Pharmacological Interventions in Paraphilic Disorders: Systematic Review and Insights
Abstract
1. Introduction
2. Materials and Methods
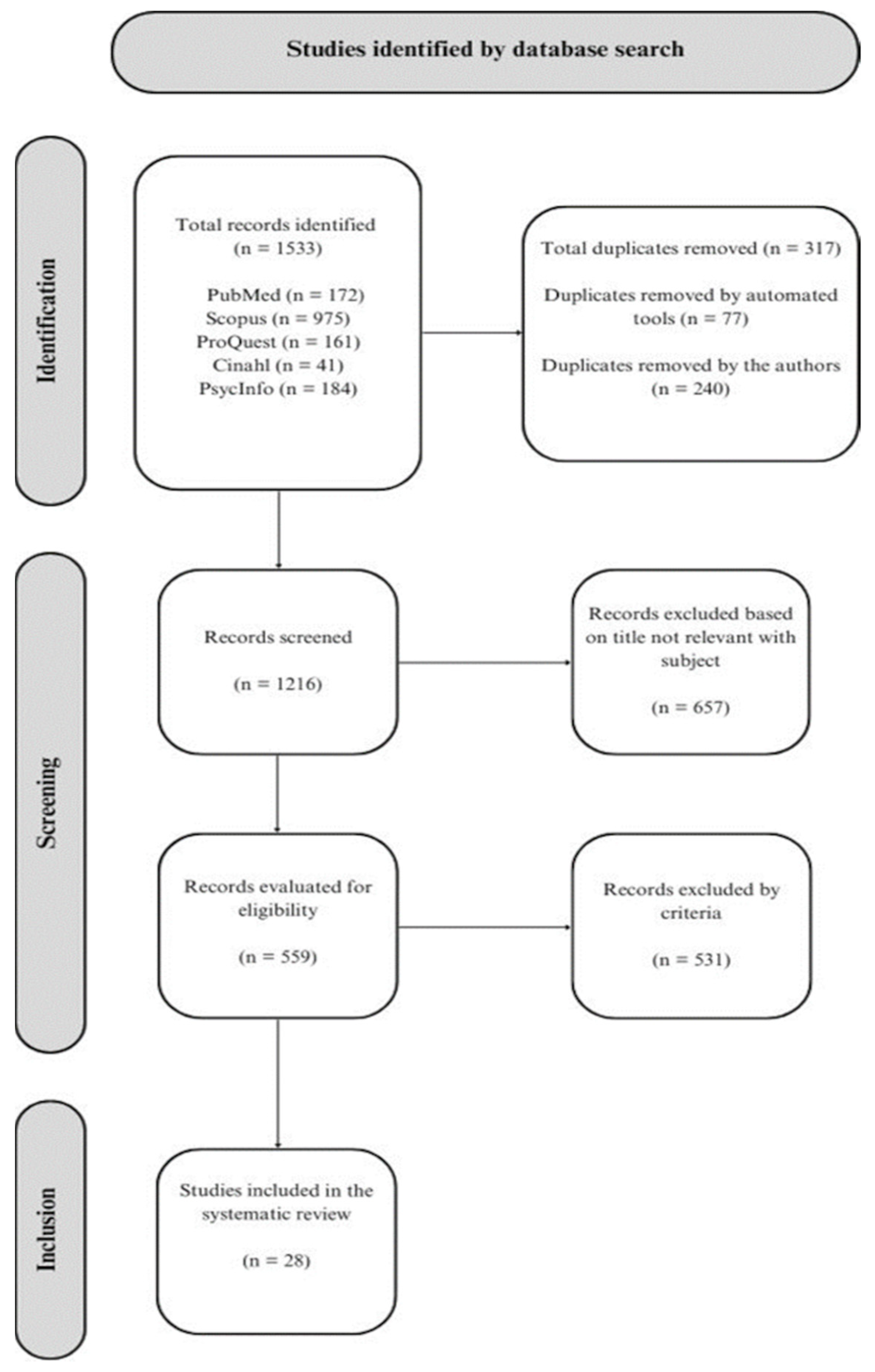
2.1. Literature Search and Inclusion Criteria
2.2. Quality Assessment
3. Results
3.1. Included Studies
3.2. Quality Assessment
3.3. Evaluation of Effectiveness
3.3.1. Selective Serotonin Reuptake Inhibitors (SSRIs)
3.3.2. Steroidal Antiandrogens
3.3.3. GnRH Agonist and Analogue
3.3.4. Other Drugs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beech, A.R.; Miner, M.H.; Thornton, D. Paraphilias in the DSM-5. Annu. Rev. Clin. Psychol. 2016, 12, 383–406. [Google Scholar] [CrossRef] [PubMed]
- Krueger, R.B.; Kaplan, M.S. The paraphilic and hypersexual disorders: An overview. J. Psychiatr. Pract. 2001, 7, 391–403. [Google Scholar] [CrossRef]
- Turner, D.; Petermann, J.; Harrison, K.; Krueger, R.; Briken, P. Pharmacological treatment of patients with paraphilic disorders and risk of sexual offending: An international perspective. World J. Biol. Psychiatry 2017, 20, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Walton, M.T.; Cantor, J.M.; Bhullar, N.; Lykins, A.D. Hypersexuality: A critical review and introduction to the “sexhavior cycle”. Arch. Sex. Behav. 2017, 46, 2231–2251. [Google Scholar] [CrossRef] [PubMed]
- Tozdan, S.; Briken, P. Paraphilias: Diagnostics, Comorbidities, and Treatment. In Psychiatry and Sexual Medicine: A Comprehensive Guide for Clinical Practitioners; Lew-Starowicz, M., Giraldi, A., Krüger, T.H.C., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 407–416. [Google Scholar] [CrossRef]
- Kafka, M. Axis I Psychiatric Disorders, Paraphilic Sexual Offending and Implications for Pharmacological Treatment. Isr. J. Psychiatry Relat. Sci. 2012, 49, 255–261. [Google Scholar] [PubMed]
- Caldeano, A.R.; Nunes, J.; da Costa, P. Paraphilic disorder in the 21st century. Eur. Psychiatry 2016, 33, S591. [Google Scholar] [CrossRef]
- Yakeley, J. Psychoanalytic perspectives on paraphilias and perversions. Eur. J. Psychother. Couns. 2018, 20, 164–183. [Google Scholar] [CrossRef]
- First, M.B. DSM-5 and paraphilic disorders. J. Am. Acad. Psychiatry Law. Online 2014, 42, 191–201. [Google Scholar]
- Di Lorenzo, G.; Gorea, F.; Longo, L.; Ribolsi, M. Paraphilia and paraphilic disorders. In Sexual Dysfunctions in Mentally Ill Patients; Springer: Cham, Switzerland, 2018; pp. 193–213. [Google Scholar]
- Baez-Sierra, D.; Balgobin, C.; Wise, T.N. Treatment of Paraphilic Disorders. In Practical Guide to Paraphilia and Paraphilic Disorders; Springer: Cham, Switzerland, 2016; pp. 43–62. [Google Scholar]
- Holoyda, B.J.; Kellaher, D.C. The biological treatment of paraphilic disorders: An updated review. Curr. Psychiatry Rep. 2016, 18, 19. [Google Scholar] [CrossRef] [PubMed]
