Functional Outcomes in Upper Limb Replantation—A Systematic Review
Abstract
1. Introduction
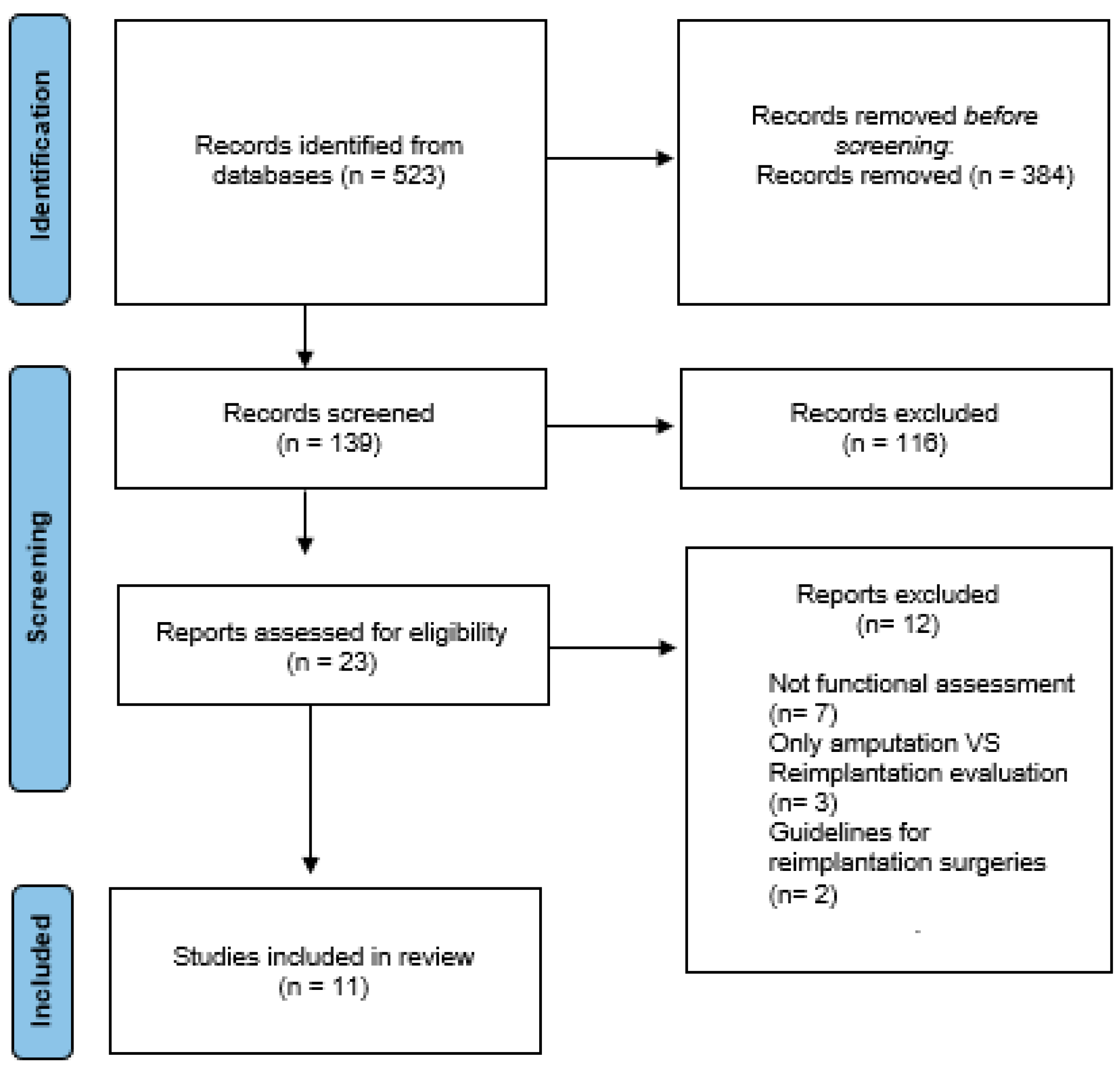
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Medling, B.D.; Bueno, R.A.; Russell, R.C.; Neumeister, M.W. Replantation outcomes. Clin. Plast. Surg. 2007, 34, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.H. Practical Tips to Improve Efficiency and Success in Upper Limb Replantation. Plast. Reconstr. Surg. 2019, 144, 878e–911e. [Google Scholar] [CrossRef] [PubMed]
- Barbary, S.; Dap, F.; Dautel, G. Finger replantation: Surgical technique and indications. Chir. Main 2013, 32, 363–372. [Google Scholar] [CrossRef]
- Sears, E.; Chung, K. Reimplantación de lesiones por avulsión de dedos: Una revisión sistemática de la supervivencia y los resultados funcionales. J. Hand Surg. Am. 2011, 36, 386–394. [Google Scholar] [CrossRef]
- Atkin Sara, E.; Winterton Robert, I.S.; Kay Simón, P. Upper limb amputations: Where, when and how to replant. Orthopaedics and trauma. Curr. Orthop. 2008, 22, 31–41. [Google Scholar] [CrossRef]
- Lara Guerrero, M.; Camporro Fernández, D.; Fernández Tárano, L.; García del Pozo, E. Measurement of replantation out-comes at Central University Hospital of Asturias (Spain): A retrospective study. Cir. Plást. Iberolati-Noam. Abril-Junio 2023, 49, 177–186. [Google Scholar]
- Camporro Fernández, D.; Barrio, L.; García del Pozo, E.; Contreras Pedraza, D.; Matarranz Faya, A. Principios de evalua¬ción y resultados funcionales en los reimplantes de miembro superior. Cir. Plást. Iberolatinoam. 2012, 38, 247–256. [Google Scholar] [CrossRef]
- Chuang, D.C.; Lai, J.B.; Cheng, S.L.; Jain, V.; Lin, C.H.; Chen, H.C. Traction avulsion amputation of the major upper limb: A proposed new classification, guidelines for acute management, and strategies for secondary reconstruction. Plast. Reconstr. Surg. 2001, 108, 1624–1638. [Google Scholar] [CrossRef]
- Tamai, S. Twenty years experience of limb replantation. Review of 293 upper limb reimplants. J. Hand Surg. 1982, 7, 549–556. [Google Scholar] [CrossRef]
- Ono, S.; Chung, K.C. Efficiency in Digital and Hand Replantation. Clin. Plast. Surg. 2019, 46, 359–370. [Google Scholar] [CrossRef]
- Khan, N.; Rashid, M.; Rashid, H.; Rehman Sarwar, S.; Khalid Choudry, U.; Khurshid, M. Resultados funcionales de los procedimientos secundarios en el reimplante y revascularización de las extremidades superiores. Cureus2 2019, 11, 5164. [Google Scholar] [CrossRef]
- Bott, S.; Rachunek, K.; Medved, F.; Bott, T.; Daigeler, A.; Wahler, T. Resultado funcional después del reimplante de dedos versus amputación. J. Orthop. Traumatol. 2022, 23, 35. [Google Scholar] [CrossRef] [PubMed]
