Risk Factors for Cervical Disc Arthroplasty Subsidence with Bryan Disc—A Retrospective Observational Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
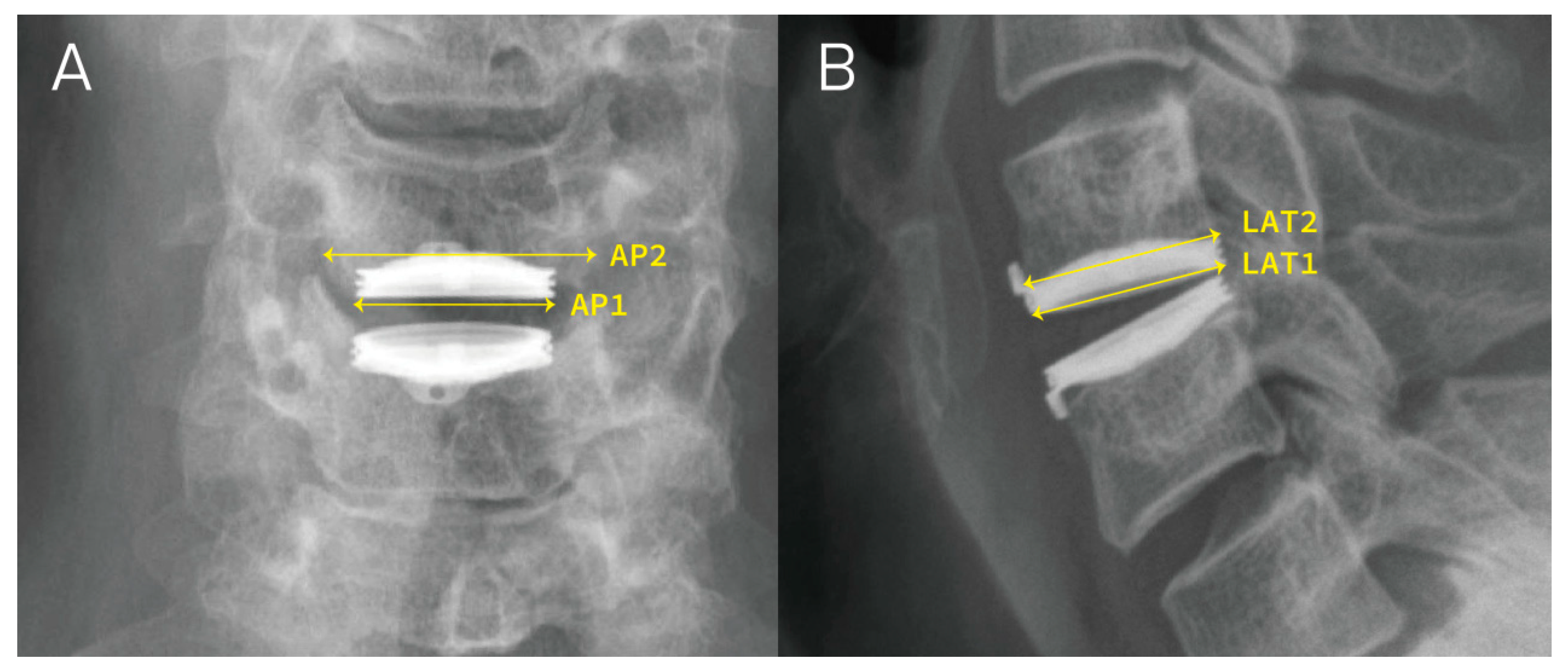
2.2. Radiographic Evaluation
2.3. Calculation
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, G.W.; Robinson, R.A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J. Bone Joint Surg. Am. 1958, 40, 607–624. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, M.M.; Mobbs, R.J.; Hogan, J.; Zhao, D.F.; Rao, P.J.; Phan, K. Anterior cervical disc arthroplasty (ACDA) versus anterior cervical discectomy and fusion (ACDF): A systematic review and meta-analysis. J. Spine Surg. 2015, 1, 72–85. [Google Scholar] [PubMed]
- Gornet, M.F.; Lanman, T.H.; Burkus, J.K.; Hodges, S.D.; McConnell, J.R.; Dryer, R.F.; Copay, A.G.; Nian, H.; Harrell, F.E. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: Results of a prospective, multicenter randomized controlled clinical trial at 24 months. J. Neurosurg. Spine 2017, 26, 653–667. [Google Scholar] [CrossRef] [PubMed]
- Eck, J.C.; Humphreys, S.C.; Lim, T.H.; Jeong, S.T.; Kim, J.G.; Hodges, S.D.; An, H.S. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 2002, 27, 2431–2434. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Kim, K.H.; Kuh, S.U.; Chin, D.K.; Kim, K.S.; Cho, Y.E. What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT. Eur. Spine J. 2013, 22, 1078–1089. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Okada, E.; Ichihara, D.; Watanabe, K.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Iwanami, A.; et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: Comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine 2010, 35, 36–43. [Google Scholar] [CrossRef]
- Zavras, A.G.; Sullivan, T.B.; Singh, K.; Phillips, F.M.; Colman, M.W. Failure in cervical total disc arthroplasty: Single institution experience, systematic review of the literature, and proposal of the RUSH TDA failure classification system. Spine J. 2022, 22, 353–369. [Google Scholar] [CrossRef]
- Anderson, P.A.; Rouleau, J.P. Intervertebral disc arthroplasty. Spine 2004, 29, 2779–2786. [Google Scholar] [CrossRef]
- Phillips, F.M.; Geisler, F.H.; Gilder, K.M.; Reah, C.; Howell, K.M.; McAfee, P.C. Long-term Outcomes of the US FDA IDE Prospective, Randomized Controlled Clinical Trial Comparing PCM Cervical Disc Arthroplasty with Anterior Cervical Discectomy and Fusion. Spine 2015, 40, 674–683. [Google Scholar] [CrossRef]
- Lavelle, W.F.; Riew, K.D.; Levi, A.D.; Florman, J.E. Ten-year Outcomes of Cervical Disc Replacement with the BRYAN Cervical Disc: Results from a Prospective, Randomized, Controlled Clinical Trial. Spine 2019, 44, 601–608. [Google Scholar] [CrossRef]
- Radcliff, K.; Davis, R.J.; Hisey, M.S.; Nunley, P.D.; Hoffman, G.A.; Jackson, R.J.; Bae, H.W.; Albert, T.; Coric, D. Long-term Evaluation of Cervical Disc Arthroplasty with the Mobi-C© Cervical Disc: A Randomized, Prospective, Multicenter Clinical Trial with Seven-Year Follow-up. Int. J. Spine Surg. 2017, 11, 31. [Google Scholar] [CrossRef]
