Femoral Neck Fractures Treated by Closed Reduction and Internal Fixation with the Double Fluoroscope Technique: A Preliminary Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
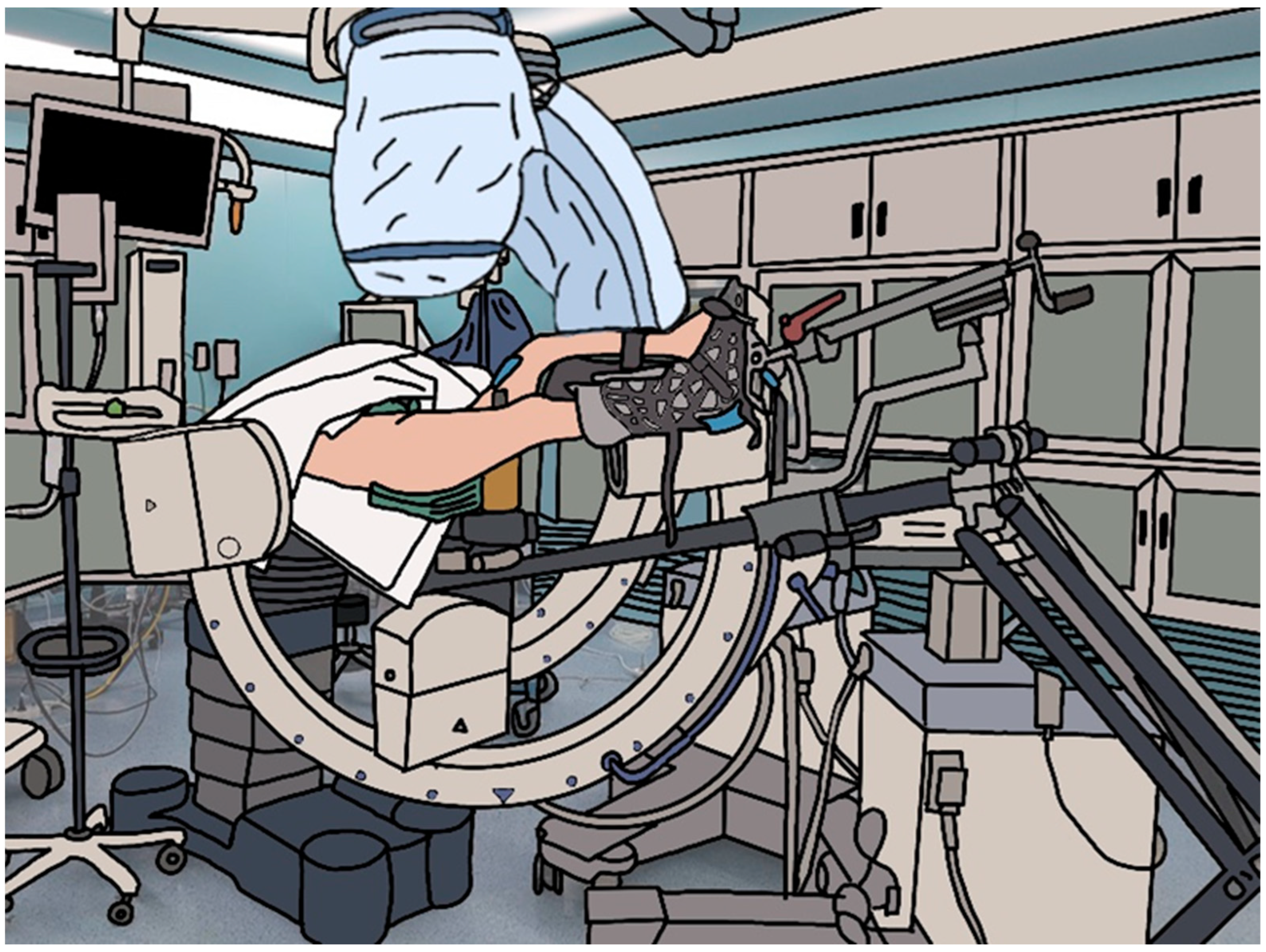
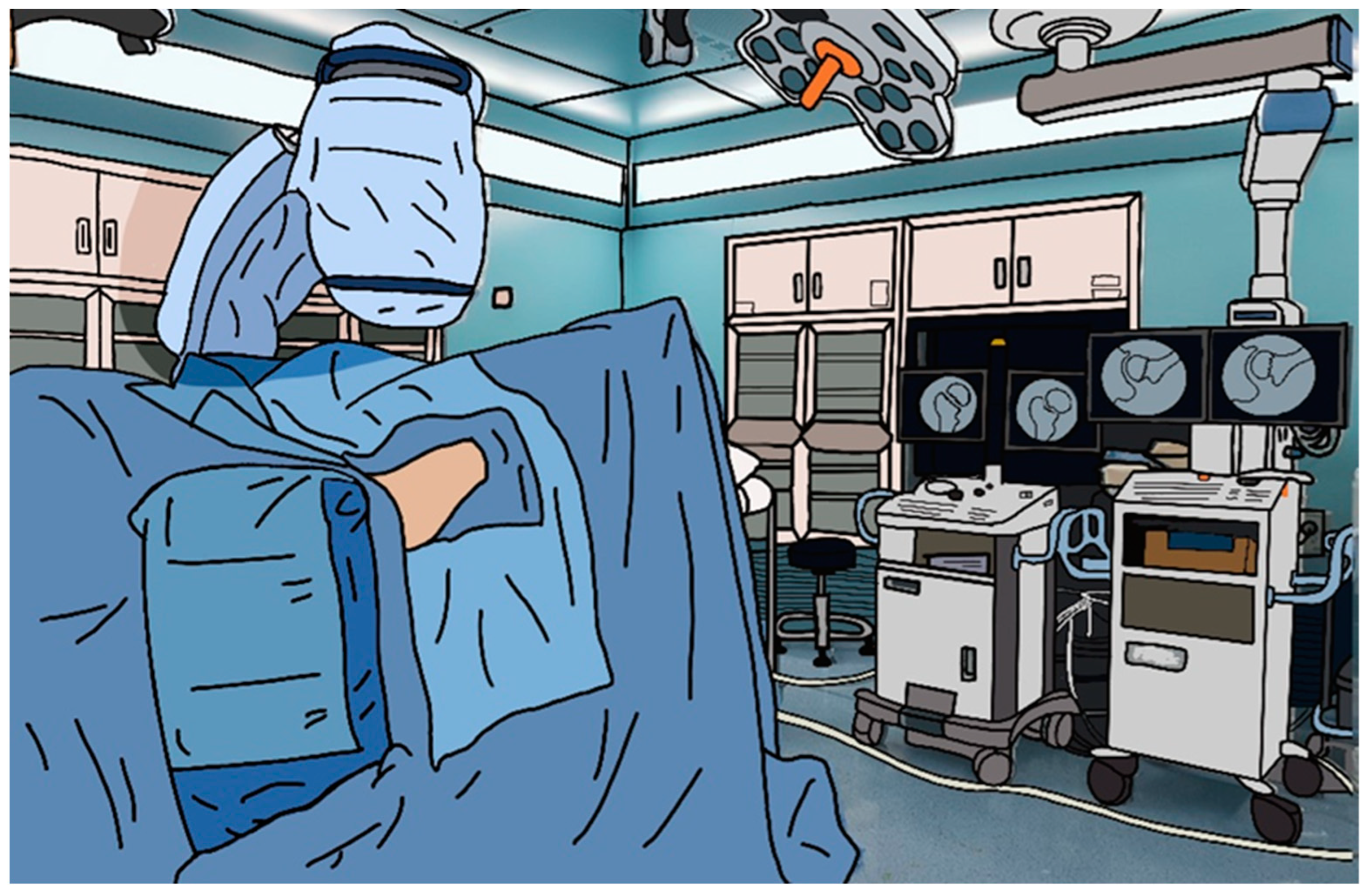
2.2. Operation Device
2.3. Study Design
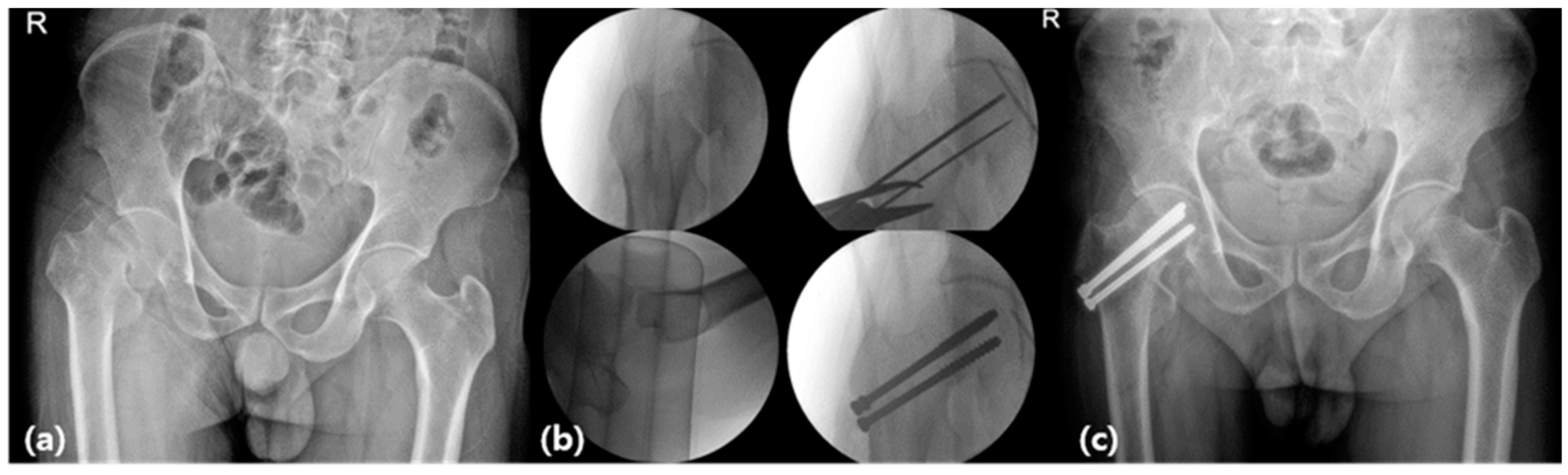
2.4. Procedure
2.5. Data Collection
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Participants (Single C-Arm versus Double C-Arm)
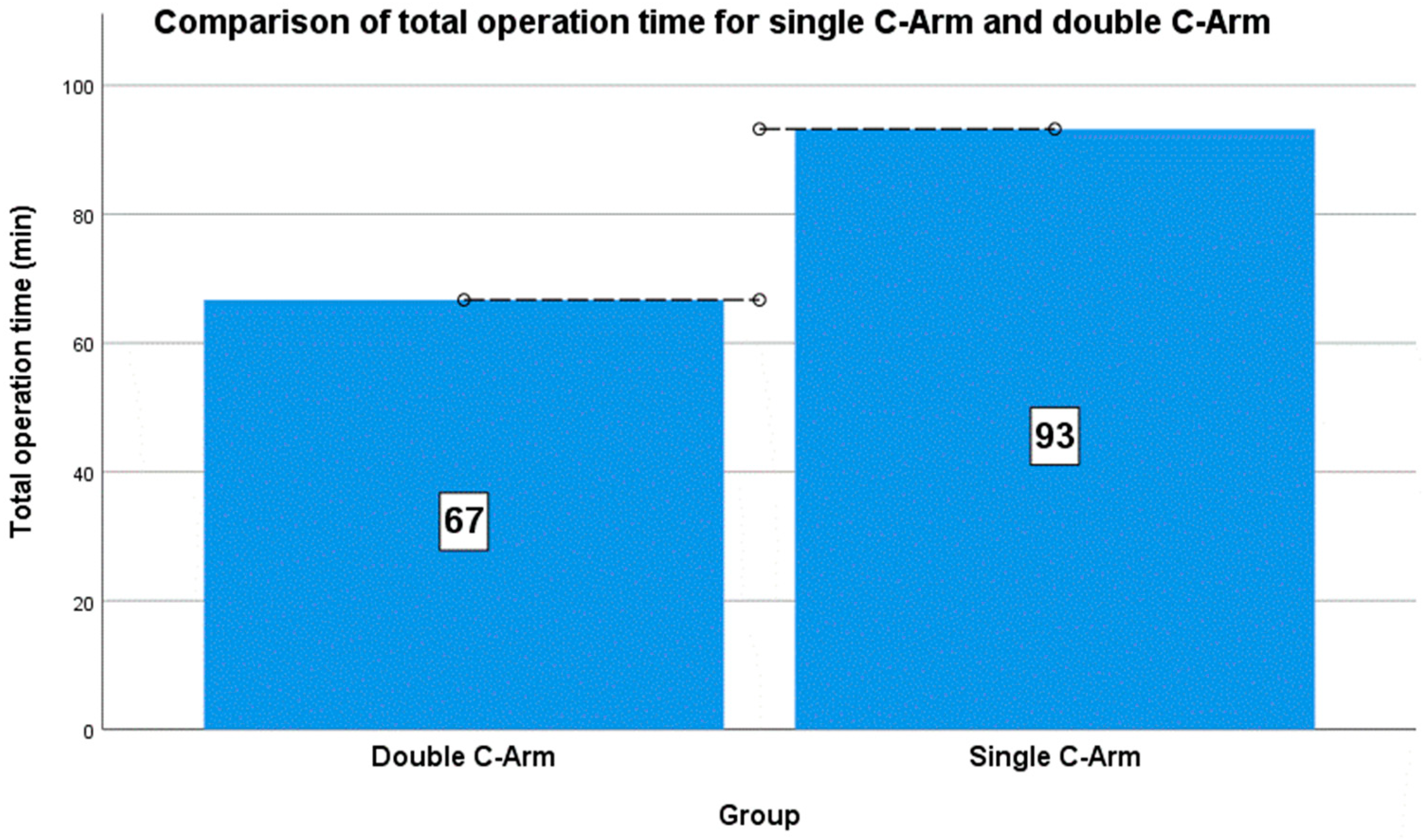
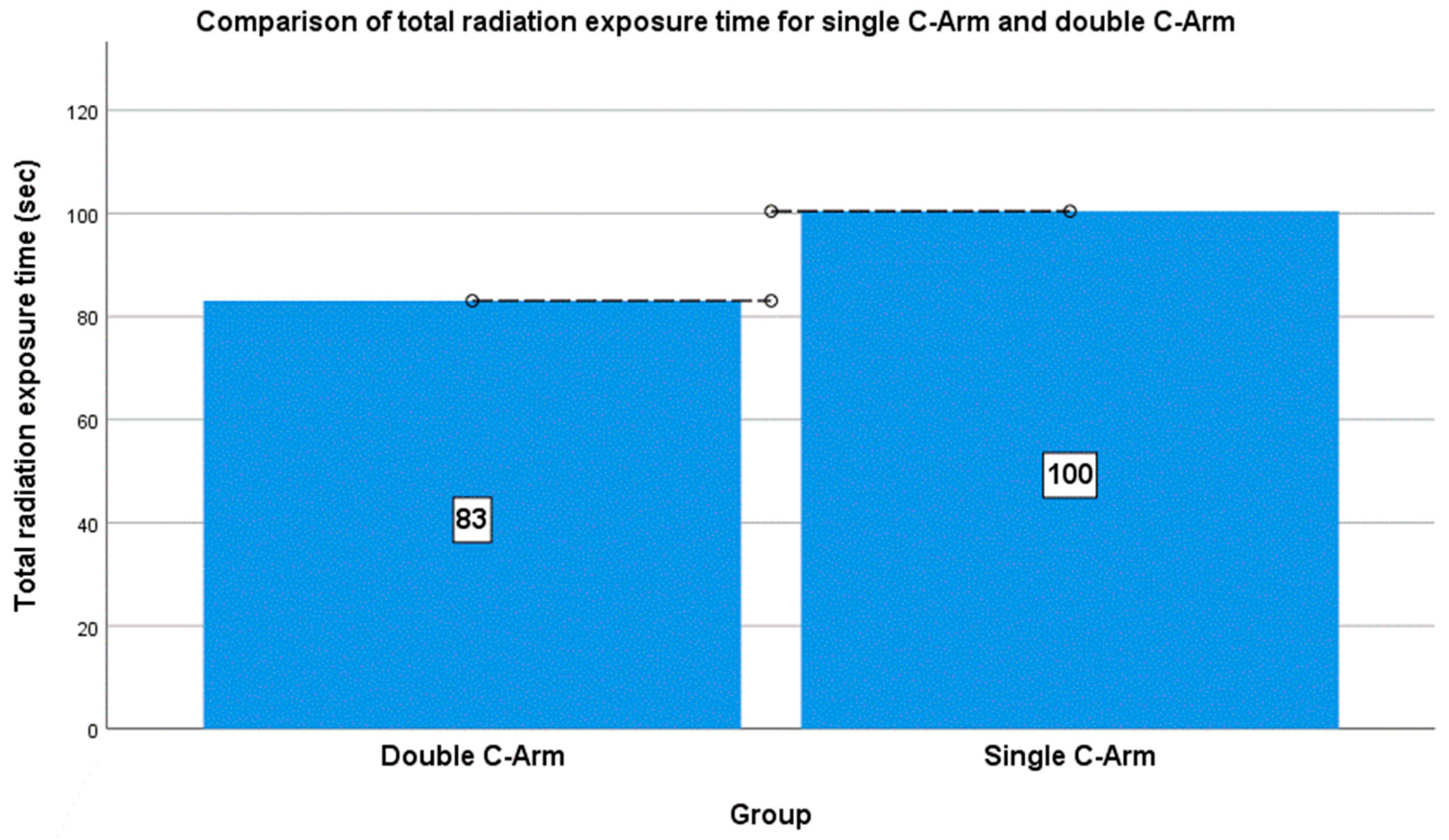
3.2. Comparison of Operation and Radiation Exposure Times between the Two Groups (Single and Double C-Arm Groups)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sterling, R.S. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin. Orthop. Relat. Res. 2011, 469, 1913–1918. [Google Scholar] [CrossRef]
- Zuckerman, J.D. Hip fracture. N. Engl. J. Med. 1996, 334, 1519–1525. [Google Scholar] [CrossRef] [PubMed]
- Menzies, I.B.; Mendelson, D.A.; Kates, S.L.; Friedman, S.M. The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr. Orthop. Surg. Rehabilt. 