Comparison of Cylindrical and Tapered Stem Designs for Femoral Revision Hip Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Assessment
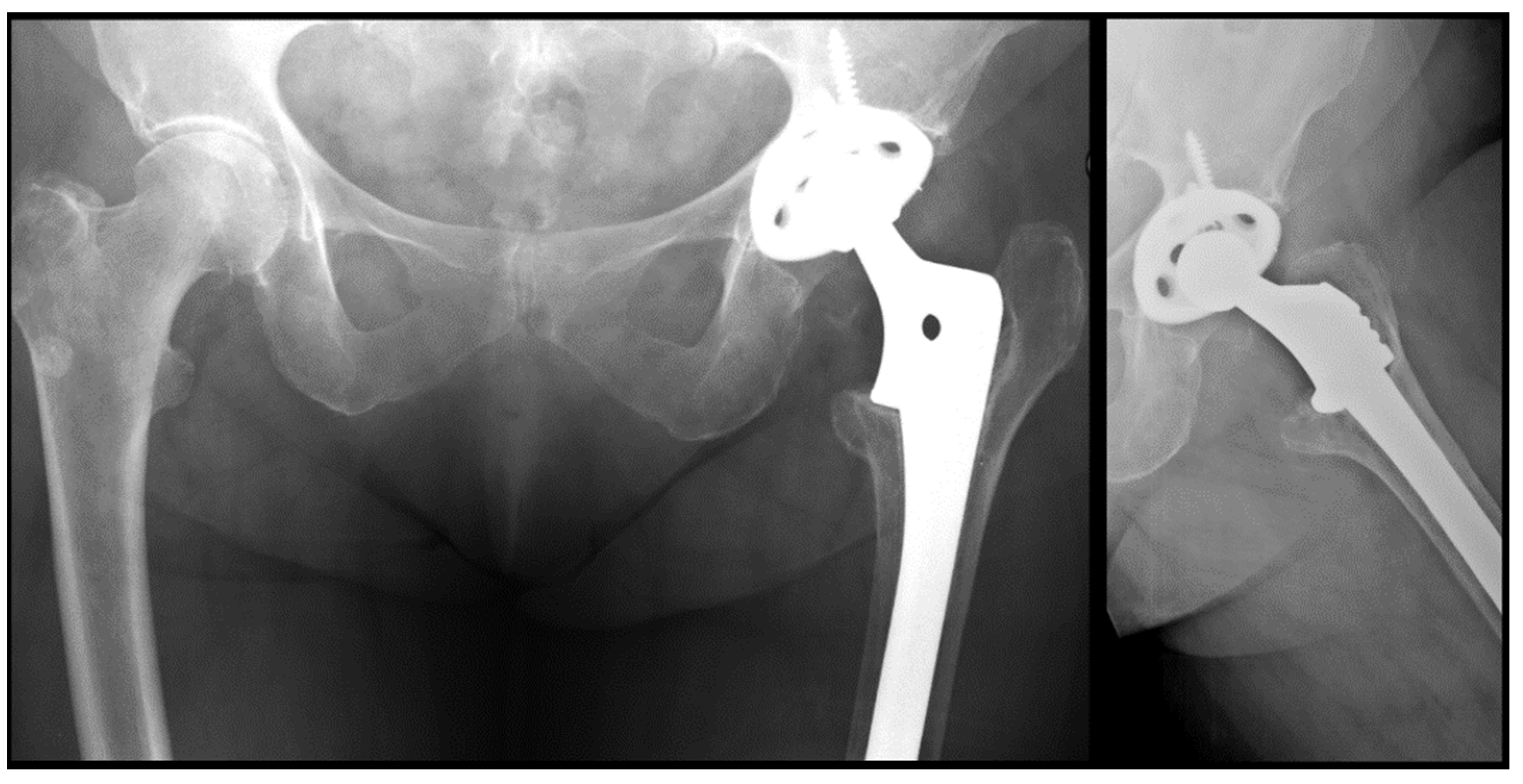
2.2. Radiological Analysis
2.3. Statistical Analysis
3. Results
3.1. Clinical Results
3.2. Radiographic Results
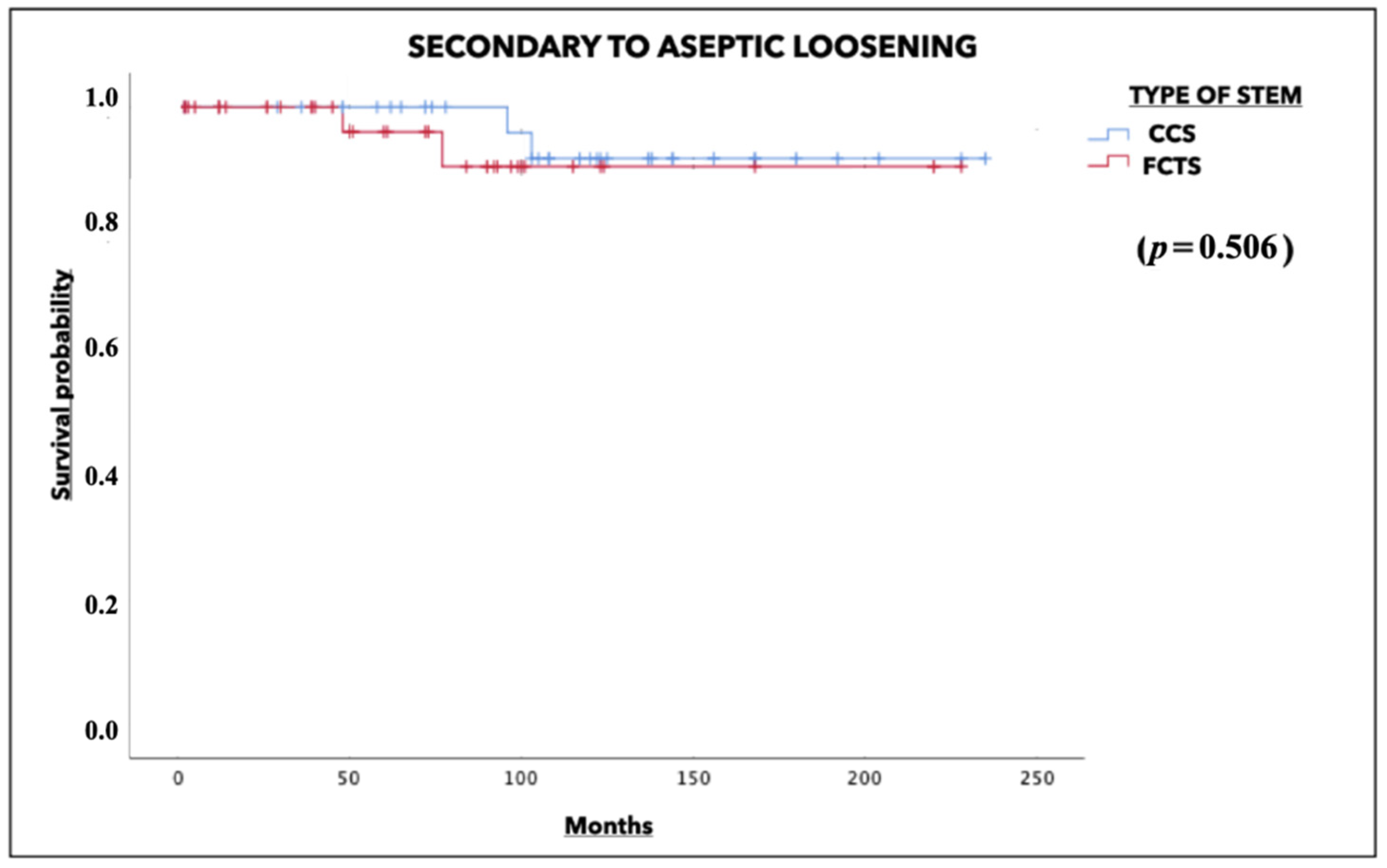
3.3. Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hegde, V.; Stambough, J.B.; Levine, B.R.; Springer, B.D. Highlights of the 2022 American Joint Replacement Registry Annual Report. Arthroplast. Today 2023, 21, 101137. [Google Scholar] [CrossRef] [PubMed]
- Garbuz, D.S.; Toms, A.; Masri, B.A.; Duncan, C.P. Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin. Orthop. Relat. Res. 2006, 453, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Krishnamurthy, A.B.; MacDonald, S.J.; Paprosky, W.G. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J. Arthroplast. 1997, 12, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, Y.; Sun, J.N.; Hua, Z.J.; Chen, X.Y.; Feng, S. Comparison of cylindrical and tapered stem designs for femoral revision hip arthroplasty. BMC Musculoskelet. Disord. 2020, 21, 411. [Google Scholar] [CrossRef] [PubMed]
- Richards, C.J.; Duncan, C.P.; Masri, B.A.; Garbuz, D.S. Femoral revision hip arthroplasty: A comparison of two stem designs. Clin. Orthop. Relat. Res. 2010, 468, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Sheth, N.P.; Nelson, C.L.; Paprosky, W.G. Femoral bone loss in revision total hip arthroplasty: Evaluation and management. J. Am. Acad. Orthop. Surg. 2013, 21, 601–612. [Google Scholar] [CrossRef]
- Park, K.S.; Jin, S.Y.; Lim, J.H.; Yoon, T.R. Long-term outcomes of cementless femoral stem revision with the Wagner cone prosthesis. J. Orthop. Surg. Res. 2021, 16, 375. [Google Scholar] [CrossRef]
- Thomsen, P.B.; Jensen, N.J.; Kampmann, J.; Hansen, T.B. Revision hip arthroplasty with an extensively porous-coated stem—Excellent long-term results also in severe femoral bone stock loss. HIP Int. 2013, 23, 352–358. [Google Scholar] [CrossRef]
