Validation of the Italian Version of the Web Screening Questionnaire for Common Mental Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Translation and Cultural Adaptation
2.2. Sample Size Determination
2.3. Participants
2.4. Procedures
2.5. Measures
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics
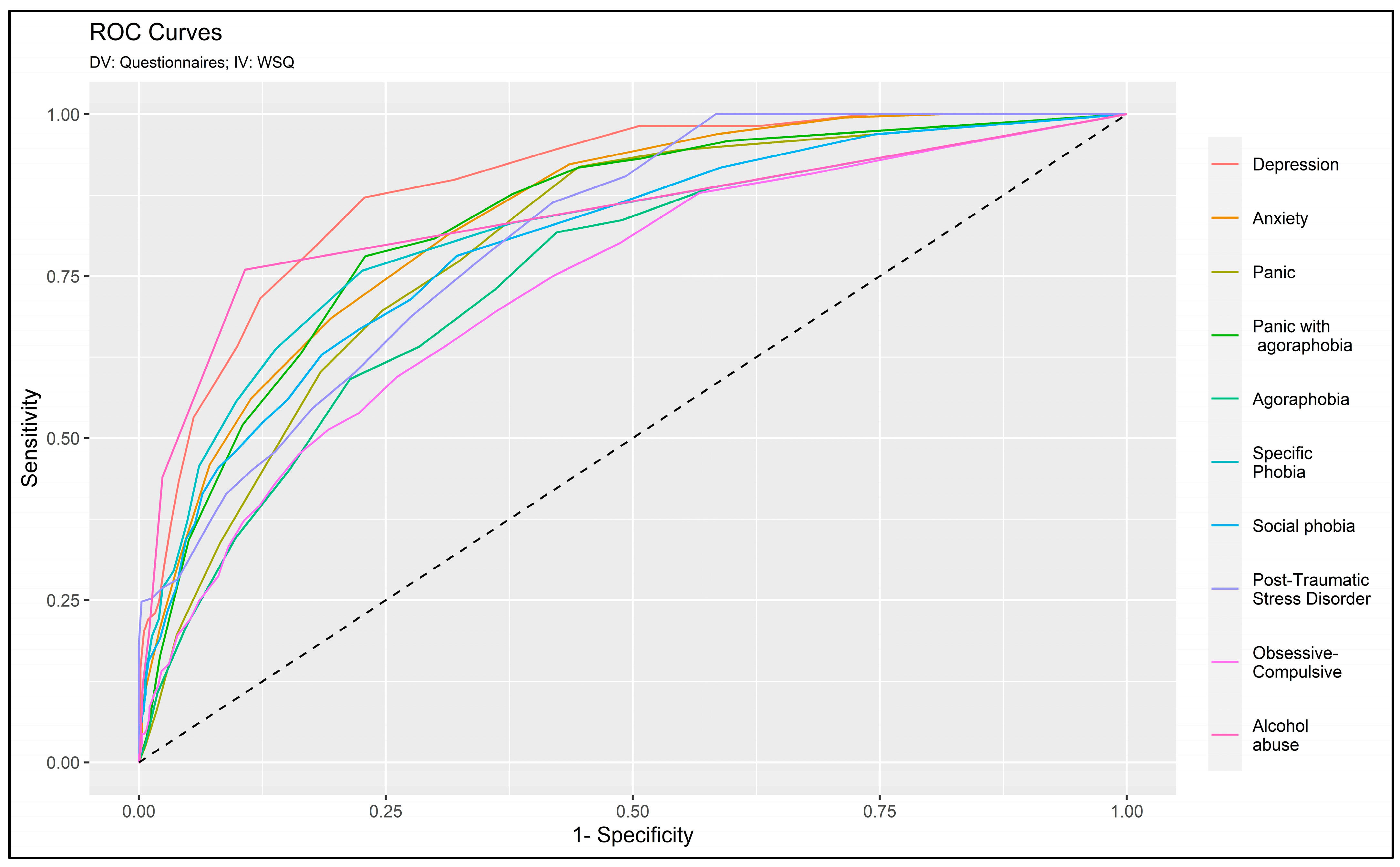
3.2. Concordance between the Screening Questionnaires and the Web Screening Questionnaire (WSQ)
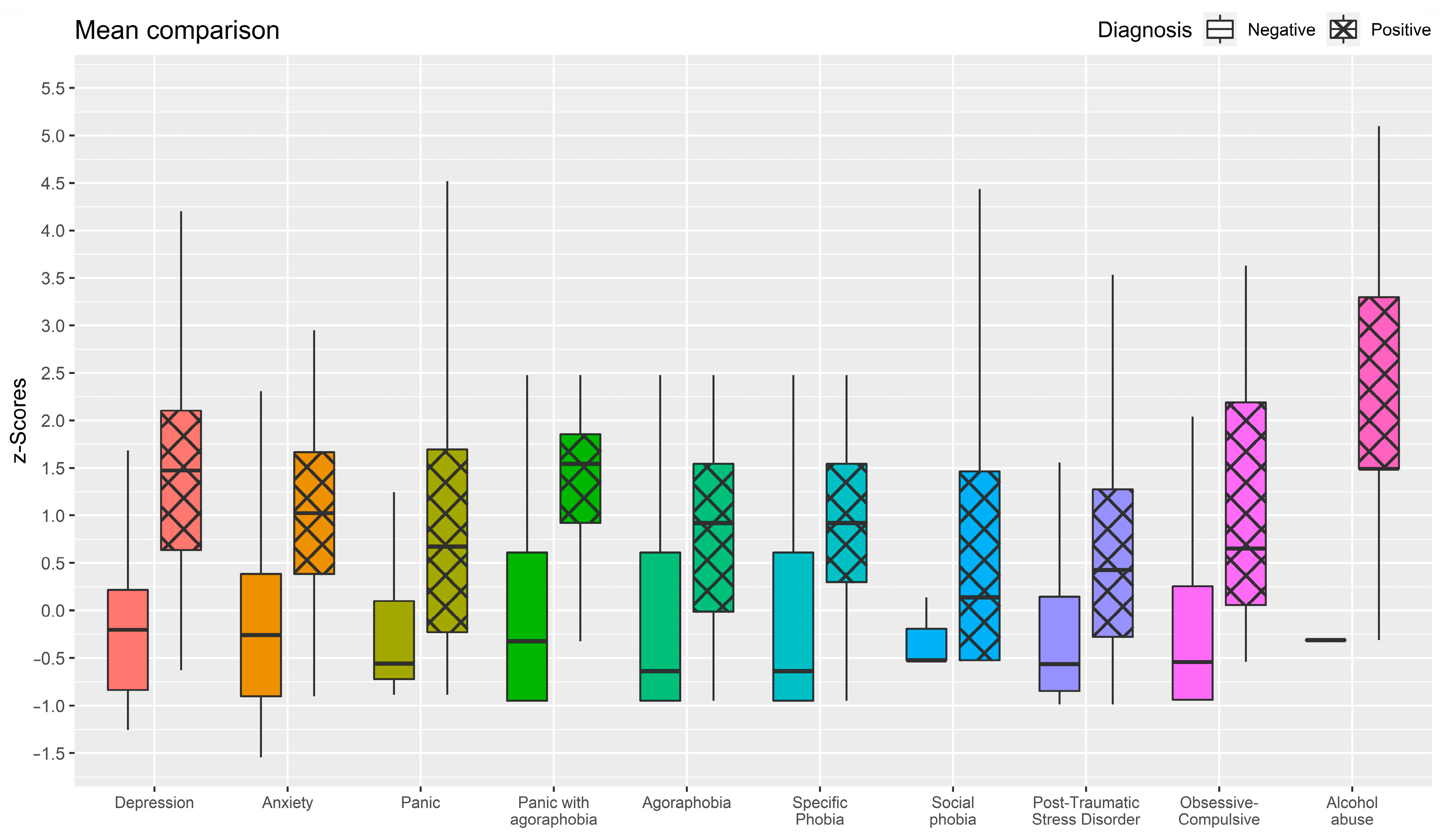
3.3. Assessing the Strength of Differences
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Semonella, M.; Andersson, G.; Dekel, R.; Pietrabissa, G.; Vilchinsky, N. Making a Virtue Out of Necessity: COVID-19 as a Catalyst for Applying Internet-Based Psychological Interventions for Informal Caregivers. Front. Psychol. 2022, 13, 856016. [Google Scholar] [CrossRef]
- Beatty, L.; Lambert, S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin. Psychol. Rev. 2013, 33, 609–622. [Google Scholar] [CrossRef]
- Hedman-Lagerlof, E.; Carlbring, P.; Svardman, F.; Riper, H.; Cuijpers, P.; Andersson, G. Therapist-supported Internet-based cognitive behaviour therapy yields similar effects as face-to-face therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. World Psychiatry 2023, 22, 305–314. [Google Scholar] [CrossRef]
- Carlbring, P.; Andersson, G.; Cuijpers, P.; Riper, H.; Hedman-Lagerlof, E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018, 47, 1–18. [Google Scholar] [CrossRef]
- Andersson, G.; Cuijpers, P.; Carlbring, P.; Riper, H.; Hedman, E. Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: A systematic review and meta-analysis. World Psychiatry 2014, 13, 288–295. [Google Scholar] [CrossRef]
- Van Ballegooijen, W.; Riper, H.; Klein, B.; Ebert, D.D.; Kramer, J.; Meulenbeek, P.; Cuijpers, P. An Internet-based guided self-help intervention for panic symptoms: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e154. [Google Scholar] [CrossRef] [PubMed]
- Kahlke, F.; Berger, T.; Schulz, A.; Baumeister, H.; Berking, M.; Auerbach, R.P.; Bruffaerts, R.; Cuijpers, P.; Kessler, R.C.; Ebert, D.D. Efficacy of an unguided internet-based self-help intervention for social anxiety disorder in university students: A randomized controlled trial. Int. J. Methods Psychiatr. Res. 2019, 28, e1766. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Donker, T.; Johansson, R.; Mohr, D.C.; van Straten, A.; Andersson, G. Self-guided psychological treatment for depressive symptoms: A meta-analysis. PLoS ONE 2011, 6, e21274. [Google Scholar] [CrossRef] [PubMed]
