Abstract
Background: There is a lack of studies investigating the prevalence of syncope-related injuries in a large representative cohort. The aim of this cross-sectional study is to investigate the prevalence of, and variables associated with syncope-related injuries and fractures in a large outpatient population in Germany. Methods: The present study used data from the Disease Analyzer database (IQVIA) and included adults with first-time diagnoses of syncope in 1 of 1284 general practices in Germany between 2005 and 2022 (index date). The prevalence of injuries and separate fractures documented on the index date was examined, and the association of demographic and clinical variables with the risk of syncope-related injuries and fractures was studied using multivariable logistic regression. Results: A total of 143,226 patients (mean age: 57.1 years, 56.9% female) were included in this study. The proportion of injuries was 10.4% and increased from 6.4% in the age group 18–30 to 15.0% in the age group >80 years. Female sex was associated with a slightly higher risk of injury (OR: 1.09; 95% CI: 1.05–1.13) and fractures (OR: 1.17; 95% CI: 1.07–1.28). Osteoporosis was associated with a higher risk of injury (OR: 1.25; 95% CI: 1.16–1.34) and fracture (OR: 1.53; 95% CI: 1.33–1.76), while obesity was only associated with a slightly increased risk of injury. Conclusions: Syncope-related injuries are common among syncope patients. Factors associated with a higher risk of syncope-related injuries, such as female sex, older age, and osteoporosis, can be incorporated into an effective risk stratification and help to improve the outcome of syncope patients.
1. Introduction
Syncope is characterized as a brief and temporary loss of consciousness (TLOC) due to transient global cerebral hypoperfusion, with an immediate onset and spontaneous and complete recovery [1,2,3,4]. With a lifetime cumulative incidence of up to 35% [5], syncope is common in the general population and accounts for approximately 1% of all emergency department visits in the U.S. [6], with an average cost of USD 5400 per hospitalization [7].
Although syncope is often considered a benign clinical entity [1,8,9,10], it can be associated with significantly increased mortality [8,11] and significantly reduced quality of life (QoL) for those affected [12,13,14,15]. Further possible and potentially serious consequences of immediate syncopal loss of consciousness include resulting injuries and fractures [3,16], making the condition a significant public health issue. Investigating the prevalence of syncope-related traumatic injuries in a cohort of 346 consecutive patients with recurrent VVS spells, Ammirati et al. found that 27.2% of patients studied had incurred at least one traumatic injury related to syncope, while 8.9% of the cohort even required hospitalization and surgical treatment due to the severity of their syncope-related traumatic injuries [17]. A systematic review of 23 studies by Jorge et al. came to similar conclusions, with a weighted mean injury rate of 33.5% among all VVS patients included in the studies reviewed [3].
However, there is a lack of studies investigating the prevalence of syncope-related injuries in a large representative cohort. Among other things, this is due to the fact that the majority of the studies directly or indirectly addressing the association between syncope and subsequent injury are based in a clinical setting. Consequently, the patient cohorts used for these studies cannot be assumed to be representative of the overall group of syncope patients, as it can be supposed that only a fraction of syncope patients in the overall population make use of higher-threshold services offered by specialized centers and emergency departments [3].
Therefore, the primary aim of this cross-sectional study is to investigate the prevalence of syncope-related injuries and fractures. The secondary aim was to evaluate variables associated with syncope-related injuries and fractures in a large outpatient population in Germany.
2. Methods
2.1. Database
The present study used data from the Disease Analyzer database (IQVIA), which has already been described in the scientific literature [18]. Briefly, the database contains demographic, diagnosis, and prescription data collected in office-based practices in Germany. The selection of practices included in the Disease Analyzer database relies on multiple variables (i.e., physician age, specialty group, community size category, and German federal state). The database includes around 3000 general and specialized practices in Germany.
2.2. Study Population and Variables
This retrospective cross-sectional study included adults with first-time syncope diagnosis (ICD-10 code: R55) in 1 of 1284 general practices in Germany between 2005 and 2022 (index date) (Figure 1).