- Urbaniak, J.R.; Evans, J.P.; Bright, D.S. Microvascular management of ring avulsion injuries. J. Hand Surg. Am. 1981, 6, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Kay, S.; Werntz, J.; Wolff, T.W. Ring avulsion injuries: Classification and prognosis. J. Hand Surg. Am. 1989, 14 Pt 1, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Axelrod, T.; Buchler, U. Lesiones complejas graves en la extremidad superior: Revascularización y reimplantación. J. Hand Surg. Am. 1991, 16, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Laing, T.; Cassell, O.; O’Donovan, D.; Eadie, P. Resultados funcionales a largo plazo de reimplantes importantes de extremidades. J. Plast. Reconstr. Aesthet. Surg. 2012, 65, 931–934. [Google Scholar] [CrossRef]
- Mattiassich, G.; Rittenschober, F.; Dorninger, L.; Rois, J.; Mittermayr, R.; Ortmaier, R.; Ponschab, M.; Katzensteiner, K.; Larcher, L. Resultado a largo plazo tras el reimplante de una extremidad superior después de una amputación traumática mayor. Trastor. Musculoesquelético BMC 2017, 18, 77. [Google Scholar] [CrossRef]
- Molski, M. Replantation of fingers and hands after avulsion and crush injuries. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 748–754. [Google Scholar] [CrossRef]
- Battison, B.; Tos, P.; Clemente, A.; Pontini, I. Actualities in big segment replantation surgery. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 849–855. [Google Scholar] [CrossRef]
- Sebastin, S.; Chung, K. Desafíos en la medición de los resultados después de la reimplantación digital. Cirugía Semin. Plast. 2013, 27, 174–181. [Google Scholar] [CrossRef]
- Hudak, P.; Amadio, P.; Bombardier, C. Desarrollo de una medida de resultado de las extremidades superiores: El DASH (discapacidades del brazo, hombro y mano) [corregido]. El Grupo Colaborativo de Extremidades Superiores (UECG). Soy. J. Ind. Med. 1996, 29, 302–308. [Google Scholar] [CrossRef]
- Carlsson, I.; Cederlund, R.; Höglund, P.; Lundborg, G.; Rosén, B. Lesiones en las manos y sensibilidad al frío: Confiabilidad y validez de los cuestionarios de sensibilidad al frío. Disabil. Rehabil. 2008, 30, 1920–1928. [Google Scholar] [CrossRef]
- Gummesson, C.; Ward, M.; Atroshi, I. Las discapacidades abreviadas del cuestionario de brazo, hombro y mano (QuickDASH): Validez y confiabilidad basadas en respuestas dentro del cuestionario DASH completo. Trastor. Musculoesquelético BMC 2006, 8, 44. [Google Scholar] [CrossRef]
- Chen, Z.; Yu, H. Procedimientos actuales en China sobre reimplantación de extremidades y dedos amputados. Clin. Orthop. Relat. Res. 1987, 215, 15–23. [Google Scholar]
- Chung, K.; Pillsbury, M.; Walters, M.; Hayward, R. Pruebas de confiabilidad y validez del Michigan Hand Outcomes Questionnaire. Cirugía Mano J. Am. 1998, 23, 575–587. [Google Scholar] [CrossRef]
- Colen, L.; Bunkis, J.; Gordon, L.; Walton, R. Evaluación funcional de la transferencia de rayos para la pérdida digital central. D. Mano Surg. 1985, 10, 232–237. [Google Scholar] [CrossRef]
- Goodson, A.; McGregor, A.; Douglas, J.; Taylor, P. Evaluación clínica cuantitativa directa de la función de la mano: Utilidad y reproducibilidad. Hombre Allí. 2007, 12, 144–152. [Google Scholar] [CrossRef]
