The Effect of Hydrostatic Pressure on Coronary Flow and Pressure-Based Indices of Coronary Stenosis Severity
Abstract
1. Introduction
2. Methods
2.1. Study Design
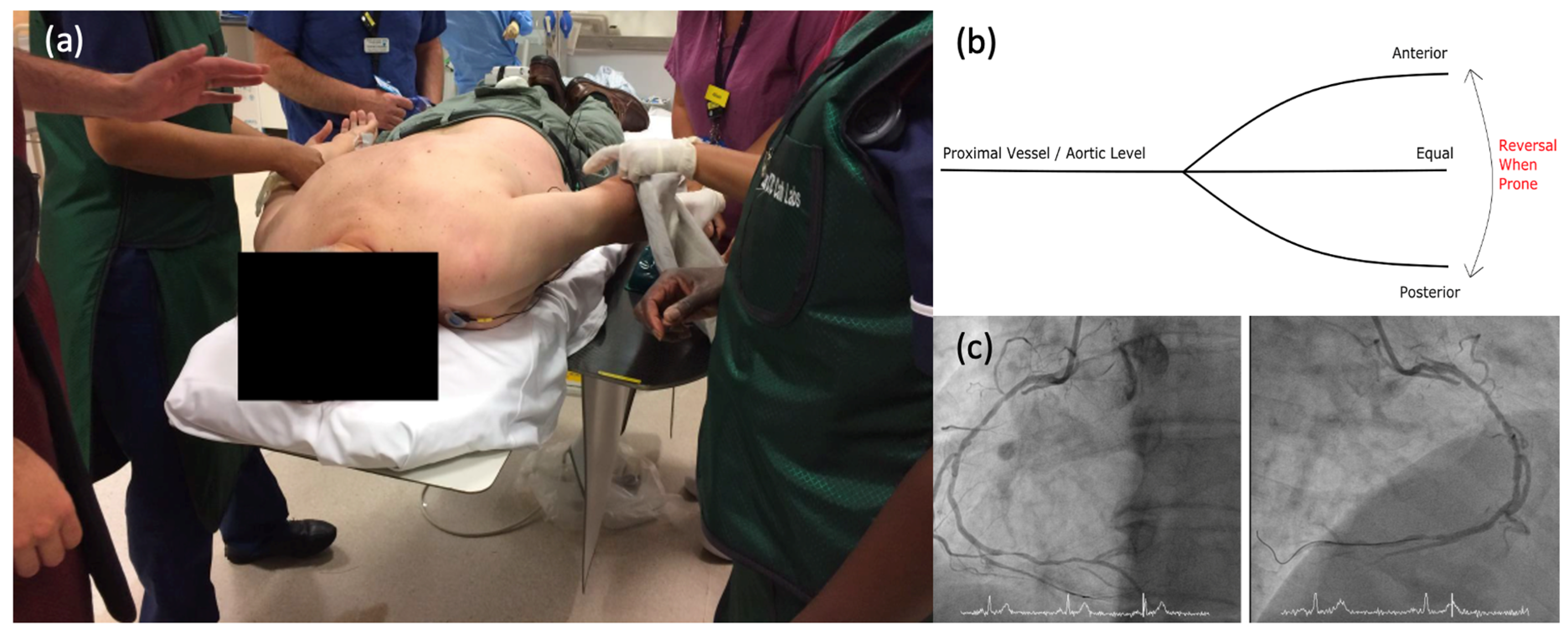
2.2. Catheterisation Protocol
2.3. Proximal Wire Position
2.4. Data Analysis
2.5. Change in Ischaemia Classification
2.6. Stenosis Severity
2.7. Statistical Analysis
3. Results
3.1. Pressure-Based Indices of Stenosis Severity