2012, 3, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Boszczyk, B.M.; Bierschneider, M.; Panzer, S.; Panzer, W.; Harstall, R.; Schmid, K.; Jaksche, H. Fluoroscopic radiation exposure of the kyphoplasty patient. Eur. Spine J. 2006, 15, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Samuel, S.; Saran, A.K.; Mahajan, M.K.; Mam, M.K. Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. J. Clin. Diagn. Res. 2015, 9, RC01–RC04. [Google Scholar] [CrossRef] [PubMed]
- Brin, Y.S.; Palmanovich, E.; Aliev, E.; Laver, L.; Yaacobi, E.; Nyska, M.; Kish, B.J. Closed reduction and internal fixation for intertrochanteric femoral fractures is safer and more efficient using two fluoroscopes simultaneously. Injury 2014, 45, 1071–1075. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; McGuigan, J.; Shaw, D.L. Ionizing radiation during internal fixation of extracapsular neck of femur fractures. Injury 1998, 29, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Kotil, K.; Sengoz, A.; Savas, Y. Cervical transpedicular fixation aided by biplanar flouroscopy. J. Orthop. Surg. 2011, 19, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Gülenç, B.; Günaydin, B.; Çamur, S.; Talmaç, M.A.; Güler, Y.; Kara, A. An effective technique in treatment of femoral neck fractures—Ostheosynthesis under double fluoroscopic guidance. Acta Chir. Orthop. Traumatol. Cechoslov. 2019, 86, 271–275. [Google Scholar] [CrossRef]