- Krueger, R.B.; Kaplan, M.S. Behavioral and psychopharmacological treatment of the paraphilic and hypersexual disorders. J. Psychiatr. Pract. 2002, 8, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, D.M.; Bradford, J.M.W. Treatment of the paraphilic disorders: A review of the role of the selective serotonin reuptake inhibitors. Sex. Abus. 1997, 9, 349–360. [Google Scholar] [CrossRef]
- Turner, D.; Briken, P. Treatment of Paraphilic Disorders in Sexual Offenders or Men with a Risk of Sexual Offending with Luteinizing Hormone-Releasing Hormone Agonists: An Updated Systematic Review. J. Sex. Med. 2018, 15, 77–93. [Google Scholar] [CrossRef]
- Winder, B.; Fedoroff, J.P.; Grubin, D.; Klapilova, K.; Kamenskov, M.; Tucker, D.; Basinskaya, I.A.; Vvedensky, G.E. The pharmacologic treatment of problematic sexual interests, paraphilic disorders and sexual preoccupation in adult men who have committed a sexual offence. Int. Rev. Psychiatry 2019, 31, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Landgren, V.; Savard, J.; Dhejne, C.; Jokinen, J.; Arver, S.; Seto, M.C.; Rahm, C. Pharmacological Treatment for Pedophilic Disorder and Compulsive Sexual Behavior Disorder: A Review. Drugs 2022, 82, 663–681. [Google Scholar] [CrossRef] [PubMed]
- Gola, M.; Lewczuk, K.; Potenza, M.N.; Kingston, D.A.; Grubbs, J.B.; Stark, R.; Reid, R.C. What should be included in the criteria for compulsive sexual behavior disorder? J. Behav. Addict. 2022, 11, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2015. [Google Scholar]
- Abouesh, A.; Clayton, A. Compulsive Voyeurism and Exhibitionism: A Clinical Response to Paroxetine. Arch. Sex. Behav. 1999, 28, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.W.C.; Choy, A.L. Clinical Case Report Series 1 Clinical Characteristics and Treatment Response to SSRI in a Female Pedophile. Arch. Sex. Behav. 2002, 31, 211–215. [Google Scholar] [CrossRef]
- Baltieri, D.A.; De Andrade, A. Treatment of paraphilic sexual offenders in brazil: Issues and controversies. Int. J. Forensic Ment. Health 2009, 8, 218–223. [Google Scholar] [CrossRef]
- Emmanuel, N.P.; Lydiard, R.B.; Ballenger, J.C. Fluoxetine treatment of voyeurism. Am. J. Psychiatry 1991, 148, 950. [Google Scholar]
- Perilstein, R.D.; Lipper, S.; Friedman, L.J. Three cases of paraphilias responsive to fluoxetine treatment. J. Clin. Psychiatry 1991, 52, 169–170. [Google Scholar]
- Saleh, F.M.; Berlin, F.S. Sex hormones, neurotransmitters, and psychopharmacological treatments in men with paraphilic disorders. J. Child Sex. Abus. 2004, 12, 233–253. [Google Scholar] [CrossRef] [PubMed]
- Shiwach, R.S.; Prosser, J. Treatment of an unusual case of masochism. J. Sex Marital Ther. 1998, 24, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Amelung, T.; Kuhle, L.F.; Konrad, A.; Pauls, A.; Beier, K.M. Androgen deprivation therapy of self-identifying, help-seeking pedophiles in the Dunkelfeld. Int. J. Law Psychiatry 2012, 35, 176–184. [Google Scholar] [CrossRef]
- Bradford, J.M.; Pawlak, A. Double-Blind Placebo Crossover Study of Cyproterone Acetate in the Treatment of the Paraphilias. Arch. Sex. Behav. 1993, 22, 383–402. [Google Scholar] [CrossRef]