- Wilson, M.J.; Hook, S.; Whitehouse, S.L.; Timperley, A.J.; Gie, G.A. Femoral impaction bone grafting in revision hip arthroplasty. Bone Jt. J. 2016, 98 B, 1611–1619. [Google Scholar] [CrossRef]
- McNamara, I.R. Impaction bone grafting in revision hip surgery: Past, present and future. Cell Tissue Bank. 2010, 11, 57–73. [Google Scholar] [CrossRef]
- Sandiford, N.A.; Duncan, C.P.; Garbuz, D.S.; Masri, B.A. Tapered, fluted titanium stems in revision total hip arthroplasty: Role and results in contemporary practice. Instr. Course Lect. 2015, 64, 359–366. [Google Scholar]
- Konan, S.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. Non-modular tapered fluted titanium stems in hip revision surgery. Bone Jt. J. 2014, 96, 56–59. [Google Scholar] [CrossRef]
- Sporer, S.M.; Paprosky, W.G. Revision total hip arthroplasty. Clin. Orthop. Relat. Res. 2003, 417, 203–209. [Google Scholar] [CrossRef]
- Ngu, A.W.T.; Rowan, F.E.; Carli, A.V.; Haddad, F.S. Single 3° tapered fluted femoral stems demonstrate low subsidence at mid-term follow-up in severe bony deficiency. Ann. Transl. Med. 2019, 7, 725. [Google Scholar] [CrossRef]
- Passano, B.; Oakley, C.T.; Lutes, W.B.; Incavo, S.J.; Park, K.J.; Schwarzkopf, R. Clinical and Radiographic Outcomes of a Monoblock Fluted Titanium-Tapered Stem for Paprosky IIIa, IIIb, and IV Femoral Bone Defects. J. Arthroplast. 2023, 38, 1342–1348. [Google Scholar] [CrossRef]
- Valle, C.J.; Paprosky, W.G. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J. Bone Jt. Surg. 2003, 85, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.A.; Deshmukh, A.J.; Klauser, W.U.; Rasquinha, V.J.; Lubinus, P.; Ranawat, C.S. Patterns of osseointegration and remodeling in femoral revision with bone loss using modular, tapered, fluted, titanium stems. J. Arthroplast. 2011, 26, 1409–1417.e1. [Google Scholar] [CrossRef] [PubMed]
- Böhm, P.; Bischel, O. Femoral revision with the Wagner SL revision stem: Evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J. Bone Jt. Surg. 2001, 83, 1023–1031. [Google Scholar] [CrossRef]