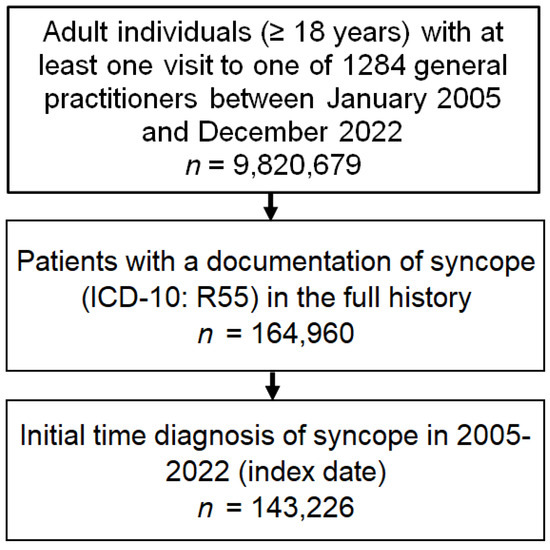
Figure 1.
Selection of study patients.
Demographic variables included age and sex. Several chronic conditions frequently associated with frailty and possible increased fall risk were documented within 12 months prior to the index date. These disorders included diabetes (ICD-10: E10–E14], essential hypertension (ICD-10: I10), lipid metabolism disorders (ICD-10: E78), obesity (ICD-10: E66), cardiac arrhythmias (ICD-10: I76–I79), depression (ICD-10: F32, F33), osteoporosis (ICD-10: M81), and dementia (ICD-10: F01, F03, G30).
2.3. Statistical Analyses
Baseline characteristics were described using absolute numbers (percentages) for all variables except for continuous age, which was described using the mean (standard deviation). In addition, the prevalence of injuries (ICD-10: S00–T14) and separate fractures (ICD-10: S02, S12, S22, S32, S42, S52, S62, S72, S82, S92, T02, T08, T10, T12) documented on the index date was studied in the overall sample and also within seven age groups (≤30, 31–40, 41–50, 51–60, 61–70, 71–80, >80 years), women and men, and patients with different comorbidities (diabetes, obesity, lipid metabolism disorders, hypertension, cardiac arrhythmias, depression, osteoporosis, dementia).
Finally, the association between these variables and the risk of syncope-related injuries and fractures was studied using multivariable logistic regression adjusted for age, sex, and the comorbidities diabetes, obesity, lipid metabolism disorders, hypertension, cardiac arrhythmias, depression, osteoporosis, and dementia. The results of the models are displayed as odds ratios (ORs) and 95% confidence intervals (95%CI. p-values lower than 0.05 were considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA).
3. Results
3.1. Baseline Characteristics of the Study Participants
A total of 143,226 patients were included in this study. The baseline characteristics of the study participants are displayed in Table 1. The mean (standard deviation) age was 57.1 (21.6) years, while the prevalence of women was 56.9%. The three most common co-diagnoses were hypertension (33.3%), lipid metabolism disorders (20.0%), and depression (15.2%).

Table 1.
Baseline characteristics of the study sample.
3.2. Prevalence of Syncope-Related Injuries and Fractures
Figure 2 and Figure 3 displays the prevalence of syncope-related injuries and fractures in the overall population and by age, sex, and co-diagnosis. In the overall population, the proportion of injuries was 10.4% and increased from 6.4% in the age group 18–30 to 15.0% in age group >80 years (Figure 2). This prevalence was highest in osteoporosis patients (15.6%). The prevalence of fractures was 1.6% in the overall population and increased from 0.3% in the age group 18–30 to 3.2% in the age group >80 years. Here too, fractures occurred in 3.5% of osteoporosis patients (Figure 3).

Figure 2.
Prevalence of syncope-related injuries and fractures in the overall population and by age and sex.
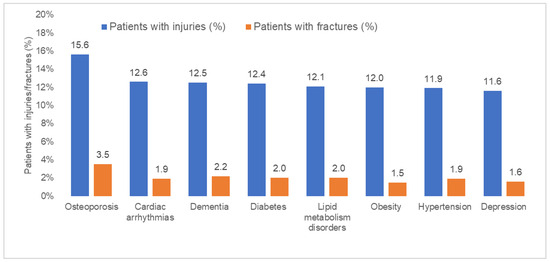
Figure 3.
Prevalence of syncope-related injuries and fractures by co-diagnoses.
3.3. Baseline Characteristics of Patients with and without Injuries and Fractures
Patients with injuries were older than patients without injuries (63.0 vs. 56.5 years, p < 0.001), and the proportion of women was slightly higher in the injury group (59.2% vs. 56.6%). Patients with fractures were much older than patients without fractures (70.9 vs. 56.9 years, p < 0.001), and the proportion of women was also higher in the former group (62.4% vs. 56.8%, p < 0.001). Due to the higher age, the proportions of comorbidities were also significantly higher among patients with injuries and fractures than among patients without fractures or injuries (Table 2).