- Boons, L.; Jeandarme, I.; Vervaeke, G. Androgen Deprivation Therapy in Pedophilic Disorder: Exploring the Physical, Psychological, and Sexual Effects From a Patient’s Perspective. J. Sex. Med. 2021, 18, 353–362. [Google Scholar] [CrossRef]
- Cooper, A.J.; Cernovsky, Z.Z. Comparison of Cyproterone Acetate (CPA) and Leuprolide Acetate (LHRH Agonist) in a Chronic Pedophile: A Clinical Case Study. Biol. Psychiatry 1994, 36, 269–271. [Google Scholar] [CrossRef]
- Kiersch, T.A. Treatment of Sex Offenders with Depo-Provera. Bull. Am. Acad. Psychiatry Law 1990, 18, 179–187. [Google Scholar] [PubMed]
- Kravitz, H.M.; Haywood, T.W.; Kelly, J.; Wahlstrom, C.; Liles, S.; Cavanaugh, J.L. Medroxyprogesterone Treatment for Paraphiliacs. Bull. Am. Acad. Psychiatry Law 1995, 23, 19–33. [Google Scholar]
- Krueger, R.B.; Hembree, W.; Hill, M. Prescription of medroxyprogesterone acetate to a patient with pedophilia, resulting in Cushing’s Syndrome and adrenal insufficiency. Sex. Abus. J. Res. Treat. 2006, 18, 227–228. [Google Scholar] [CrossRef]
- Lehne, G.K.; Money, J. The First Case of Paraphilia Treated With Depo-Provera: 40-Year Outcome. J. Sex Educ. Ther. 2000, 25, 213–220. [Google Scholar] [CrossRef]
- Meyer Ill, W.J.; Cole, C.; Emory, E. Depo Provera Treatment for Sex Offending Behavior: An Evaluation of Outcome. Bull. Am. Acad. Psychiatry Law 1992, 20, 249–259. [Google Scholar]
- Choi, J.H.; Lee, J.W.; Lee, J.K.; Jang, S.; Yoo, M.; Lee, D.B.; Hong, J.-W.; Noh, I.S.; Lim, M.H. Therapeutic effects of leuprorelin (leuprolide acetate) in sexual offenders with paraphilia. J. Korean Med. Sci. 2018, 33, e231. [Google Scholar] [CrossRef]
- Saleh, F. A hypersexual paraphilic patient treated with leuprolide acetate: A single case report. J. Sex Marital Ther. 2005, 31, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Dickey, R. The Management of a Case of Treatment-Resistant Paraphilia with a Long-Acting LHRH Agonist. Can. J. Psychiatry 1992, 37, 567–570. [Google Scholar] [CrossRef]
- Habermeyer, B.; Händel, N.; Lemoine, P.; Klarhöfer, M.; Seifritz, E.; Dittmann, V.; Graf, M. LH-RH agonists modulate amygdala response to visual sexual stimulation: A single case fMRI study in pedophilia. Neurocase 2012, 18, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Schiffer, B.; Gizewski, E.; Kruger, T. Reduced neuronal responsiveness to visual sexual stimuli in a pedophile treated with a long-acting LH-RH agonist. J. Sex. Med. 2009, 6, 892–894. [Google Scholar] [CrossRef] [PubMed]
- Dickey, R. Case report: The management of bone demineralization associated with long-term treatment of multiple paraphilias with long-acting LHRH agonists. J. Sex Marital Ther. 2002, 28, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Landgren, V.; Malki, K.; Bottai, M.; Arver, S.; Rahm, C. Effect of gonadotropin-releasing hormone antagonist on risk of committing child sexual abuse in men with pedophilic disorder: A randomized clinical trial. JAMA Psychiatry 2020, 77, 897–905. [Google Scholar] [CrossRef]
