Risk Factors for Higher Postoperative Myocardial Injury in Minimally Invasive Mitral Valve Surgery Patients: A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Patients’ Care and Management
2.3. Data Collection and Definitions
2.4. Endpoint of the Study
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Higher Myocardial Injury versus Lower Myocardial Injury
3.3. Postoperative Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Laffey, J.G.; Boylan, J.F.; Cheng, D.C. The systemic inflammatory response to cardiac surgery: Implications for the anesthesiologist. Anesthesiology 2002, 97, 215–252. [Google Scholar]
- Paparella, D.; Guida, P.; Caparrotti, S.; Fanelli, V.; Martinelli, G.; Mazzei, V.; Zaccaria, S.; Bisceglia, L.; Scrascia, G. Myocardial damage influences short- and mid-term survival after valve surgery: A prospective multicenter study. J. Thorac. Cardiovasc. Surg. 2014, 148, 2373–2379.e1. [Google Scholar] [CrossRef] [PubMed]
- Lurati Buse, G.A.; Koller, M.T.; Grapow, M.; Bolliger, D.; Seeberger, M.; Filipovic, M. The prognostic value of troponin release after adult cardiac surgery—A meta-analysis. Eur. J. Cardiothorac. Surg. 2010, 37, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Devereaux, P.J.; Lamy, A.; Chan, M.T.V.; Allard, R.V.; Lomivorotov, V.V.; Landoni, G.; Zheng, H.; Paparella, D.; McGillion, M.H.; Belley-Cote, E.P.; et al. High-Sensitivity Troponin I after Cardiac Surgery and 30-Day Mortality. N. Engl. J. Med. 2022, 386, 827–836. [Google Scholar] [CrossRef]
- Grazioli, V.; Giroletti, L.; Graniero, A.; Albano, G.; Mazzoni, M.; Panisi, P.G.; Gerometta, P.; Anselmi, A.; Agnino, A. Comparative myocardial protection of endoaortic balloon versus external clamp in minimally invasive mitral valve surgery. J. Cardiovasc. Med. 2023, 24, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Agnino, A.; Lanzone, A.M.; Albertini, A.; Anselmi, A. Follow-Up of the Novel Free Margin Running Suture Technique for Mitral Valve Repair. Thorac. Cardiovasc. Surg. 2019, 67, 557–560. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Khuri, S.F.; Henderson, W.G.; DePalma, R.G.; Mosca, C.; Healey, N.A.; Kumbhani, D.J.; Participants in the VANSQIP. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann. Surg. 2005, 242, 326–341; discussion 341–343. [Google Scholar] [CrossRef] [PubMed]
- Roques, F.; Nashef, S.A.; Michel, P.; Gauducheau, E.; de Vincentiis, C.; Baudet, E.; Cortina, J.; David, M.; Faichney, A.; Gabrielle, F.; et al. Risk factors and outcome in European cardiac surgery: Analysis of the EuroSCORE multinational database of 19030 patients. Eur. J. Cardiothorac. Surg. 1999, 15, 816–822; discussion 816–823. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, W.R.; Edwards, F.H.; Schwartz, M.; Bero, J.W.; Clark, R.E.; Grover, F.L. Risk stratification for cardiac valve replacement. National Cardiac Surgery Database. Database Committee of The Society of Thoracic Surgeons. Ann. Thorac. Surg. 1999, 67, 943–951. [Google Scholar]