3.1.1. Pd/Pa
3.1.2. Instantaneous Wave Free Ratio (iFR)
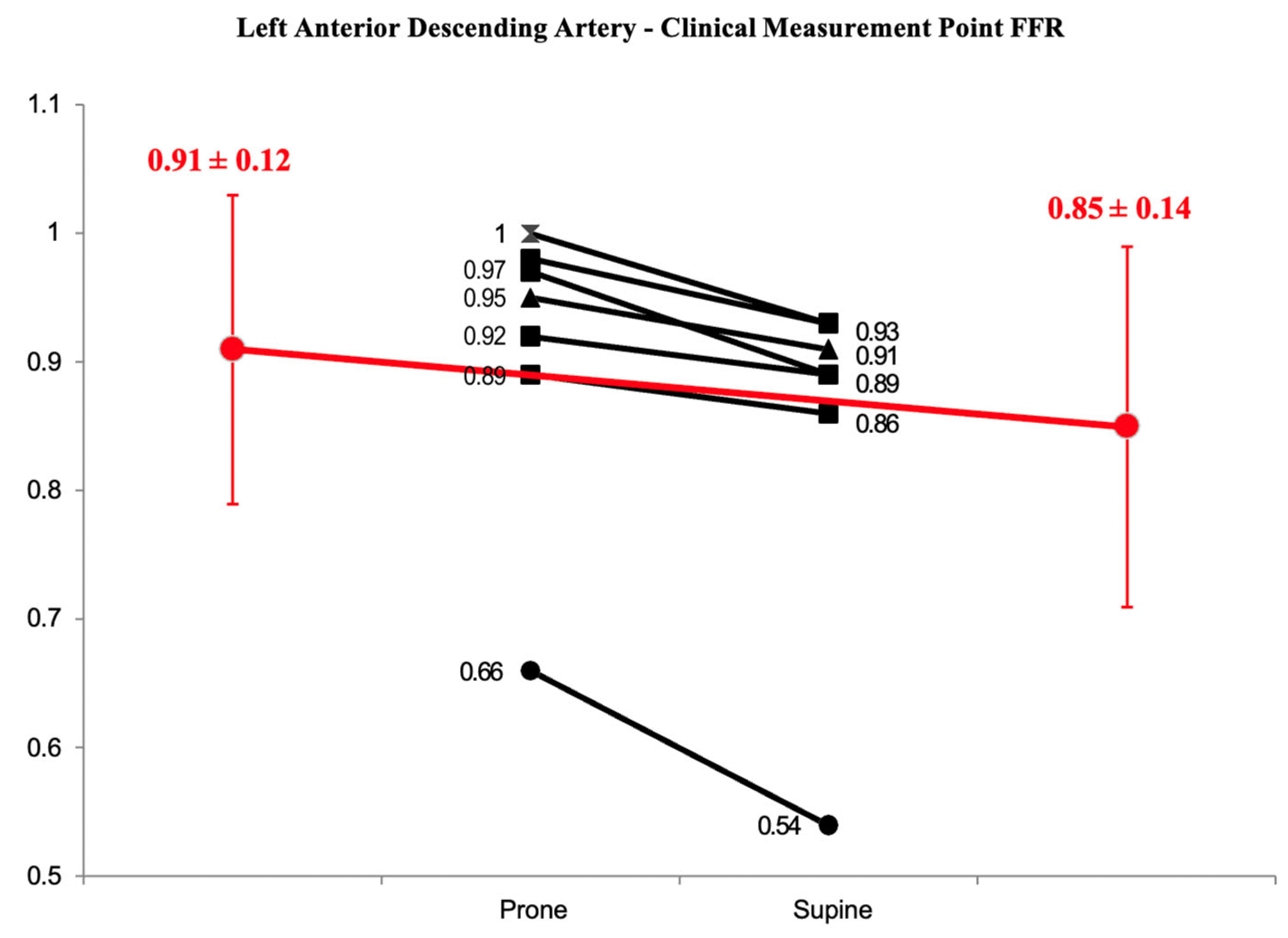
3.1.3. Fractional Flow Reserve (FFR)
3.2. Proximal Wire Position
3.3. Stenosis Re-Classification
3.4. Doppler Flow Measurements
4. Discussion
- There was a statistically significant difference in pressure-based indices across the same stenosis when comparing prone to supine patient measurements.