- Kass, A.E.; Trockel, M.; Safer, D.L.; Sinton, M.M.; Cunning, D.; Rizk, M.T.; Genkin, B.H.; Weisman, H.L.; Bailey, J.O.; Jacobi, C.; et al. Internet-based preventive intervention for reducing eating disorder risk: A randomized controlled trial comparing guided with unguided self-help. Behav. Res. Ther. 2014, 63, 90–98. [Google Scholar] [CrossRef]
- Eimontas, J.; Rimsaite, Z.; Gegieckaite, G.; Zelviene, P.; Kazlauskas, E. Internet-Based Self-Help Intervention for ICD-11 Adjustment Disorder: Preliminary Findings. Psychiatr. Q. 2018, 89, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Hedman, E.; Ljotsson, B.; Kaldo, V.; Hesser, H.; El Alaoui, S.; Kraepelien, M.; Andersson, E.; Ruck, C.; Svanborg, C.; Andersson, G.; et al. Effectiveness of Internet-based cognitive behaviour therapy for depression in routine psychiatric care. J. Affect. Disord. 2014, 155, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Mathiasen, K.; Riper, H.; Andersen, T.E.; Roessler, K.K. Guided Internet-Based Cognitive Behavioral Therapy for Adult Depression and Anxiety in Routine Secondary Care: Observational Study. J. Med. Internet Res. 2018, 20, e10927. [Google Scholar] [CrossRef]
- Whitton, A.E.; Hardy, R.; Cope, K.; Gieng, C.; Gow, L.; MacKinnon, A.; Gale, N.; O’Moore, K.; Anderson, J.; Proudfoot, J.; et al. Mental Health Screening in General Practices as a Means for Enhancing Uptake of Digital Mental Health Interventions: Observational Cohort Study. J. Med. Internet Res. 2021, 23, e28369. [Google Scholar] [CrossRef] [PubMed]
- Bertuzzi, V.; Semonella, M.; Castelnuovo, G.; Andersson, G.; Pietrabissa, G. Synthesizing Stakeholders Perspectives on Online Psychological Interventions to Improve the Mental Health of the Italian Population during the COVID-19 Pandemic: An Online Survey Study. Int. J. Environ. Res. Public. Health 2022, 19, 7008. [Google Scholar] [CrossRef] [PubMed]
- Marks, I.M.; Cuijpers, P.; Cavanagh, K.; van Straten, A.; Gega, L.; Andersson, G. Meta-analysis of computer-aided psychotherapy: Problems and partial solutions. Cogn. Behav. Ther. 2009, 38, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Marks, I.M.; Cavanagh, K.; Gega, L. Computer-aided psychotherapy: Revolution or bubble? Br. J. Psychiatry 2007, 191, 471–473. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Cuijpers, P.; Carlbring, P.; Lindefors, N. Effects of Internet-delivered cognitive behaviour therapy for anxiety and mood disorders. Psychiatry Investig. 2007, 1, 9–14. [Google Scholar]