- Mauermann, E.; Bolliger, D.; Fassl, J.; Grapow, M.; Seeberger, E.E.; Seeberger, M.D.; Filipovic, M.; Lurati Buse, G.A.L. Postoperative High-Sensitivity Troponin and Its Association With 30-Day and 12-Month, All-Cause Mortality in Patients Undergoing On-Pump Cardiac Surgery. Anesth. Analg. 2017, 125, 1110–1117. [Google Scholar] [CrossRef]
- Nesher, N.; Alghamdi, A.A.; Singh, S.K.; Sever, J.Y.; Christakis, G.T.; Goldman, B.S.; Cohen, G.N.; Moussa, F.; Fremes, S.E. Troponin after cardiac surgery: A predictor or a phenomenon? Ann. Thorac. Surg. 2008, 85, 1348–1354. [Google Scholar] [CrossRef]
- Thielmann, M.; Massoudy, P.; Neuhauser, M.; Knipp, S.; Kamler, M.; Marggraf, G.; Piotrowski, J.; Jakob, H. Risk stratification with cardiac troponin I in patients undergoing elective coronary artery bypass surgery. Eur. J. Cardiothorac. Surg. 2005, 27, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology; American College of Cardiology; American Heart Association; et al. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef]
- Garcia-Garcia, H.M.; McFadden, E.P.; Farb, A.; Mehran, R.; Stone, G.W.; Spertus, J.; Onuma, Y.; Morel, M.A.; van Es, G.A.; Zuckerman, B.; et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Circulation 2018, 137, 2635–2650. [Google Scholar] [CrossRef] [PubMed]
- Kokofer, A.; Cozowicz, C.; Wernly, B.; Rodemund, N. Timing and threshold of high sensitive troponin T measurement for the prediction of mortality after cardiac surgery: A retrospective cohort analysis. Intensive Care Med. Exp. 2023, 11, 58. [Google Scholar] [CrossRef] [PubMed]
- Polzl, L.; Engler, C.; Sterzinger, P.; Lohmann, R.; Nagele, F.; Hirsch, J.; Graber, M.; Eder, J.; Reinstadler, S.; Sappler, N.; et al. Association of High-Sensitivity Cardiac Troponin T With 30-Day and 5-Year Mortality after Cardiac Surgery. J. Am. Coll. Cardiol. 2023, 82, 1301–1312. [Google Scholar] [CrossRef] [PubMed]
- Lazar, D.R.; Lazar, F.L.; Homorodean, C.; Cainap, C.; Focsan, M.; Cainap, S.; Olinic, D.M. High-Sensitivity Troponin: A Review on Characteristics, Assessment, and Clinical Implications. Dis. Markers 2022, 2022, 9713326. [Google Scholar] [CrossRef]
- Giustino, G.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Grayburn, P.A.; Kapadia, S.R.; Cohen, D.J.; Kotinkaduwa, L.N.; Weissman, N.J.; et al. NYHA Functional Classification and Outcomes After Transcatheter Mitral Valve Repair in Heart Failure: The COAPT Trial. JACC Cardiovasc. Interv. 2020, 13, 2317–2328. [Google Scholar] [CrossRef]
- Azman Ates, B.E. The effect of cross clamp time on Troponin I levels in patients undergoing coronary artery bypass grafting. East Afr. Sch. J. Med. Sci. 2019, 2, 175–179. [Google Scholar]