- The inferior artery position (i.e., Cx and RCA–PLV) produced statistically higher Pd/Pa, iFR, and FFR values compared to the superior artery position (i.e., LAD and RCA–PDA).
- Using a binary cut-off, approximately one-third of iFR and one-fourth of FFR measurements were re-classified across an ischaemic threshold due to a change in patient position.
- Doppler flow velocity did not change when prone and supine positions were compared.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/ EACTS guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [PubMed]
- Pijls, N.H.; De Bruyne, B.; Peels, K.; Van Der Voort, P.H.; Bonnier, H.J.; Bartunek, J.; Koolen, J.J. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N. Engl. J. Med. 1996, 334, 1703–1708. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.E.; Sen, S.; Dehbi, H.-M.; Al-Lamee, R.; Petraco, R.; Nijjer, S.S.; Bhindi, R.; Lehman, S.J.; Walters, D.; Sapontis, J.; et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N. Engl. J. Med. 2017, 376, 1824–1834. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.P.; Johnson, D.T.; Kirkeeide, R.L.; Berry, C.; De Bruyne, B.; Fearon, W.F.; Oldroyd, K.G.; Pijls, N.H.; Gould, K.L. Repeatability of fractional flow reserve despite variations in systemic and coronary hemodynamics. JACC Cardiovasc. Interv. 2015, 8, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Seto, A.H.; Tehrani, D.; Kern, M.J. Limitations and Pitfalls of Fractional Flow Reserve Measurements and Adenosine-Induced Hyperemia. Interv. Cardiol. Clin. 2015, 4, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Paradies, V.; Smits, P.C. The Influence of Hydrostatic Pressure on Physiological Indexes. Cardiovasc. Revascularization Med. 2023, 52, 106–107. [Google Scholar] [CrossRef] [PubMed]
- Al-Janabi, F.; Karamasis, G.; Cook, C.M.; Kabir, A.M.; Jagathesan, R.O.; Robinson, N.M.; Sayer, J.W.; Aggarwal, R.K.; Clesham, G.J.; Kelly, P.R.; et al. Coronary artery height differences and their effect on fractional flow reserve. Cardiol. J. 2021, 28, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Härle, T.; Luz, M.; Meyer, S.; Kronberg, K.; Nickau, B.; Escaned, J.; Davies, J.; Elsässer, A. Effect of Coronary Anatomy and Hydrostatic Pressure on Intracoronary Indices of Stenosis Severity. JACC Cardiovasc. Interv. 2017, 10, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.P.; Kirkeeide, R.L.; Gould, K.L. Hydrostatic forces. JACC Cardiovasc. Interv. 2017, 10, 1596–1597. [Google Scholar] [CrossRef] [PubMed]
- Härle, T.; Luz, M.; Meyer, S.; Vahldiek, F.; van der Harst, P.; van Dijk, R.; Ties, D.; Escaned, J.; Davies, J.; Elsässer, A. Influence of hydrostatic pressure on intracoronary indices of stenosis severity in vivo. Clin. Res. Cardiol. 2018, 107, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Ito, K.; Kin, H.; Shirai, Y.; Okazaki, A.; Miyajima, K.; Watanabe, T.; Tatsuguchi, M.; Wakabayashi, Y.; Maekawa, Y. Impact of hydrostatic pressure variations caused by height differences in supine and prone positions on fractional flow reserve values in the coronary circulation. J. Interv. Cardiol. 2019, 2019, 4532862. [Google Scholar] [CrossRef] [PubMed]