- Landgren, V.; Olsson, P.; Briken, P.; Rahm, C. Effects of testosterone suppression on desire, hypersexuality, and sexual interest in children in men with pedophilic disorder. World J. Biol. Psychiatry 2022, 23, 560–571. [Google Scholar] [CrossRef]
- Rösler, A.; Witztum, E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N. Engl. J. Med. 1998, 338, 416–422. [Google Scholar] [CrossRef]
- Rousseau, L.; Couture, M.; Dupont, A.; Labrie, F.; Couture, N. Effect of combined androgen blockade with an LHRH agonist and flutamide in one severe case of male exhibitionism. Can. J. Psychiatry 1990, 35, 338–341. [Google Scholar] [CrossRef]
- Shiah, I.-S.; Chao, C.-Y.; Mao, W.-C.; Chuang, Y.-J. Treatment of paraphilic sexual disorder: The use of topiramate in fetishism. Int. Clin. Psychopharmacol. 2006, 21, 241–243. [Google Scholar] [CrossRef]
- Vayısoğlu, S. Symptoms of exhibitionism that regress with bupropion: A case report. Front. Psychiatry 2023, 13, 1079863. [Google Scholar] [CrossRef]
- Pearson, H.J.; Marshall, W.L.; Barbaree, H.E.; Southmayd, S. Treatment of a Compulsive Paraphiliac with Buspirone. Ann. Sex Res. 1992, 5, 239–246. [Google Scholar] [CrossRef]
- Overall, J.E.; Gorham, D.R. The Brief Psychiatric Rating Scale; Southern University Press: Skudai, Malaysia, 1962; Volume 10. [Google Scholar]
- Thibaut, F.; Cosyns, P.; Fedoroff, J.P.; Briken, P.; Goethals, K.; Bradford, J.M.W. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J. Biol. Psychiatry 2020, 21, 412–490. [Google Scholar] [CrossRef]
- Bickle, A.; Cameron, C.; Hassan, T.; Safdar, H.; Khalifa, N. International overview of phallometric testing for sexual offending behaviour and sexual risk. BJPsych Int. 2021, 18, E11. [Google Scholar] [CrossRef] [PubMed]
- Marshall, W.L. Phallometric assessments of sexual interests: An update. Curr. Psychiatry Rep. 2014, 16, 428. [Google Scholar] [CrossRef] [PubMed]
- Kolářský, A.; Freund, K.; Machek, J.; Polak, O. Male sexual deviation: Association with early temporal lobe damage. Arch. Gen. Psychiatry 1967, 17, 735–743. [Google Scholar] [CrossRef]
| Study | Samples and Diagnoses | Treatment | Duration of Treatment | Main Results | Side Effects |
|---|---|---|---|---|---|
| Selective serotonin reuptake inhibitors (SSRIs) | |||||
| Abouesh and Clayton (1999) [20] | two men with voyeuristic (A) and exhibitionistic (B) disorder | Paroxetine: A: 20 mg/day; B: 30 mg/day. | A: three months of treatment and then four months without B: six months of treatment and two months follow-up | Improved impulse control, decrease in fantasies and behaviors. | NR |
| Chow and Choy (2002) [21] | one woman sex offender with pedophilia | Sertraline (50 mg/day) + psychotherapy | 12 months | Decrease in intensity and frequency of fantasies, increased impulse control. | NR |