- Carlbring, P.; Nilsson-Ihrfelt, E.; Waara, J.; Kollenstam, C.; Buhrman, M.; Kaldo, V.; Soderberg, M.; Ekselius, L.; Andersson, G. Treatment of panic disorder: Live therapy vs. self-help via the Internet. Behav. Res. Ther. 2005, 43, 1321–1333. [Google Scholar] [CrossRef]
- Andersson, G.; Titov, N. Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry 2014, 13, 4–11. [Google Scholar] [CrossRef]
- Jäckle, A.; Roberts, C.; Lynn, P. Assessing the effect of data collection mode on measurement. Int. Stat. Rev. 2010, 78, 3–20. [Google Scholar] [CrossRef]
- Wyatt, J. Same information, different decisions: Format counts. Format as well as content matters in clinical information. BMJ 1999, 318, 1501–1502. [Google Scholar] [CrossRef]
- Determann, D.; Lambooij, M.S.; Steyerberg, E.W.; de Bekker-Grob, E.W.; de Wit, G.A. Impact of Survey Administration Mode on the Results of a Health-Related Discrete Choice Experiment: Online and Paper Comparison. Value Health 2017, 20, 953–960. [Google Scholar] [CrossRef]
- Norman, R.; King, M.T.; Clarke, D.; Viney, R.; Cronin, P.; Street, D. Does mode of administration matter? Comparison of online and face-to-face administration of a time trade-off task. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2010, 19, 499–508. [Google Scholar] [CrossRef]
- Saloniki, E.C.; Malley, J.; Burge, P.; Lu, H.; Batchelder, L.; Linnosmaa, I.; Trukeschitz, B.; Forder, J. Comparing internet and face-to-face surveys as methods for eliciting preferences for social care-related quality of life: Evidence from England using the ASCOT service user measure. Qual. Life Res. Int. J. Qual. Life Asp. Treat., Care Rehabil. 2019, 28, 2207–2220. [Google Scholar] [CrossRef]
- Coles, M.E.; Cook, L.M.; Blake, T.R. Assessing obsessive compulsive symptoms and cognitions on the internet: Evidence for the comparability of paper and Internet administration. Behav. Res. Ther. 2007, 45, 2232–2240. [Google Scholar] [CrossRef]
- Carlbring, P.; Brunt, S.; Bohman, S.; Austin, D.; Richards, J.; Öst, L.G.; Andersson, G. Internet vs. paper and pencil administration of questionnaires commonly used in panic/agoraphobia research. Comp. Human. Behav. 2007, 23, 1421–1434. [Google Scholar] [CrossRef]
- Hedman, E.; Ljótsson, B.; Rück, C.; Furmark, T.; Carlbring, P.; Lindefors, N.; Andersson, G. Internet administration of self-report measures commonly used in research on social anxiety disorder: A psychometric evaluation. Comput. Hum. Behav. 2010, 26, 736–740. [Google Scholar] [CrossRef]