- Bout, C.A.; Cannegieter, D.M.; Juttmann, J.W. Percutaneous cannulated screw fixation of femoral neck fractures: The three point principle. Injury 1997, 28, 135–139. [Google Scholar] [CrossRef]
- Duffin, M.; Pilson, H.T. Technologies for young femoral neck fracture fixation. J. Orthop. Trauma 2019, 33, S20–S26. [Google Scholar] [CrossRef]
- Zhou, X.Q.; Li, Z.Q.; Xu, R.J.; She, Y.S.; Zhang, X.X.; Chen, G.X.; Yu, X. Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop. Surg. 2021, 13, 1802–1809. [Google Scholar] [CrossRef]
- Huang, S.; Zhang, Y.; Zhang, X.; Zhou, C.; Li, W.; Wang, Y.; Zhu, Z. Comparison of femoral neck system and three cannulated cancellous screws in the treatment of vertical femoral neck fractures: Clinical observation and finite element analysis. Biomed. Eng. Online. 2023, 22, 1–12. [Google Scholar] [CrossRef]
- Schueler, B.A.; Vrieze, T.J.; Bjarnason, H.; Stanson, A.W. An investigation of operator exposure in interventional radiology. Radiographics 2006, 26, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Singer, G. Occupational radiation exposure to the surgeon. J. Am. Acad. Orthop. Surg. 2005, 13, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.; Koval, K.J.; DiPasquale, T.; Schmelling, G.; Stenzler, S.; Ross, E. Exposure of the orthopaedic surgeon to radiation. J. Bone Jt. Surg. Am. 1993, 75, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Beebe, M.J.; Jenkins, P.; Rothberg, D.L.; Kubiak, E.N.; Higgins, T.F. Prospective assessment of the oncogenic risk to patients from fluoroscopy during trauma surgery. J. Orthop. Trauma 2016, 30, e223–e229. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, G.; Fedeli, U.; Fadda, E.; Giovanazzi, A.; Scoizzato, L.; Saia, B. Increased cancer risk among surgeons in an orthopaedic hospital. Occup. Med. 2005, 55, 498–500. [Google Scholar] [CrossRef] [PubMed]
- O’Rourke, P.J.; Crerand, S.; Harrington, P.; Casey, M.; Quinlan, W. Risks of radiation exposure to orthopaedic surgeons. J. R. Coll. Surg. Edinb. 1996, 41, 40–43. [Google Scholar] [PubMed]
- Crawley, M.T.; Rogers, A.T. Dose-area product measurements in a range of common orthopaedic procedures and their possible use in establishing local diagnostic reference levels. Br. J. Radiol. 2000, 73, 740–744. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.T.; Huang, K.C.; Chen, M.C.; Li, Y.Y.; Hsu, R.W. Percutaneous placement of iliosacral screws for unstable pelvic ring injuries: Comparison between one and two C-arm fluoroscopic techniques. J. Trauma 2006, 60, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.Y.; Huang, T.J.; Cheng, C.C.; Hsu, R.W. A comparison between one- and two-fluoroscopic techniques in percutaneous vertebroplasty. BMC Musculoskelet. Disord. 2008, 9, 67. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Shin, J.U.; Kim, S. Comparative study for osteosynthesis of femoral neck fractures: Cannulated screws versus femoral neck system. Hip Pelvis 2023, 35, 47. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J.; Solan, M.; Moore, E. Cone-beam computed tomography in orthopaedics. Orthop. Trauma 2022, 36, 194–201. [Google Scholar] [CrossRef]
- Sebaaly, A.; Jouffroy, P.; Moreau, P.E.; Rodaix, C.; Riouallon, G. Intraoperative cone beam tomography and navigation for displaced acetabular fractures: A comparative study. J. Orthop. Trauma 2018, 32, 612–616. [Google Scholar] [CrossRef]
- Costa, F.; Tosi, G.; Attuati, L.; Cardia, A.; Ortolina, A.; Grimaldi, M.; Fornari, M. Radiation exposure in spine surgery using an image-guided system based on intraoperative cone-beam computed tomography: Analysis of 107 consecutive cases. J. Neurosurg. Spine 2016, 25, 654–659. [Google Scholar] [CrossRef]