- Chambers, D.J.; Fallouh, H.B. Cardioplegia and cardiac surgery: Pharmacological arrest and cardioprotection during global ischemia and reperfusion. Pharmacol. Ther. 2010, 127, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Buckberg, G.D.; Athanasuleas, C.L. Cardioplegia: Solutions or strategies? Eur. J. Cardiothorac. Surg. 2016, 50, 787–791. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Zhang, X.; Cui, H.; Zhang, L.; Gong, Z.; Li, L.; Ren, T.; Gao, C.; Jiang, S. Comparison of clinical outcomes between robotic and thoracoscopic mitral valve repair. Cardiovasc. Diagn. Ther. 2020, 10, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Bonatti, J.; Kiaii, B.; Alhan, C.; Cerny, S.; Torregrossa, G.; Bisleri, G.; Komlo, C.; Guy, T.S. The role of robotic technology in minimally invasive surgery for mitral valve disease. Expert. Rev. Med. Devices 2021, 18, 955–970. [Google Scholar] [CrossRef] [PubMed]
- Husen, T.F.; Kohar, K.; Angelica, R.; Saputro, B.I.L. Robotic vs other surgery techniques for mitral valve repair and/or replacement: A systematic review and meta-analysis. Hellenic J. Cardiol. 2023, 71, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.B.; Mehaffey, J.H.; Mullen, M.G.; Nifong, W.L.; Chitwood, W.R.; Katz, M.R.; Quader, M.A.; Kiser, A.C.; Speir, A.M.; Ailawadi, G.; et al. A propensity matched analysis of robotic, minimally invasive, and conventional mitral valve surgery. Heart 2018, 104, 1970–1975. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Tauber, K.; Szeto, W.Y.; Hargrove, W.C.; Atluri, P.; Acker, M.; Crawford, T.; Ibrahim, M.E. Robotic and endoscopic mitral valve repair for degenerative disease. Ann. Cardiothorac. Surg. 2022, 11, 614–621. [Google Scholar] [CrossRef]
- Zheng, C.R.; Mazur, P.; Arghami, A.; Jahanian, S.; Viehman, J.K.; King, K.S.; Dearani, J.A.; Daly, R.C.; Rowse, P.G.; Bagameri, G.; et al. Robotic vs. minimally invasive mitral valve repair: A 5-year comparison of surgical outcomes. J. Card. Surg. 2022, 37, 3267–3275. [Google Scholar] [CrossRef]
- Bonatti, J.; Crailsheim, I.; Grabenwoger, M.; Winkler, B. Minimally Invasive and Robotic Mitral Valve Surgery: Methods and Outcomes in a 20-Year Review. Innovations 2021, 16, 317–326. [Google Scholar] [CrossRef]
- Palmen, M.; Navarra, E.; Bonatti, J.; Franke, U.; Cerny, S.; Musumeci, F.; Modi, P.; Singh, S.; Sandoval, E.; Pettinari, M.; et al. Current state of the art and recommendations in robotic mitral valve surgery. Interact. Cardiovasc. Thorac. Surg. 2022, 35, ivac160. [Google Scholar] [CrossRef]
| Overall (n = 316) | Higher Myocardial Injury (n = 48) | Lower Myocardial Injury (n = 268) | p Values | |
|---|---|---|---|---|
| Age, years | 63 [53–71] | 65 [56–73] | 63 [52–71] | 0.37 |