Table 2.
Baseline characteristics of the study patients with and without injuries and fractures.
3.4. Variables Associated with Risk of Injury and Fracture
Table 3 shows the results of the univariable logistic regression since Table 4 shows the results of the multivariable logistic regression following stepwise selection. In the univariable regression analysis, all the included variables were significantly associated with an increased risk of injuries. However, in multivariable regression analysis, only higher age (OR: 1.02; 95% CI: 1.01–1.02 per year), female sex (OR: 1.09; 95% CI: 1.05–1.13), osteoporosis (OR: 1.25; 95% CI: 1.16–1.34), and obesity (OR: 1.12; 95%: 1.05–1.20) were associated with an increased risk of injury. Age (OR: 1.04; 95% CI: 1.04–1.04), female sex (OR: 1.17; 95% CI: 1.07–1.28), and osteoporosis (OR: 1.53, 95% CI: 1.33–1.76) were positively associated with a risk of fracture (Table 4).

Table 3.
Variables associated with risk of injury and fracture in syncope patients (univariable logistic regression).

Table 4.
Variables associated with risk of injury and fracture in syncope patients (multivariable logistic regression).
4. Discussion
This cross-sectional study showed that injuries in general were common among outpatients with at least one documented episode of syncope, whereas fractures were rather rare. Furthermore, there was a clear association between the presence of injuries and fractures and older age in the cohort studied. Osteoporosis and female sex were also found to be associated with a more frequent occurrence of injuries and fractures among patients with at least one documented episode of syncope.
Although syncope can be attributed to benign causes in a large number of cases [1,8,9,10], the immediate loss of consciousness is associated with a considerable risk of resulting injuries and fractures [3,17,19]. Both Jorge et al. in a systematic review and Ammirati et al. found markedly higher prevalences of syncope-related injuries among the syncope patients studied, at around one third and one quarter, respectively [3,17]. Investigating the risk of patients hospitalized for unexplained syncope and orthostatic hypotension, Johansson et al. found a fracture prevalence of 27% among the 30,399 individuals observed [20]. Like the results of Jorge et al. and Ammirati et al. discussed above, this represents a clear deviation from the findings of our study. The reason for these differences can be the fact that the studies of Jorge et al. and Ammirati et al. were conducted in hospital settings, where clinically more severe cases of syncope are treated [3], since our study was based on outpatients with probably less severe symptoms.
We found a significant association between the incidence of injuries and fractures among syncope patients and their age. One possible explanation for this association could be the increase in factors associated with older age, which in turn increase the risk of adverse outcomes in syncope, such as the occurrence of an injury or fracture as a result of syncope-related falls. Thus, older age is associated with an increased risk of frailty, as an overarching concept of an often progressive inability to adequately restore physical homeostasis following a stressor [21]. Various changes in the structural composition and metabolism of the bones often result in weaker and more brittle bones with age, which can also cause the general risk of fracture to increase with age [22].
Furthermore, our study showed that women had an increased risk of injury compared to men, particularly for the occurrence of fractures, which is consistent with the findings in the existing literature on this topic. Post-menopausal women in particular have a significantly increased risk of developing osteoporosis, as hormonal development during menopause, especially a lack of estrogen, has an unfavorable effect on bone stability and quality and results in an imbalance between bone formation and bone resorption in favor of resorption [23]. For example, women aged >65 and >80 had a higher risk of suffering a fracture during their lifetime than male patients in the same age groups [24].
A further finding of our study is the positive association between obesity and injuries, but there is no association between obesity and fractures. Individuals with obesity experience restricted mobility, raising the likelihood of falls. For example, Finkelstein et al. reported a strong association between body mass index and the probability of sustaining an injury [25]. Vice versa, not obesity but underweight is a known risk factor for fractures, since obesity is usually not associated with an increased risk of fractures [26,27].
The positive association between osteoporosis and fractures found in our study is well known. Osteoporosis leads to a decrease in bone mineral density, making bones porous and more susceptible to fractures. The loss of minerals, such as calcium, compromises the structural integrity of bones. The weakened bones are more prone to breaking, even with minimal force or trauma [28].