| Single C-Arm Group (n = 14) | Double C-Arm Group (n = 16) | p-Value 3 | |
|---|---|---|---|
| Sex, man/woman, n (%) | 10 (71.43)/4 (28.57) | 8 (50)/8 (50) | 0.232 2 |
| Age (years), mean (±SD) | 48.57 ± 20.01 | 50.94 ± 6.21 | 0.677 1 |
| BMI (kg/m2) 4, mean (±SD) | 22.22 ± 2.27 | 23.57 ± 3.07 | 0.189 1 |
| Anesthesia, general/spinal, n (%) | 8 (57.15)/6 (42.85) | 9 (56.25)/7 (43.75) | 0.961 2 |
| Garden classification, stage 3/4, n (%) | 5 (35.71)/9 (64.29) | 11 (68.75)/5 (31.25) | 0.070 2 |
| Single C-Arm (n = 14) | Double C-Arm (n = 16) | p-Value 3 | ||
|---|---|---|---|---|
| Radiation time (s) | Preparative | 19.93 ± 9.02 | 14.25 ± 7.31 | 0.038 2 |
| Intraoperative | 80.50 ± 17.65 | 68.00 ± 14.23 | 0.034 2 | |
| Total | 100.43 ± 24.59 | 83.06 ± 19.53 | 0.015 2 | |
| Operation time (min) | Preparative | 37.86 ± 6.99 | 28.75 ± 11.47 | 0.013 2 |
| Intraoperative | 55.36 ± 17.26 | 37.94 ± 6.55 | 0.002 2 | |
| total | 93.21 ± 20.70 | 66.69 ± 13.97 | 0.001 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.H.; Kang, K.-Y.; Sung, S.-Y.; Lee, S.-B.; Kim, S.-H.; Jung, S.-I.; Shin, D.H.; Oh, B.H.; Chae, D.