| Baltieri and De Andrade (2009) [22] | one man with exhibitionism and pedophilia | (1) Sertraline (200 mg/day) + topiramate (200 mg/day) + haloperidol (300 mg/mo) + psychotherapy; (2) addition of MPA (300 mg/2 tmo). | four months of treatment and three months follow-up | (1) No decrease in fantasies; (2) absence of fantasies and deviant behaviors. | NR |
| Emmanuel et al. (1991) [23] | one man with voyeurism | Fluoxetine (60 mg/day) | 3 months | Suppression of thoughts and deviant behaviors. | NR |
| Perilstein et al. (1991) [24] | three men | Fluoxetine | - | Improvement of impulse control | NR |
| Saleh and Berlin, (2004) [25] | one man with exhibitionism | Fluoxetine | 6 months | Urge reduction and sexual desire. | Delayed ejaculation |
| Shiwach and Prosser (1998) [26] | one man with masochism | Fluoxetine (80 mg/day) + psychotherapy | 42 weeks | Decreased fantasies and arousal. | NR |
| Steroidal antiandrogens | |||||
| Amelung et al. (2012) [27] | one hundred and eleven patients with pedophilia | (1) seven with CPA (300–600 mg/biweek) and seven with GnRHa + Psychotherapy; (2) ninety-six with psychotherapy. SSRI as an add-on if necessary. | 3 months | (1) Decreased deviant behavior and increased self-efficacy. | NR |
| Bradford et al. (1993) [28] | nineteen patients with multiple paraphilias (1) + placebo (2) | (1) CPA (50–200 mg/day); (2) placebo (50–200 mg/day). | 8 months | Decreased TS, FSH, LH, decreased BPRS scores. | Without any significant variations |
| Boons et al. (2020) [29] | twelve sex offenders with pedophilia | (1) CPA + CBT; (2) triptorelin + CBT. | - | Decrease in fantasies, urges, and behaviors. | (1) Gastric problems, reduced blood pressure; (2) weight gain, loss of bone mass. |
| Cooper and Cernovsky (1994) [30] | one man with pedophilia | (1) CPA (100–200 mg/day); (2) leuprolide acetate (7.5 mg/mo). | 38 months | (1) Decrease in values; (2) suppressed TS levels, arousal, and self-report measures. | NR |
| Kiersch (1990) [31] | eight men with pedophilia | MPA (DepoProvera) (100–400 mg/week) + Saline (100–400 mg/week) | 64 weeks | Remission fantasies, arousal with nondeviant stimuli. Decreased fantasies and frequency of masturbation with MPA. Decreased fantasies with saline. Decrease with saline, increase with MPA. | Glaucoma Migraine |
| Kravitz et al. (1995) [32] | twenty-nine men with various paraphilias | MPA (300 mg/week) + Group therapy MPA | 6 months | Suppression of fantasies and deviant activities, increased ability to control impulses. | Muscle cramps, weight gain, migraine, fatigue, lethargy, drowsiness, depression, anxiety, pulmonary embolism. |
| Krueger et al. (2006) [33] | one man with pedophilia | MPA (300 mg/day) | 4 years | Reduced sexual impulses. | Gynecomastia, obesity, adrenal insufficiency, Cushing’s syndrome. |
| Lehne and Money (2000) [34] | one man with multiple paraphilias | MPA | forty years’ follow-up | Decrease in TS levels, cessation of deviant urges. | Erectile dysfunction, weight gain, fatigue. |