Although this study is based on a large patient population, the most important limitation is the bias created by the study design. By including only outpatients with a first visit after the first diagnosis of syncope, we may have missed many adverse events. For example, a patient only diagnosed with a fracture after seeing their GP would not have been counted. However, the database used does not include hospital data. Secondly, the use of ICD-10 codes might result in the misclassification and undercoding of specific diagnoses. Moreover, ICD-10 codes do not allow any statements to be made about the severity of the injuries and fractures recorded. Thirdly, the present study design does not allow us to differentiate between patients with single syncope episodes and those with recurrent syncope attacks. This would also have been interesting in view of the existing literature, which discusses an increased risk of syncope-related injury and risk of more severe injuries with an increasing number of syncope episodes [17,21]. Fourthly, the database does not include data on mortality. Finally, based on the data available, it is not possible to draw any conclusions regarding causality, and we were therefore only able to make assumptions regarding associations between different factors in this study.
5. Conclusions
Syncope-related injuries are common among syncope patients. Factors associated with a higher risk of syncope-related injuries, such as female sex, older age, and osteoporosis, can be incorporated into an effective risk stratification and help to improve the outcomes of syncope patients.
Author Contributions
D.C.G. contributed to the design of the study, managed the literature searches, and wrote the first draft of the manuscript. K.K. contributed to the design of the study, performed the statistical analyses, and corrected the manuscript. M.K. contributed to the design of the study and corrected the manuscript. S.K. and A.K. corrected the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The database used includes only anonymized data in compliance with the regulations of the applicable data protection laws. German law allows the use of anonymous electronic medical records for research purposes under certain conditions. Because patients were only queried as aggregates and no protected health information was available for queries, no Institutional Review Board approval was required for the use of this database or the completion of this study.
Informed Consent Statement
According to this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Brignole, M.; Moya, A.; de Lange, F.J.; Deharo, J.C.; Elliott, P.M.; Fanciulli, A.; Fedorowski, A.; Furlan, R.; Kenny, R.A. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018, 39, 1883–1948. [Google Scholar] [CrossRef] [PubMed]
- Quinn, J.V.; Stiell, I.G.; McDermott, D.A.; Sellers, K.L.; Kohn, M.A.; Wells, G.A. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann. Emerg. Med. 2004, 43, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Jorge, J.G.; Raj, S.R.; Teixeira, P.S.; Teixeira, J.A.C.; Sheldon, R.S. Likelihood of injury due to vasovagal syncope: A systematic review and meta-analysis. EP Eur. 2021, 23, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.C. Quality-of-Life, Health Service Use, and Costs Associated With Syncope. Prog. Cardiovasc. Dis. 2013, 55, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Ganzeboom, K.S.; Mairuhu, G.; Reitsma, J.B.; Linzer, M.; Wieling, W.; Van Dijk, N. Lifetime Cumulative Incidence of Syncope in the General Population: A Study of 549 Dutch Subjects Aged 35-60 Years. J. Cardiovasc. Electrophysiol. 2006, 17, 1172–1176. [Google Scholar] [CrossRef] [PubMed]
- Probst, M.A.; Kanzaria, H.K.; Gbedemah, M.; Richardson, L.D.; Sun, B.C. National trends in resource utilization associated with ED visits for syncope. Am. J. Emerg. Med. 2015, 33, 998–1001. [Google Scholar] [CrossRef]
- Sun, B.C.; Emond, J.A.; Camargo, C.A. Direct medical costs of syncope-related hospitalizations in the United States. Am. J. Cardiol. 2005, 95, 668–671. [Google Scholar] [CrossRef]
- D’Ascenzo, F.; Biondi-Zoccai, G.; Reed, M.J.; Gabayan, G.Z.; Suzuki, M.; Costantino, G.; Furlan, R.; Del Rosso, A.; Sarasin, F.P.; Sun, B.C.; et al. Incidence, etiology and predictors of adverse outcomes in 43,315 patients presenting to the Emergency Department with syncope: An international meta-analysis. Int. J. Cardiol. 2013, 167, 57–62. [Google Scholar] [CrossRef]