- Pickett, G.E.; Sekhon, L.H.; Sears, W.R.; Duggal, N. Complications with cervical arthroplasty. J. Neurosurg. Spine 2006, 4, 98–105. [Google Scholar] [CrossRef]
- Walraevens, J.; Demaerel, P.; Suetens, P.; Van Calenbergh, F.; van Loon, J.; Sloten, J.V.; Goffin, J. Longitudinal prospective long-term radiographic follow-up after treatment of single-level cervical disk disease with the Bryan Cervical Disc. Neurosurgery 2010, 67, 679–687; discussion 87. [Google Scholar] [CrossRef] [PubMed]
- Berg, A.; Killen, M.-C.; Khan, S.; Reddy, G.; Friesem, T. Subsidence in Single Level Cervical Disc Arthroplasty. Glob. Spine J. 2015, 5 (Suppl. S1), s-0035-1554496. [Google Scholar] [CrossRef]
- Hacker, F.M.; Babcock, R.M.; Hacker, R.J. Very late complications of cervical arthroplasty: Results of 2 controlled randomized prospective studies from a single investigator site. Spine 2013, 38, 2223–2226. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.Y.; Chen, W.H.; Tzeng, C.Y.; Huang, C.-W.; Yang, C.-C.; Chen, H.-T.; Chang, C.-C.; Lee, C.-Y.; Tsou, H.-K. Anterior bone loss after cervical Bryan disc arthroplasty: Insight into the biomechanics following total disc replacement. Spine J. 2020, 20, 1211–1218. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.W.; Tsou, H.K.; Chen, W.H.; Tsai, J.-C.; Chung, K.-C.; Lin, R.-H.; Chen, T.-Y.; Tzeng, C.-Y. The residual exposed endplate ratio is predictive of posterior heterotopic ossification after cervical Bryan disc arthroplasty. J. Clin. Neurosci. 2023, 114, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.; Beutler, W.; Peppelman, W.; Marzluff, J.; Mugglin, A.; Ramakrishnan, P.S.; Myer, J.; Baker, K.J. Long-Term Clinical Experience with Selectively Constrained SECURE-C Cervical Artificial Disc for 1-Level Cervical Disc Disease: Results from Seven-Year Follow-up of a Prospective, Randomized, Controlled Investigational Device Exemption Clinical Trial. Int. J. Spine Surg. 2018, 12, 377–387. [Google Scholar] [CrossRef]
- Mende, K.C.; Eicker, S.O.; Weber, F. Cage deviation in the subaxial cervical spine in relation to implant position in the sagittal plane. Neurosurg. Rev. 2018, 41, 267–274. [Google Scholar] [CrossRef]
- Karikari, I.O.; Jain, D.; Owens, T.R.; Gottfried, O.; Hodges, T.R.; Nimjee, S.M.; Bagley, C.A. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: A systematic review. J. Spinal Disord. Tech. 2014, 27, 1–10. [Google Scholar] [CrossRef]
- Opsenak, R.; Hanko, M.; Snopko, P.; Varga, K.; Kolarovszki, B. Subsidence of anchored cage after anterior cervical discectomy. Bratisl. Lek. Listy. 2019, 120, 356–361. [Google Scholar] [CrossRef]
- Godlewski, B.; Bebenek, A.; Dominiak, M.; Karpinski, G.; Cieslik, P.; Pawelczyk, T. Subsidence following cervical discectomy and implant-to-bone ratio. BMC Musculoskelet. Disord. 2022, 23, 750. [Google Scholar] [CrossRef]