| Meyer et al. (1992) [35] | forty sex offenders with various paraphilias | MPA (400 mg/week) + psychotherapy + Group therapy | from 6 months to 12 years | Eighteen percent reiteration of abuse with MPA, 35% reiteration after termination, 58% reiteration without MPA. | Weight gain, migraine headaches, cramps, increased blood pressure, diabetes mellitus. |
| GnRH agonists or analogs | |||||
| Choi et al. (2018) [36] | seven sex offenders with various paraphilias | Leuprolide acetate + psychotherapy | 12 months | Decreased sexual fantasies, sexual interest, decreased scores on the questionnaires. | Feminization, fatigue, hot flushes. |
| Saleh (2005) [37] | one patient with hypersexuality and exhibitionism | Leuprolide acetate (7.5 mg/mo) + psychotherapy | 5 months | Decreased urge and sexual drive, decreased LH, FSH, TS levels. | NR |
| Dickey (1992) [38] | one man with multiple paraphilias | Leuprolide acetate | 32 months | Decreased TS levels, LH, decreased frequency of masturbation and cessation of deviant behavior. | NR |
| Habermeyer et al. (2011) [39] | one man with homosexual pedophilia | Leuprorelin (11.25 mg/3 mo) | - | Decreased TS levels, decreased activation of the amygdala. | NR |
| Schiffer et al. (2009) [40] | one man with pedophilia | Leuprorelin (11.25 mg/3 mo) | 9 months | Decrease in processing of visual stimuli in subcortical areas. | NR |
| Dickey (2002) [41] | one man with multiple paraphilias | Leuprolide acetate | 10 years | Decreased TS levels, increased ability to control. | Osteoporosis |
| Landgren et al. (2020) [42] | fifty-two men with pedophilia | (1) degarelix (120 mg); (2) placebo. | 2 weeks | Decreased scores on scale of risk. | (1) Hepatobiliary enzyme increase, suicidal ideation; (2) NR. |
| Landgren et al. (2022) [43] | 52 men with pedophilia | (1) degarelix (120 mg) [25]; (2) placebo [25]. | 10 weeks | Reduced SDI, HBI, decreased deviant interest. | NR |
| Rösler and Witton (1998) [44] | thirty patients with severe paraphilias | Triptorelin (3.75 mg/mo) + psychotherapy | 8–42 months | Decreased questionnaire scores, decreased hormone levels, decreased fantasies. | Osteoporosis, hot flushes, muscle tension, erectile dysfunction. |
| Rousseau et al. (1990) [45] | one patient with exhibitionism | Flutamide + LHRH agonist | 52 weeks | TS decrease, DHT, remission of deviant activities, decrease in sexual fantasies. | Hot flushes |
| Other drugs | |||||
| Shiah et al. (2006) [46] | one man with fetishism | Topiramate (200 mg/day) | 6 months | Reduction in symptoms, development of ability to control. | NR |
| Vayisoglu (2023) [47] | one patient with exhibitionism | Bupropion (150 mg/day) | 6 months | Reduction of deviant fantasies and impulses. | NR |
| Pearson et al. (1992) [48] | one patient with exhibitionism and telephone scatology. | Buspirone (25 mg/day) + psychotherapy | 30 months | Termination of deviant behaviors, suppression of deviant fantasies. | NR |
| Paper | Selection | Comparability | Exposure | Tot | |||||
|---|---|---|---|---|---|---|---|---|---|