- Ungar, A.; Del Rosso, A.; Giada, F.; Bartoletti, A.; Furlan, R.; Quartieri, F.; Lagi, A.; Morrione, A.; Mussi, C.; Lunati, M.; et al. Early and late outcome of treated patients referred for syncope to emergency department: The EGSYS 2 follow-up study. Eur. Heart J. 2010, 31, 2021–2026. [Google Scholar] [CrossRef]
- Cheshire, W.P. Syncope. Continuum (Minneap Minn). Sel. Top. Outpatient Neurol. 2017, 23, 335–358. [Google Scholar] [CrossRef]
- Task Force Members; Moya, A.; Sutton, R.; Ammirati, F.; Blanc, J.J.; Brignole, M.; Dahm, J.B.; Deharo, J.C.; Gajek, J.; Gjesdal, K.; et al. Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). Eur. Heart J. 2009, 30, 2631–2671. [Google Scholar] [CrossRef] [PubMed]
- Atici, A.; Asoglu, R.; Demirkiran, A.; Serbest, N.G.; Emektas, B.; Sarikaya, R.; Yeldan, I.; Bilge, A.K. The relationship between clinical characteristics and psychological status and quality of life in patients with vasovagal syncope. North. Clin. Istanb. 2020, 7, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Giada, F.; Silvestri, I.; Rossillo, A.; Nicotera, P.; Manzillo, G.; Raviele, A. Psychiatric profile, quality of life and risk of syncopal recurrence in patients with tilt-induced vasovagal syncope. Europace 2005, 7, 465–471. [Google Scholar] [CrossRef]
- Ng, J.; Sheldon, R.S.; Ritchie, D.; Raj, V.; Raj, S.R. Reduced Quality of Life and Greater Psychological Distress in Vasovagal Syncope Patients Compared to Healthy Individuals. Pacing Clin. Electrophysiol. 2019, 42, 180–188. [Google Scholar] [CrossRef]
- Sutton, R.; Ricci, F.; Fedorowski, A. Risk stratification of syncope: Current syncope guidelines and beyond. Auton. Neurosci. Basic Clin. 2022, 238, 102929. [Google Scholar] [CrossRef]
- Kavi, K.S.; Gall, N.P. Trauma and syncope: Looking beyond the injury. Trauma Surg. Acute Care Open 2023, 8, e001036. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, F.; Colivicchi, F.; Velardi, A.; Santini, M. Prevalence and correlates of syncope-related traumatic injuries in tilt-induced vasovagal syncope. Ital. Heart J. 2001, 2, 38–41. [Google Scholar]
- Rathmann, W.; Bongaerts, B.; Carius, H.J.; E Kruppert, S.; Kostev, K. Basic characteristics and representativeness of the German Disease Analyzer database. Int. J. Clin. Pharmacol. Ther. 2018, 56, 459–466. [Google Scholar] [CrossRef]
- Bartoletti, A.; Fabiani, P.; Bagnoli, L.; Cappelletti, C.; Cappellini, M.; Nappini, G.; Gianni, R.; Lavacchi, A.; Santoro, G.M. Physical injuries caused by a transient loss of consciousness: Main clinical characteristics of patients and diagnostic contribution of carotid sinus massage. Eur. Heart J. 2008, 29, 618–624. [Google Scholar] [CrossRef]
- Johansson, M.; Rogmark, C.; Sutton, R.; Fedorowski, A.; Hamrefors, V. Risk of incident fractures in individuals hospitalised due to unexplained syncope and orthostatic hypotension. BMC Med. 2021, 19, 188. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Boskey, A.L.; Coleman, R. Aging and Bone. J. Dent. Res. 2010, 89, 1333–1348. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.C.; Tella, S.H. Prevention and treatment of postmenopausal osteoporosis. J. Steroid Biochem. Mol. Biol. 2014, 142, 155–170. [Google Scholar] [CrossRef]
- Court-Brown, C.M.; Clement, N.D.; Duckworth, A.D.; Aitken, S.; Biant, L.C.; McQueen, M.M. The spectrum of fractures in the elderly. Bone Jt. J. 2014, 96-B, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Chen, H.; Prabhu, M.; Trogdon, J.G.; Corso, P.S. The relationship between obesity and injuries among U.S. adults. Am. J. Health Promot. 2007, 21, 460–468. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.; Han, S.; Jang, H.D.; Hong, J.Y.; Han, K.; Kim, H.J.; Yeom, J.S. Underweight and risk of fractures in adults over 40 years using the nationwide claims database. Sci. Rep. 2023, 13, 8013. [Google Scholar] [CrossRef]
- Kim, J.G.; Hong, J.Y.; Park, J.; Park, S.M.; Han, K.; Kim, H.J.; Yeom, J.S. Risk of fracture according to temporal changes of low body weight changes in adults over 40 years: A nationwide population-based cohort study. BMC Public Health 2023, 23, 948. [Google Scholar] [CrossRef]
- LeBoff, M.S.; Greenspan, S.L.; Insogna, K.L.; Lewiecki, E.M.; Saag, K.G.; Singer, A.J.; Siris, E.S. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2022, 33, 2049–2102. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).