- Nagamatsu, S.; Sakamoto, K.; Yamashita, T.; Sato, R.; Tabata, N.; Motozato, K.; Yamanaga, K.; Ito, M.; Fujisue, K.; Kanazawa, H.; et al. Impact of hydrostatic pressure on fractional flow reserve: In vivo experimental study of anatomical height difference of coronary arteries. J. Cardiol. 2020, 76, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Üveges, Á.; Tar, B.; Jenei, C.; Czuriga, D.; Papp, Z.; Csanádi, Z.; Kőszegi, Z. The impact of hydrostatic pressure on the result of physiological measurements in various coronary segments. Int. J. Cardiovasc. Imaging 2021, 37, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Soh, M.S.; Kim, H.; Kang, M.G.; Lee, H.J.; Lee, S.D.; Hwang, S.J.; Hwang, J.-Y.; Kim, K.; Park, J.-R.; Kim, H.-R.; et al. Impact of height difference between coronary ostium and location of intracoronary pressure sensor on fractional flow reserve measurements. PLoS ONE 2023, 18, e0289646. [Google Scholar] [CrossRef] [PubMed]
- Florie, N.H.M.; Eerdekens, R.; Manzi, M.V.; Heinrichs, E.; van‘t Veer, M.; van Royen, N.; Tonino, P.A.L.; van Nunen, L.X. Potential effects of the hydrostatic pressure gradient on hyperemic and nonhyperemic pressure ratios. Am. J. Physiol. Heart Circ. Physiol. 2023, 325, H562–H568. [Google Scholar] [CrossRef] [PubMed]
- Nijjer, S.S.; de Waard, G.A.; Sen, S.; van de Hoef, T.P.; Petraco, R.; Echavarría-Pinto, M.; van Lavieren, M.A.; Meuwissen, M.; Danad, I.; Knaapen, P.; et al. Coronary pressure and flow relationships in humans: Phasic analysis of normal and pathological vessels and the implications for stenosis assessment: A report from the Iberian-Dutch-English (IDEAL) collaborators. Eur. Heart J. 2016, 37, 2069–2080. [Google Scholar] [CrossRef] [PubMed]
- Yokota, S.; Borren, N.M.; Ottervanger, J.P.; Mouden, M.; Timmer, J.R.; Knollema, S.; Jager, P.L. Does fractional flow reserve overestimate severity of LAD lesions? J. Nucl. Cardiol. 2020, 27, 1306–1313. [Google Scholar] [CrossRef] [PubMed]
- Muller, O.; Mangiacapra, F.; Ntalianis, A.; Verhamme, K.M.; Trana, C.; Hamilos, M.; Bartunek, J.; Vanderheyden, M.; Wyffels, E.; Heyndrickx, G.R.; et al. Long-term follow-up after fractional flow reserve-guided treatment strategy in patients with an isolated proximal left anterior descending coronary artery stenosis. JACC Cardiovasc. Interv. 2011, 4, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Jeremias, A.; Kirtane, A.J.; Stone, G.W. A Test in Context: Fractional Flow Reserve: Accuracy, Prognostic Implications, and Limitations. J. Am. Coll. Cardiol. 2017, 69, 2748–2758. [Google Scholar] [CrossRef] [PubMed]


| (%) | |
| Total Number | 23 (100) |
| Age | 63 ± 7 |
| Male | 23 (100) |
| Height (cm) | 174 ± 18 |
| Smoking | 1 (4) |
| Diabetes | 3 (13) |
| Hypertension | 10 (43) |
| Hypercholesterolaemia | 11 (48) |