- Callaghan, J.J. Results of primary total hip arthroplasty in young patients. J. Bone Jt. Surg. 1993, 75, 1728–1734. [Google Scholar] [CrossRef]
- Sculco, P.K.; Abdel, M.P.; Lewallen, D.G. Management of femoral bone loss in revision total hip arthroplasty. HIP Int. 2015, 25, 380–387. [Google Scholar] [CrossRef]
- Hartwig, C.H.; Böhm, P.; Czech, U.; Reize, P.; Küsswetter, W. The Wagner revision stem in alloarthroplasty of the hip. Arch. Orthop. Trauma Surg. 1996, 115, 5–9. [Google Scholar] [CrossRef]
- Iwana, D.; Nishii, T.; Miki, H.; Sugano, N.; Sakai, T.; Ohzono, K.; Yoshikawa, H. Proximal bone remodelling differed between two types of titanium long femoral components after cementless revision arthroplasty. Int. Orthop. 2008, 32, 431–436. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Friebert, G.; Gombár, C.; Bozó, A.; Polyák, I.; Brzózka, Á.; Sisák, K. Differences between proximal bone remodeling in femoral revisions for aseptic loosening and periprosthetic fractures using the Wagner SL stem. BMC Musculoskelet. Disord. 2021, 22, 201. [Google Scholar] [CrossRef] [PubMed]
- Revision Total Hip Arthroplasty Study Group A comparison of modular tapered versus modular cylindrical stems for complex femoral revisions. J. Arthroplast. 2013, 28 (Suppl. 8), 71–73. [CrossRef]
- Otero, J.E.; Martin, J.R.; Rowe, T.M.; Odum, S.M.; Mason, J.B. Radiographic and Clinical Outcomes of Modular Tapered Fluted Stems for Femoral Revision for Paprosky III and IV Femoral Defects or Vancouver B2 and B3 Femoral Fractures. J. Arthroplast. 2020, 35, 1069–1073. [Google Scholar] [CrossRef]
- Del Alamo, J.G.; Garcia-Cimbrelo, E.; Castellanos, V.; Gil-Garay, E. Radiographic bone regeneration and clinical outcome with the Wagner SL revision stem: A 5-Year to 12-Year Follow-Up Study. J. Arthroplast. 2007, 22, 515–524. [Google Scholar] [CrossRef]
- Böhm, P.; Bischel, O. The use of tapered stems for femoral revision surgery. Clin. Orthop. Relat. Res. 2004, 420, 148–159. [Google Scholar] [CrossRef]
