.12) | 0.005 | |
| Evaluation of other IMID at each visit | |||
| Male sex | 0.80 (0.35–1.66) | 0.51 | |
| Age > 45 years | 1.05 (0.48–2.29) | 0.89 | |
| Location (Northern Italy) | 1.4 (0.65–3.12) | 0.37 | |
| Specialization (Gastroenterology) | 0.72 (0.20–2.55) | 0.60 | |
| Type of hospital (Academic) | 2.48 (1.12–5.81) | 0.03 | |
| Patient load (>1000 patients) | 1.39 (0.62–3.10) | 0.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vernero, M.; Bezzio, C.; Ribaldone, D.G.; Caprioli, F.A.; Fantini, M.C.; Festa, S.; Macaluso, F.S.; Orlando, A.; Pugliese, D.; Renna, S.; et al. Immune-Mediated Inflammatory Diseases Awareness and Management among Physicians Treating Patients with Inflammatory Bowel Disease: An IG-IBD Survey. J. Clin. Med. 2024, 13, 1857. https://doi.org/10.3390/jcm13071857
Vernero M, Bezzio C, Ribaldone DG, Caprioli FA, Fantini MC, Festa S, Macaluso FS, Orlando A, Pugliese D, Renna S, et al. Immune-Mediated Inflammatory Diseases Awareness and Management among Physicians Treating Patients with Inflammatory Bowel Disease: An IG-IBD Survey. Journal of Clinical Medicine. 2024; 13(7):1857. https://doi.org/10.3390/jcm13071857
Chicago/Turabian StyleVernero, Marta, Cristina Bezzio, Davide G. Ribaldone, Flavio A. Caprioli, Massimo C. Fantini, Stefano Festa, Fabio S. Macaluso, Ambrogio Orlando, Daniela Pugliese, Sara Renna, and et al. 2024. "Immune-Mediated Inflammatory Diseases Awareness and Management among Physicians Treating Patients with Inflammatory Bowel Disease: An IG-IBD Survey" Journal of Clinical Medicine 13, no. 7: 1857. https://doi.org/10.3390/jcm13071857
APA StyleVernero, M., Bezzio, C., Ribaldone, D. G., Caprioli, F. A., Fantini, M. C., Festa, S., Macaluso, F. S., Orlando, A., Pugliese, D., Renna, S., Rispo, A., Savarino, E. V., Variola, A., & Saibeni, S., on behalf of the Italian Group for Inflammatory Bowel Disease (IG-IBD). (2024). Immune-Mediated Inflammatory Diseases Awareness and Management among Physicians Treating Patients with Inflammatory Bowel Disease: An IG-IBD Survey. Journal of Clinical Medicine, 13(7), 1857. https://doi.org/10.3390/jcm13071857