- Kao, T.H.; Wu, C.H.; Chou, Y.C.; Chen, H.T.; Chen, W.H.; Tsou, H.K. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: A review of 82 cases and 182 levels. Arch. Orthop. Trauma. Surg. 2014, 134, 1343–1351. [Google Scholar] [CrossRef]
- Parish, J.M.; Asher, A.M.; Coric, D. Complications and Complication Avoidance with Cervical Total Disc Replacement. Int. J. Spine Surg. 2020, 14, S50–S56. [Google Scholar] [CrossRef]
- Wu, W.J.; Jiang, L.S.; Liang, Y.; Dai, L.Y. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: A retrospective study. Eur. Spine J. 2012, 21, 1374–1382. [Google Scholar] [CrossRef]
- Brenke, C.; Dostal, M.; Scharf, J.; Weiß, C.; Schmieder, K.; Barth, M. Influence of cervical bone mineral density on cage subsidence in patients following stand-alone anterior cervical discectomy and fusion. Eur. Spine J. 2015, 24, 2832–2840. [Google Scholar] [CrossRef]
- Wenger, M.; Markwalder, T.M. Bryan total disc arthroplasty: A replacement disc for cervical disc disease. Med. Devices 2010, 3, 11–24. [Google Scholar] [CrossRef] [PubMed]
- de Kleuver, M.; Oner, F.C.; Jacobs, W.C. Total disc replacement for chronic low back pain: Background and a systematic review of the literature. Eur. Spine J. 2003, 12, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Bertagnoli, R.; Kumar, S. Indications for full prosthetic disc arthroplasty: A correlation of clinical outcome against a variety of indications. Eur. Spine J. 2002, 11 (Suppl. S2), S131–S136. [Google Scholar] [CrossRef]
- Griffith, S.L.; Shelokov, A.P.; Büttner-Janz, K.; LeMaire, J.P.; Zeegers, W.S. A multicenter retrospective study of the clinical results of the LINK SB Charité intervertebral prosthesis. The initial European experience. Spine 1994, 19, 1842–1849. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K. Osteopenia and total disc prosthesis subsidence: Inclusion/exclusion criteria for total disc replacement. SAS J. 2007, 1, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Ganau, M.; Fehlings, M.G. Surgical decision-making in degenerative cervical myelopathy-Anterior versus posterior approach. J. Clin. Neurosci. 2018, 58, 7–12. [Google Scholar] [CrossRef] [PubMed]



| No Subsidence | Subsidence | Total | p Value | ||||
|---|---|---|---|---|---|---|---|
| Participants | 86 | 18 | 104 | ||||
| CDA numbers, n | 118 | 35 | 153 | ||||
| Sex | 1.000 | ||||||
| Female | 43 | (50.0%) | 9 | (50.0%) | 52 | (50.0%) | |
| Male | 43 | (50.0%) | 9 | (50.0%) | 52 | (50.0%) | |
| Age, years | 49.00 | (43.00, 54.25) | 49.00 | (43.25, 55.00) | 49.00 | (43.00, 54.75) | 0.976 |
| Smoking, n | 26 | (30.2%) | 5 | (27.8%) | 31 | (29.8%) | 1.000 |
| Follow-up period, months | 43.50 | (16.50, 75.75) | 71.00 | (48.00, 135.50) | 51.00 | (20.75, 89.75) | 0.007 ** |
| Operative levels | 0.597 | ||||||
| Single level cases | 47 | (54.7%) | 8 | (44.4%) | 55 | (52.9%) | |
| Two level cases | 39 | (45.3%) | 10 | (55.6%) | 49 | (47.1%) | |
| Segments | 0.594 | ||||||
| Single level | 47 | (37.3%) | 8 | (29.6%) | 55 | (35.9%) | |