- Engh, C.A., Jr.; Ellis, T.J.; Koralewicz, L.M.; McAuley, J.P.; Engh, C.A., Sr. Extensively porous-coated femoral revision for severe femoral bone loss: Minimum 10-year follow-up. J. Arthroplast. 2002, 17, 955–960. [Google Scholar] [CrossRef]
- Engh, C.A., Jr.; Young, A.M.M.; Hopper, R.H., Jr. Clinical consequences of stress shielding after porous-coated total hip arthroplasty. Clin. Orthop. Relat. Res. 2003, 417, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.D.; Pierce, W.; Huo, M.H. Tapered vs Cylindrical Stem Fixation in a Model of Femoral Bone Deficiency in Revision Total Hip Arthroplasty. J. Arthroplast. 2016, 31, 1352–1355. [Google Scholar] [CrossRef]
- Limmahakhun, S.; Adulkasem, N.; Rungsiyakull, C.; Jingjit, W.; Rojanasthien, S. Micromotion and stress shielding between taper fluted and cylindrical femoral stems for Paprosky bone deficiency type IIIB. Musculoskelet. Surg. 2023, 107, 391–396. [Google Scholar] [CrossRef]
- Grünig, R.; Morscher, E.; Ochsner, P.E. Three- to 7-year results with the uncemented SL femoral revision prosthesis. Arch. Orthop. Trauma Surg. 1997, 116, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Isacson, J.; Stark, A.; Wallensten, R. The Wagner revision prosthesis consistently restores femoral bone structure. Int. Orthop. 2000, 24, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Reitman, R.D.; Emerson, R.; Higgins, L.; Head, W. Thirteen year results of total hip arthroplasty using a tapered titanium femoral component inserted without cement in patients with type C bone. J. Arthroplast. 2003, 18, 116–121. [Google Scholar] [CrossRef] [PubMed]



| Demographic Data | Cylindrical Stems (N = 38) | Tapered Stems (N = 40) |
|---|---|---|
| Age (Years) | 68.55 ± 12.78 | 71.38 ± 12.86 |
| Gender (Male/Female) | 21/17 | 21/19 |
| Side (Right/Left) | 15/23 | 15/25 |
| BMI 1 (kg/m2) | 26.54 ± 5.21 | 26.93 ± 4.97 |
| Stature (cm) | 164.68 ± 6.73 | 167.33 ± 5.22 |
| Smokers (%) | 28.9% | 17.24% |
| Presence of DM (%) | 10.5% | 24.1% |