| Female sex, n (%) | 118 (37) | 22 (46) | 96 (36) | 0.20 |
| BMI | 24.5 [22.1–26.6] | 23.9 [22.5–25.8] | 24.6 [22.1–26.6] | 0.84 |
| Preoperative Characteristics | ||||
| Atrial Fibrillation, n (%) | 60 (19) | 11 (23) | 49 (18) | 0.43 |
| Mitral Valve Stenosis, n (%) | 10 (3) | 3 (6) | 7 (3) | 0.18 |
| Arterial Hypertension, n (%) | 183 (58) | 32 (66) | 151 (56) | 0.21 |
| Chronic Arteriopathy, n (%) | 4 (1) | - | 4 (2) | 1.00 |
| Diabetes, n (%) | 15 (5) | 3 (6) | 12 (5) | 0.71 |
| Neurologic Disease, n (%) | 29 (9) | 3 (6) | 26 (10) | 0.59 |
| Asthma/COPD, n (%) | 26 (8) | 4 (8) | 22 (8) | 1.00 |
| Preoperative Hemoglobin | 14.1 [13.1–15.0] | 14.1 [13.2–14.9] | 14.1 [13.0–15.0] | 0.94 |
| Preoperative Creatinine | 0.90 [0.80–1.07] | 0.86 [0.73–0.99] | 0.91 [0.81–1.07] | 0.10 |
| EuroSCORE II, score | 0.92 [0.67–1.32] | 0.96 [0.63–2.19] | 0.90 [0.67–1.25] | 0.15 |
| LV Ejection Fraction, (%) | 62 [60–66] | 60 [59–65] | 62 [60–67] | 0.33 |
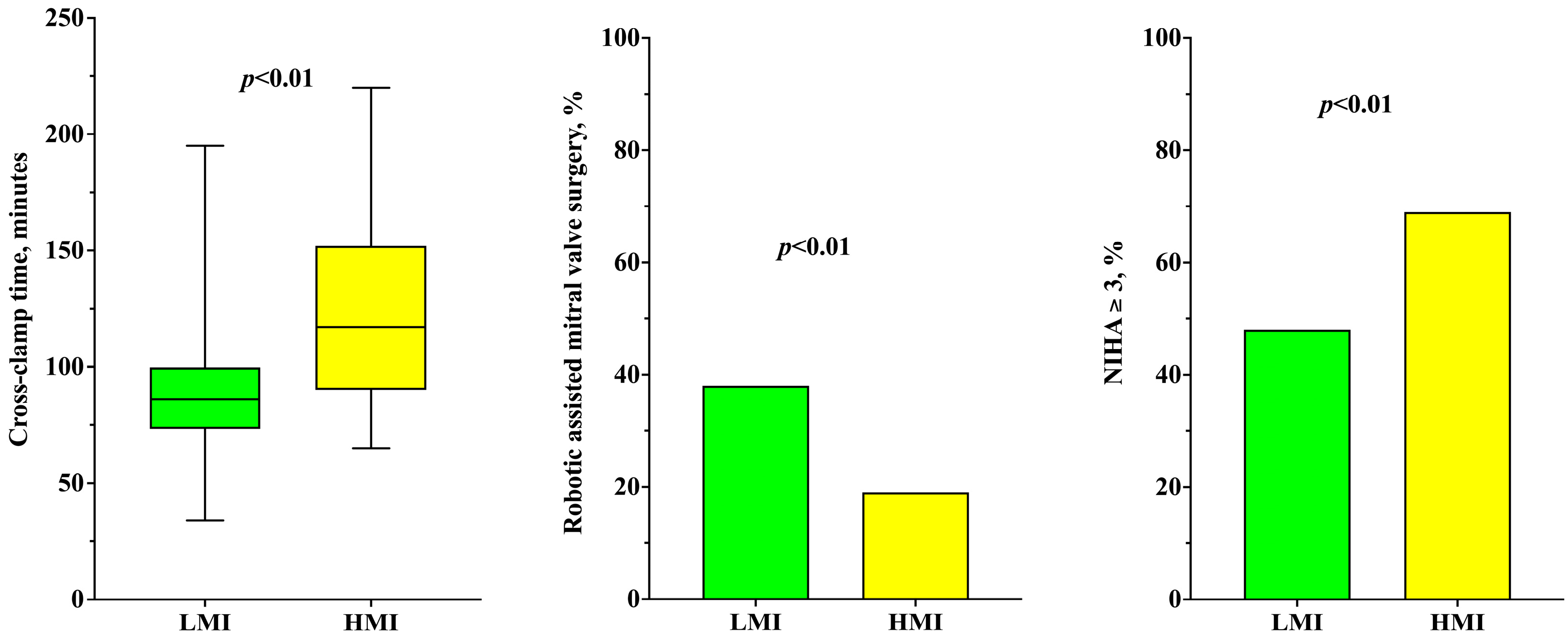
| NYHA class ≥ 3, n (%) | 161 (51) | 33 (69) | 128 (48) | <0.01 |
| Intraoperative Characteristics | ||||
| Robotic-Assisted Mitral Valve surgery, n (%) | 111 (35) | 9 (19) | 102 (38) | 0.01 |
| Mitral Valve Replacement, n (%) | 16 (5) | 6 (13) | 10 (4) | 0.02 |
| Cardiopulmonary bypass time, min | 139 [118–167] | 167 [134–209] | 135 [115–164] | <0.01 |
| Cross-clamp time, min | 87 [75–104] | 117 [91–145] | 86 [74–100] | <0.01 |
| Operative time, min | 230 [200–265] | 266 [218–313] | 223 [200–256] | <0.01 |
| IABP, n (%) | 2 (1) | 1 (2) | 1 (1) | 0.28 |
| Postoperative Characteristics | ||||
| Bleeding at 24 h, mL | 340 [250–495] | 405 [265–540] | 330 [250–480] | 0.06 |
| Highest Lactate at 24 h, mmol/L | 2.9 [2.0–4.4] | 4.0 [2.6–6.7] | 2.7 [2.0–4.1] | <0.01 |
| ICU Transfusions, n (%) | 58 (18) | 11 (23) | 47 (18) | 0.42 |
| Surgical Revision, n (%) | 12 (4) | 3 (6) | 9 (3) | 0.40 |
| Postoperative AF, n (%) | 73 (23) | 10 (21) | 63 (24) | 0.85 |
| Postoperative AKI, n (%) | 21 (7) | 8 (17) | 13 (5) | <0.01 |
| Postoperative PCI, n (%) | 2 (1) | 2 (4) | - | 0.02 |
| LVEF at discharge, % | 58 [55–60] | 57 [55–60] | 58 [54–60] | 0.74 |
| MV time, hours | 5 [3–8] | 6 [4–11] | 5 [3–7] | <0.01 |
| ICU stay, hours | 44 [40–48] | 45 [42–67] | 44 [39–47] | 0.06 |
| Postoperative Length of Stay, days | 9 [7–11] | 10 [8–11] | 8 [7–10] | <0.01 |
| In-hospital Mortality, n (%) | - | - | - | - |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Unadjusted OR [CI 95%] | p Value | Adjusted OR [CI 95%] | p Value | |
| Age, years | 1.01 [0.98–1.04] | 0.33 | ||
| Female sex, n (%) | 1.51 [0.81–2.82] | 0.19 | ||
| BMI | 1.00 [0.92–1.08] | 0.99 | ||
| Atrial Fibrillation, n (%) | 0.75 [0.36–1.58] | 0.45 | ||
| Mitral Valve Stenosis, n (%) | 0.40 [0.10–1.61] | 0.20 | ||
| Arterial Hypertension, n (%) | 0.65 [0.34–1.23] | 0.18 | ||