- Granger, C.; Ottenbacher, K.; Fiedler, R. El sistema de datos uniforme para la rehabilitación médica. Informe de primeros ingresos de 1993. Am. J. Phys. Med. Rehabil. 1995, 74, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Dolan, P. Modelización de valoraciones para estados de salud EuroQol. Atención Méd. 1997, 35, 1095–1108. [Google Scholar] [CrossRef]
- Zung, W. Un instrumento de calificación para los trastornos de ansiedad. Psicosomativos 1971, 12, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.; Steer, R. Brown GKBDI-II. Inventario de depresión de Beck: Manual. In San Antonio; Psychological Corporation: New York, NY, USA, 1996. [Google Scholar]
- Carlson, E. Estudio psicométrico de una prueba breve para el trastorno de estrés postraumático: Evaluación del impacto de múltiples eventos traumáticos. Evaluación 2001, 8, 431–441. [Google Scholar] [CrossRef]
- Urbaniak, J.R.; Roth, J.H.; Nunley, J.A.; Goldner, R.D.; Koman, A. The results of replantation after single finger amputation. J. Bone Jt. Surg. Am. 1985, 67, 611–619. [Google Scholar] [CrossRef]
- Sabapathy, S.R.; Venkatramani, H.; Bharathi, R.; Bhardwaj, P. Replantation Surgery. J. Hand Surg. 2011, 36A, 1104. [Google Scholar] [CrossRef]
- Bath, A.; Acharya, A.; Narayanakurup, J.; Kumar, B.; Nagpal, P.; Kamath, A. Resultado funcional y cosmético de la amputación de rayos de un solo dígito en la mano. Cirugía Musculoesquelética 2017, 101, 275–281. [Google Scholar] [CrossRef]
- Gürbüz, K.; Yontar, Y. Una experiencia de cuatro años en un hospital comunitario con respecto a procedimientos para la reimplantación y revascularización de los dedos. Jt. Dis. Relar. Surg. 2021, 32, 383–390. [Google Scholar] [CrossRef]
- KYNg, W.; Nirmal Kaur, M.; Thoma, A. Resultados a largo plazo de reimplantes importantes de extremidades superiores. Cirugía Plástica. 2014, 22, 9–13. [Google Scholar]
- Giardi, D.; Crosio, A.; Da Rold, I.; Magistroni, E.; Tos, P.; Titolo, P.; Battiston, B.; Ciclamini, D. Resultados clínicos a largo plazo de 33 reimplantes de pulgar. Lesión 2020, 51, S71–S76. [Google Scholar] [CrossRef]
- Ciclamini, D.; Tos, P.; Magistroni, E.; Panero, B.; Titolo, P.; Da Rold, I.; Battiston, B. Resultados funcionales y subjetivos de 20 reimplantes de pulgar. Lesión 2013, 44, 504–507. [Google Scholar] [CrossRef]
- Rosberg, H.E. Discapacidad y salud después de la reimplantación o revascularización en la extremidad superior en una población del sur de Suecia: Un seguimiento retrospectivo a largo plazo. Trastor. Musculoesquelético BMC 2014, 15, 73. [Google Scholar] [CrossRef]
- Jiménez-Cortes, E.; López-Rios, A.; Vásquez-Sañudo, V.; Cardona-González, E. Estudio descriptivo de pacientes con amputación de miembro superior como posibles candidatos a trasplante de mano en Medellín, Colombia. Cureus 2022, 14, 22527. [Google Scholar] [CrossRef]
- Haas, F.; Hubner, M.; Rappl, T.; Koch, H.; Parvizi, I.; Parvizi, D. Long-term subjective and functional evaluation after thumb replantation with special attention to the Quick DASH questionnaire and a specially designed trauma score called modified mayo score. J. Trauma 2010, 20, 460–466. [Google Scholar] [CrossRef] [PubMed]
| Article | Type of Article | n |