| Heart failure (%) | 18.42% | 20.7% |
| CKD 2 (%) | 21.1% | 10.3% |
| Immunodeficiency (%) | 2.6% | 5.2% |
| Reasons of revision (n) | ||
| Aseptic loosening | 31 | 20 |
| Infection | 5 | 5 |
| Periprosthetic fracture | 2 | 6 |
| Osteosynthesis failure | 0 | 5 |
| Recurrent dislocation | 0 | 1 |
| Two-stage revision (n) | 2 | 3 |
| Pre-surgical HHS Jr 3 | 47.4 ± 15.3 | 49.3 ± 13.9 |
| Paprosky femoral defect (n) | ||
| Type I | 5 | 0 |
| Type II | 21 | 20 |
| Type IIIA | 11 | 18 |
| Type IIIB | 1 | 2 |
| Acetabular revision (%) | 42.1% | 62.1% |
| Bone graft use (%) | 42.1% | 48.3% |
| Femoral osteotomy (n) | ||
| Not needed | 19 | 27 |
| Trochanteric | 8 | 2 |
| ETO 4 | 11 | 11 |
| Lengths of the Stem Used (n) | |
|---|---|
| FCTS group (n = 40) | |
| 190 mm | 2 (5%) |
| 225 mm | 11 (27.5%) |
| 265 mm | 15 (37.5%) |
| 305 mm | 11 (27.5%) |
| 345 mm | 1 (2.5%) |
| CCS group (n = 38) | |
| 203 mm | 17 (44.7%) |
| 254 mm | 21 (55.3%) |
| Clinical Results | CNCCS (N = 38) | TNTS (N = 40) | Signification |
|---|---|---|---|
| Length of stay | 19.9 ± 2.1 | 21.5 ± 2.1 | p = 0.586 |
| Blood loss (g/dL) | 4.7 ± 1.5 | 4.4 ± 1.1 | p = 0.459 |
| Bone grafting (n) | 16 (42.1%) | 19 (47.5%) | p = 0.632 |
| Need for ETO (n) | 11 (28.9%) | 11 (27.5%) | p = 0.840 |
| 2-stage revision (n) | 2 (5.3%) | 3 (7.5%) | p = 0.687 |
| Intraoperative periprosthetic fracture (n) | 6 (15.7%) | 8 (20%) | p = 0.535 |
| Post-op complications (n) | p = 0.658 | ||
| Dislocation | 3 (7.9%) | 3 (7.5%) | |
| Infection | 1 (2.6%) | 3 (7.5%) | |
| Periprosthetic fracture | 0 | 1 (2.5%) | |
| New loosening | 3 (7.9%) | 3 (7.5%) | |
| Patient satisfaction (n) | p = 0.247 | ||
| Unsatisfied | 6 | 11 | |
| Fairly satisfied | 12 | 7 | |
| Completely satisfied | 20 | 21 |
| Radiolucencies by Gruen Zones at a Year of Follow-Up (n) | CNCCS (n = 38) | TNTS (n = 40) | Signification |
|---|---|---|---|
| Zone 1 | 14 | 5 | p = 0.012 * |
| Zone 2 | 4 | 2 | p = 0.360 |
| Zone 3 | 5 | 1 | p = 0.077 |
| Zone 4 | 5 | 1 | p = 0.077 |
| Zone 5 | 5 | 1 | p = 0.077 |