| Family History of CAD | 2 (9) |
| Ejection Fraction | 52 ± 3 |
| Vessel (n) | Prone Pd/Pa Mean (±SD) | Supine Pd/Pa Mean (±SD) | Delta Change Mean (±SD) | p-Value |
|---|---|---|---|---|
| LAD (10) | 0.96 (0.07) | 0.88 (0.09) | 0.08 (0.04) | 0.0006 |
| Circumflex (7) | 0.93 (0.03) | 0.98 (0.02) | 0.05 (0.04) | 0.009 |
| RCA–PDA (2) | 0.93 (0.03) | 0.91 (0.06) | 0.02 (0.02) | |
| RCA–PLV (4) | 0.91 (0.07) | 0.98 (0.02) | 0.07 (0.05) | 0.032 |
| All (±SD) (23) | - | - | 0.05 (0.04) | <0.0001 |
| Vessel (n) | Prone iFR Mean (±SD) | Supine iFR Mean (±SD) | Delta Change Mean (±SD) | p-Value |
|---|---|---|---|---|
| LAD (10) | 0.91 (0.16) | 0.85 (0.14) | 0.06 (0.07) | 0.02 |
| Circumflex (7) | 0.90 (0.05) | 0.97 (0.03) | 0.07 (0.04) | 0.01 |
| RCA-PDA (2) | 0.86 (0.09) | 0.85(0.11) | 0.01 (0.02) | |
| RCA-PLV (3) | 0.87 (0.10) | 0.94 (0.04) | 0.07 (0.07) | 0.19 |
| All (±SD) (22) | - | - | 0.06 (0.05) | <0.0001 |
| Vessel (n) | Prone FFR Mean (±SD) | Supine FFR Mean (±SD) | Delta Change Mean (±SD) | p-Value |
|---|---|---|---|---|
| LAD (10) | 0.86 (0.11) | 0.77 (0.14) | 0.09 (0.07) | 0.003 |
| Circumflex (7) | 0.82 (0.06) | 0.87 (0.07) | 0.05 (0.03) | 0.006 |
| RCA–PDA (2) | 0.75 (0.10) | 0.69(0.10) | 0.06 (0.02) | |
| RCA–PLV (4) | 0.82 (0.10) | 0.86 (0.08) | 0.04 (0.03) | 0.004 |
| All (±SD) (23) | - | - | 0.06 (0.04) | <0.0001 |
| Index | Total Number | N Crossing Threshold | % Crossing Threshold |
|---|---|---|---|
| iFR | 22 | 8 | 36% |
| FFR | 23 | 6 | 26% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Janabi, F.; Karamasis, G.V.; Cook, C.M.; Stathogiannis, K.; Khan, S.; Fawaz, S.; Sajjad, U.; Jagathesan, R.; Kelly, P.R.; Gamma, R.A.; et al. The Effect of Hydrostatic Pressure on Coronary Flow and Pressure-Based Indices of Coronary Stenosis Severity. J. Clin. Med. 2024, 13, 1649. https://doi.org/10.3390/jcm13061649
Al-Janabi F, Karamasis GV, Cook CM, Stathogiannis K, Khan S, Fawaz S, Sajjad U, Jagathesan R, Kelly PR, Gamma RA, et al. The Effect of Hydrostatic Pressure on Coronary Flow and Pressure-Based Indices of Coronary Stenosis Severity. Journal of Clinical Medicine. 2024; 13(6):1649. https://doi.org/10.3390/jcm13061649
Chicago/Turabian StyleAl-Janabi, Firas, Grigoris V. Karamasis, Christopher M. Cook, Konstantinos Stathogiannis, Sarosh Khan, Samer Fawaz, Uzma Sajjad, Rohan Jagathesan, Paul R. Kelly, Reto A. Gamma, and et al. 2024. "The Effect of Hydrostatic Pressure on Coronary Flow and Pressure-Based Indices of Coronary Stenosis Severity" Journal of Clinical Medicine 13, no. 6: 1649. https://doi.org/10.3390/jcm13061649
APA StyleAl-Janabi, F., Karamasis, G. V., Cook, C. M., Stathogiannis, K., Khan, S., Fawaz, S., Sajjad, U., Jagathesan, R., Kelly, P. R., Gamma, R. A., Tang, K. H., Clesham, G. J., Keeble, T. R., & Davies, J. R. (2024). The Effect of Hydrostatic Pressure on Coronary Flow and Pressure-Based Indices of Coronary Stenosis Severity. Journal of Clinical Medicine, 13(6), 1649. https://doi.org/10.3390/jcm13061649