| Diabetes, n (%) | 0.70 [0.19–2.59] | 0.60 | ||
| Neurologic Disease, n (%) | 1.61 [0.47–5.55] | 0.45 | ||
| Asthma/COPD, n (%) | 0.98 [0.32–2.99] | 0.98 | ||
| Preoperative Hemoglobin | 1.02 [0.83–1.24] | 0.88 | ||
| Preoperative Creatinine | 0.37 [0.10–1.30] | 0.12 | ||
| EuroSCORE II, score | 1.38 [1.08–1.79] | 0.01 | 1.22 [0.87–1.70] | 0.24 |
| LV Ejection Fraction, (%) | 0.99 [0.94–1.04] | 0.57 | ||
| NYHA class ≥ 3, n (%) | 2.41 [1.24–4.64] | <0.01 | 2.33 [1.04–5.22] | 0.04 |
| Robotic-Assisted Mitral Valve surgery, n (%) | 0.38 [0.18–0.81] | 0.01 | 0.36 [0.14–0.90] | 0.03 |
| Mitral Valve Replacement, n (%) | 3.86 [1.33–11.19] | 0.01 | 2.36 [0.63–8.93] | 0.21 |
| Cardiopulmonary bypass time, min | 1.02 [1.01–1.02] | <0.01 | ||
| Cross-clamp time, min | 1.05 [1.03–1.06] | <0.01 | 1.05 [1.03–1.06] | <0.01 |
| Operative time, min | 1.02 [1.01–1.02] | <0.01 | ||
| IABP, n (%) | 0.18 [0.01–2.86] | 0.22 | ||
| Overall (n = 316) | Higher Myocardial Injury (n = 48) | Lower Myocardial Injury (n = 268) | p Values | |
|---|---|---|---|---|
| Troponin day 1, ng/L | 4071 [2810–6518] | 12,424 [7815–20,271] | 3555 [2677–4918] | <0.01 |
| Troponin day 2, ng/L | 2124 [1472–3332] | 6221 [3884–9311] | 1872 [1347–2780] | <0.01 |
| Troponin day 3, ng/L | 1032 [687–1728] | 3666 [1819–6200] | 908 [640–1345] | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baccanelli, F.; Albano, G.; Carrara, A.; Parrinello, M.; Roscitano, C.; Cecconi, M.; Gerometta, P.; Graniero, A.; Agnino, A.; Peluso, L. Risk Factors for Higher Postoperative Myocardial Injury in Minimally Invasive Mitral Valve Surgery Patients: A Cohort Study. J. Clin. Med. 2024, 13, 1591. https://doi.org/10.3390/jcm13061591
Baccanelli F, Albano G, Carrara A, Parrinello M, Roscitano C, Cecconi M, Gerometta P, Graniero A, Agnino A, Peluso L. Risk Factors for Higher Postoperative Myocardial Injury in Minimally Invasive Mitral Valve Surgery Patients: A Cohort Study. Journal of Clinical Medicine. 2024; 13(6):1591. https://doi.org/10.3390/jcm13061591
Chicago/Turabian StyleBaccanelli, Federica, Giovanni Albano, Alfonso Carrara, Matteo Parrinello, Claudio Roscitano, Maurizio Cecconi, Piersilvio Gerometta, Ascanio Graniero, Alfonso Agnino, and Lorenzo Peluso. 2024. "Risk Factors for Higher Postoperative Myocardial Injury in Minimally Invasive Mitral Valve Surgery Patients: A Cohort Study" Journal of Clinical Medicine 13, no. 6: 1591. https://doi.org/10.3390/jcm13061591
APA StyleBaccanelli, F., Albano, G., Carrara, A., Parrinello, M., Roscitano, C., Cecconi, M., Gerometta, P., Graniero, A., Agnino, A., & Peluso, L. (2024). Risk Factors for Higher Postoperative Myocardial Injury in Minimally Invasive Mitral Valve Surgery Patients: A Cohort Study. Journal of Clinical Medicine, 13(6), 1591. https://doi.org/10.3390/jcm13061591