| Zone 6 | 3 | 2 | p = 0.602 |
| Zone 7 | 10 | 3 | p = 0.026 * |
| Zone 8 | 7 | 3 | p = 0.149 |
| Zone 9 | 4 | 1 | p = 0.149 |
| Zone 10 | 6 | 1 | p = 0.040 * |
| Zone 11 | 3 | 1 | p = 0.280 |
| Zone 12 | 3 | 1 | p = 0.280 |
| Zone 13 | 4 | 2 | p = 0.360 |
| Zone 14 | 13 | 4 | p = 0.010 * |
| Radiolucencies by Gruen Zones at the End of Follow-Up (n) | CNCCS (n = 38) | TNTS (n = 40) | Signification |
|---|---|---|---|
| Zone 1 | 15 | 7 | p = 0.042 * |
| Zone 2 | 6 | 5 | p = 0.744 |
| Zone 3 | 6 | 3 | p = 0.286 |
| Zone 4 | 5 | 2 | p = 0.233 |
| Zone 5 | 6 | 2 | p = 0.134 |
| Zone 6 | 4 | 3 | p = 0.691 |
| Zone 7 | 12 | 4 | p = 0.024 * |
| Zone 8 | 9 | 4 | p = 0.127 |
| Zone 9 | 7 | 2 | p = 0.075 |
| Zone 10 | 7 | 1 | p = 0.025 * |
| Zone 11 | 4 | 1 | p = 0.165 |
| Zone 12 | 3 | 2 | p = 0.643 |
| Zone 13 | 4 | 5 | p = 0.722 |
| Zone 14 | 15 | 6 | p = 0.020 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Mateo, J.M.; Orozco-Martínez, J.; Matas-Díaz, J.A.; Vaquero, F.J.; Sanz-Ruiz, P. Comparison of Cylindrical and Tapered Stem Designs for Femoral Revision Hip Arthroplasty. J. Clin. Med. 2024, 13, 1745. https://doi.org/10.3390/jcm13061745
Hernández-Mateo JM, Orozco-Martínez J, Matas-Díaz JA, Vaquero FJ, Sanz-Ruiz P. Comparison of Cylindrical and Tapered Stem Designs for Femoral Revision Hip Arthroplasty. Journal of Clinical Medicine. 2024; 13(6):1745. https://doi.org/10.3390/jcm13061745
Chicago/Turabian StyleHernández-Mateo, José María, Javier Orozco-Martínez, José Antonio Matas-Díaz, Francisco Javier Vaquero, and Pablo Sanz-Ruiz. 2024. "Comparison of Cylindrical and Tapered Stem Designs for Femoral Revision Hip Arthroplasty" Journal of Clinical Medicine 13, no. 6: 1745. https://doi.org/10.3390/jcm13061745
APA StyleHernández-Mateo, J. M., Orozco-Martínez, J., Matas-Díaz, J. A., Vaquero, F. J., & Sanz-Ruiz, P. (2024). Comparison of Cylindrical and Tapered Stem Designs for Femoral Revision Hip Arthroplasty. Journal of Clinical Medicine, 13(6), 1745. https://doi.org/10.3390/jcm13061745