-S. Femoral Neck Fractures Treated by Closed Reduction and Internal Fixation with the Double Fluoroscope Technique: A Preliminary Study. J. Clin. Med. 2024, 13, 1418. https://doi.org/10.3390/jcm13051418
Lee HH, Kang K-Y, Sung S-Y, Lee S-B, Kim S-H, Jung S-I, Shin DH, Oh BH, Chae D-S. Femoral Neck Fractures Treated by Closed Reduction and Internal Fixation with the Double Fluoroscope Technique: A Preliminary Study. Journal of Clinical Medicine. 2024; 13(5):1418. https://doi.org/10.3390/jcm13051418
Chicago/Turabian StyleLee, Hyun Hee, Kyung-Yil Kang, Seung-Yong Sung, Soo-Bin Lee, Sang-Hee Kim, Su-Il Jung, Dong Hyuk Shin, Byung Hak Oh, and Dong-Sik Chae. 2024. "Femoral Neck Fractures Treated by Closed Reduction and Internal Fixation with the Double Fluoroscope Technique: A Preliminary Study" Journal of Clinical Medicine 13, no. 5: 1418. https://doi.org/10.3390/jcm13051418
APA StyleLee, H. H., Kang, K.-Y., Sung, S.-Y., Lee, S.-B., Kim, S.-H., Jung, S.-I., Shin, D. H., Oh, B. H., & Chae, D.-S. (2024). Femoral Neck Fractures Treated by Closed Reduction and Internal Fixation with the Double Fluoroscope Technique: A Preliminary Study. Journal of Clinical Medicine, 13(5), 1418. https://doi.org/10.3390/jcm13051418