| Two level | 79 | (62.7%) | 19 | (70.4%) | 98 | (64.1%) | |
| C3–C4 | 11 | (8.7%) | 2 | (7.4%) | 13 | (8.5%) | 1.000 |
| C4–C5 | 38 | (30.2%) | 6 | (22.2%) | 44 | (28.8%) | 0.553 |
| C5–C6 | 68 | (54.0%) | 15 | (55.6%) | 83 | (54.2%) | 1.000 |
| C6–C7 | 9 | (7.1%) | 4 | (14.8%) | 13 | (8.5%) | 0.247 |
| pre-OP Mean-DH | 5.36 | (5.19, 5.52) | 4.0 | (3.7, 4.3) | 5.05 | (4.88, 5.22) | <0.001 ** |
| ΔAP, mm | 0.17 | (0.15, 0.19) | 0.21 | (0.16, 0.25) | 0.18 | (0.16, 0.19) | 0.056 |
| ΔLat, mm | 0.14 | (0.12, 0.16) | 0.14 | (0.1, 0.19) | 0.14 | (0.12, 0.16) | 0.970 |
| ΔDH, mm | 0.59 | (0.57, 0.61) | 0.67 | (0.62, 0.72) | 0.61 | (0.59, 0.63) | 0.002 ** |
| AP ratio | 0.92 | (0.91, 0.92) | 0.9 | (0.88, 0.92) | 0.91 | (0.91, 0.92) | 0.075 |
| Lat ratio | 0.94 | (0.93, 0.95) | 0.94 | (0.92, 0.96) | 0.94 | (0.93, 0.95) | 0.917 |
| BMD | 1.136 | (1.09, 1.16) | 0.998 | (0.96, 1.03) | 1.13 | (1.05, 1.15) | 0.072 |
| T score | 0.3 | (0.05, 0.35) | −1 | (−1.21, −0.75) | 0.1 | (−0.6, 0.3) | 0.064 |
| Simple Regression | Multiple Regression (Forward) | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Age | 1.003 | (0.948, 1.061) | 0.916 | |||
| Gender | 1.127 | (0.432, 2.938) | 0.807 | |||
| Smoking | 0.814 | (0.292, 2.265) | 0.693 | |||
| pre-OP Mean-DH | 0.186 | (0.103, 0.336) | <0.001 ** | 0.151 | (0.059, 0.391) | <0.001 ** |
| ΔAP-mm | 35.557 | (0.862, 1467.464) | 0.06 | |||
| ΔLat-mm | 1.059 | (0.056, 20.097) | 0.969 | |||
| ΔDH-mm | 2.616 | (1.707, 4.011) | <0.001 ** | 0.797 | (0.395, 1.61) | 0.528 |
| AP ratio | 0.001 | (0, 2.301) | 0.078 | |||
| Lat ratio | 0.66 | (0, 1470.868) | 0.916 | |||
| Contact footprint of implant | 0.016 | (0, 6.824) | 0.18 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-Y.; Tung, K.-K.; Tsou, H.-K.; Chen, W.-H.; Tzeng, C.-Y.; Lin, R.-H.; Chen, T.-Y.; Huang, C.-W.; Kao, T.-H. Risk Factors for Cervical Disc Arthroplasty Subsidence with Bryan Disc—A Retrospective Observational Analysis. J. Clin. Med. 2024, 13, 1589. https://doi.org/10.3390/jcm13061589
Lee C-Y, Tung K-K, Tsou H-K, Chen W-H, Tzeng C-Y, Lin R-H, Chen T-Y, Huang C-W, Kao T-H. Risk Factors for Cervical Disc Arthroplasty Subsidence with Bryan Disc—A Retrospective Observational Analysis. Journal of Clinical Medicine. 2024; 13(6):1589. https://doi.org/10.3390/jcm13061589
Chicago/Turabian StyleLee, Cheng-Ying, Kuan-Kai Tung, Hsi-Kai Tsou, Wen-Hsien Chen, Chung-Yuh Tzeng, Ruei-Hong Lin, Tse-Yu Chen, Chih-Wei Huang, and Ting-Hsien Kao. 2024. "Risk Factors for Cervical Disc Arthroplasty Subsidence with Bryan Disc—A Retrospective Observational Analysis" Journal of Clinical Medicine 13, no. 6: 1589. https://doi.org/10.3390/jcm13061589
APA StyleLee, C.-Y., Tung, K.-K., Tsou, H.-K., Chen, W.-H., Tzeng, C.-Y., Lin, R.-H., Chen, T.-Y., Huang, C.-W., & Kao, T.-H. (2024). Risk Factors for Cervical Disc Arthroplasty Subsidence with Bryan Disc—A Retrospective Observational Analysis. Journal of Clinical Medicine, 13(6), 1589. https://doi.org/10.3390/jcm13061589