|---|---|---|
| Functional Outcomes of Secondary Procedures in Upper Extremity Replantation and Revascularization | Prospective observational study | 40 |
| Long-term outcomes of major upper extremity replantations | Prospective study | 16 |
| Disability and health after replantation or revascularization in the upper extremity in a population in southern Sweden—a retrospective long time follow up | Retrospective study | 326 |
| Long-term outcome following upper extremity replantation after major traumatic amputation | Prospective study | 16 |
| Long-term functional, subjective and psychological results after single digit replantation | Prospective study | 30 |
| A four-year community hospital experience regarding procedures for the replantation and revascularization of fingers | Prospective study | 58 |
| Upper extremity replantation results in our series and review of replantation indications | Prospective study | 14 |
| Reconstructive surgery of the amputated ring finger | Retrospective study | 9 |
| Functional and subjective results of 20 thumb replantations | Prospective study | 20 |
| Long-term clinical results of 33 thumb replantations | Retrospective study | 33 |
| Functional and cosmetic outcome of single-digit ray amputation in hand | Prospective study | 45 |
| Characteristics (n = 607) | |
|---|---|
| Age, y (mean) | 38 |
| Male | 512 |
| Female | 95 |
| Mechanism of injury (n = 518) | |
| Cut | 407 |
| Crush | 80 |
| Avulsion | 26 |
| Self-inflicted | 5 |
| Level of injury (n = 606) | |
| Arm | 14 |
| Elbow and forearm | 31 |
| Wrist | 27 |
| Metacarpal | 29 |
| Fingers | 361 |
| Thumb | 144 |
| Scales | Number of Articles in Which They Appear |
|---|---|
| DASH (n = 160) | 6 |
| QuickDASH (n = 424) | 3 |
| CISS (n = 528) | 7 |
| Chen (n = 27) | 2 |
| MHQ (n = 46) | 2 |
| RAS (n = 54) | 2 |
| ROM (n = 87) | 3 |
| FIM (n = 16) | 1 |
| EQ-5D (n = 326) | 1 |
| SAS (n = 30) | 1 |
| BDI (n = 30) | 1 |
| SPTSS (n = 30) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bueno, A.; Nevado-Sanchez, E.; Collazo, C.; De la Fuente-Anuncibay, R.; González-Bernal, J. Functional Outcomes in Upper Limb Replantation—A Systematic Review. J. Clin. Med. 2024, 13, 1289. https://doi.org/10.3390/jcm13051289
Bueno A, Nevado-Sanchez E, Collazo C, De la Fuente-Anuncibay R, González-Bernal J. Functional Outcomes in Upper Limb Replantation—A Systematic Review. Journal of Clinical Medicine. 2024; 13(5):1289. https://doi.org/10.3390/jcm13051289
Chicago/Turabian StyleBueno, Andrea, Endika Nevado-Sanchez, Carla Collazo, Raquel De la Fuente-Anuncibay, and Jerónimo González-Bernal. 2024. "Functional Outcomes in Upper Limb Replantation—A Systematic Review" Journal of Clinical Medicine 13, no. 5: 1289. https://doi.org/10.3390/jcm13051289
APA StyleBueno, A., Nevado-Sanchez, E., Collazo, C., De la Fuente-Anuncibay, R., & González-Bernal, J. (2024). Functional Outcomes in Upper Limb Replantation—A Systematic Review. Journal of Clinical Medicine, 13(5), 1289. https://doi.org/10.3390/jcm13051289