| Abouesh and Clayton (1999) [20] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Chow and Choy (2002) [21] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Baltieri and De Andrade (2009) [22] | 1a | 2b | - | - | - | 1a | - | - | 2 |
| Emmanuel et al. (1991) [23] | 1c | 2b | - | - | - | 1d | - | - | 0 |
| Perilstein et al. (1991) [24] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Shiwach and Prosser (1998) [26] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Dickey (1992) [38] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Amelung et al. (2012) [27] | 1a | 2a | 3b | 4b | 1a | 1d | 2a | 3b | 4 |
| Bradford et al. (1993) [28] | 1a | 2a | 3a | 4b | 1a | 1a | 2a | 3b | 6 |
| Boons et al. (2020) [29] | 1a | 2a | 3b | 4b | 1a | 1d | 2a | 3b | 4 |
| Cooper and Cernovsky (1994) [30] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Kiersch (1990) [31] | 1c | 2b | - | - | - | 1d | - | - | 0 |
| Kravitz et al. (1995) [32] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Krueger et al. (2006) [33] | 1c | 2b | - | - | - | 1d | - | - | 0 |
| Lehne and Money (2000) [34] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Meyer et al. (1992) [35] | 1a | 2a | 3a | 4b | 1a | 1d | 2b | 3b | 4 |
| Choi et al. (2018) [36] | 1a | 2a | 3a | 4b | 1a | 1a | 2a | 3b | 6 |
| Dickey (2002) [41] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Habermeyer (2012) [39] | 1a | 2b | - | - | - | 1a | - | - | 2 |
| Landgren et al. (2020) [42] | 1b | 2b | 3a | 4b | 1a | 1b | 2a | 3b | 4 |
| Landgren et al. (2022) [43] | 1a | 2a | 3a | 4b | 1a | 1d | 2a | 3b | 5 |
| Saleh (2005) [37] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Schiffer et al. (2009) [40] | 1c | 2b | - | - | - | 1d | - | - | 0 |
| Rousseau et al. (1990) [45] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Rösler and Witztum (1998) [44] | 1a | 2a | - | - | - | 1a | - | - | 3 |
| Shiah et al. (2006) [46] | 1a | 2b | - | - | - | 1d | - | - | 1 |
| Vayisoglu (2023) [47] | 1b | 2b | - | - | - | 1d | - | - | 0 |
| Pearson et al. (1992) [48] | 1a | 2b | - | - | - | 1d | - | - | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Culos, C.; Di Grazia, M.; Meneguzzo, P. Pharmacological Interventions in Paraphilic Disorders: Systematic Review and Insights. J. Clin. Med. 2024, 13, 1524. https://doi.org/10.3390/jcm13061524
Culos C, Di Grazia M, Meneguzzo P. Pharmacological Interventions in Paraphilic Disorders: Systematic Review and Insights. Journal of Clinical Medicine. 2024; 13(6):1524. https://doi.org/10.3390/jcm13061524
Chicago/Turabian StyleCulos, Chiara, Massimo Di Grazia, and Paolo Meneguzzo. 2024. "Pharmacological Interventions in Paraphilic Disorders: Systematic Review and Insights" Journal of Clinical Medicine 13, no. 6: 1524. https://doi.org/10.3390/jcm13061524
APA StyleCulos, C., Di Grazia, M., & Meneguzzo, P. (2024). Pharmacological Interventions in Paraphilic Disorders: Systematic Review and Insights. Journal of Clinical Medicine, 13(6), 1524. https://doi.org/10.3390/jcm13061524