- Buchanan, T. Internet-based questionnaire assessment: Appropriate use in clinical contexts. Cogn. Behav. Ther. 2003, 32, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Donker, T.; van Straten, A.; Marks, I.; Cuijpers, P. A brief Web-based screening questionnaire for common mental disorders: Development and validation. J. Med. Internet Res. 2009, 11, e19. [Google Scholar] [CrossRef] [PubMed]
- Gega, L.; Kenwright, M.; Mataix-Cols, D.; Cameron, R.; Marks, I.M. Screening people with anxiety/depression for suitability for guided self-help. Cogn. Behav. Ther. 2005, 34, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Guillemin, F.; Bombardier, C.; Beaton, D.E. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
- Hajian-Tilaki, K. Sample size estimation in diagnostic test studies of biomedical informatics. J. Biomed. Inform. 2014, 48, 193–204. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Aspetti Epidemiologici. 2018. Available online: https://www.epicentro.iss.it/infettive/archivio2018 (accessed on 15 February 2024).
- Consoli, S.; Rossi, A.; Thompson, L.Y.; Volpi, C.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Assessing Psychometric Properties of the Italian Version of the Heartland Forgiveness Scale. Front. Psychol. 2020, 11, 596501. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2023, 15, 104. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Pietrabissa, G.; Gearhardt, A.N.; Musetti, A.; Castelnuovo, G.; Mannarini, S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients 2023, 15, 1378. [Google Scholar] [CrossRef]
- Rossi, A.A.; Panzeri, A.; Taccini, F.; Parola, A.; Mannarini, S. The Rising of the Shield hero. Development of the Post-Traumatic Symptom Questionnaire (PTSQ) and Assessment of the Protective Effect of self-esteem from trauma-related Anxiety and Depression. J. Child Adolesc. Trauma 2022, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Invernizzi, R.; Mannarini, S.; Fernandez, I. La valutazione dell’evento di vita stressante / traumatico: Strumenti self-report per la pratica clinica e la ricerca. In L’EMDR nei Contesti Ospedalieri. Protocolli D’intervento a Favore dei Pazienti e del Personale Sanitario; Lo Nigro, T., Ed.; MIMESIS: Milano, Italy, 2023; pp. 117–132. [Google Scholar]
- Rossi, A.A.; Panzeri, A.; Fernandez, I.; Invernizzi, R.; Taccini, F.; Mannarini, S. Shedding Light on the Impact of Traumatic Event. Sci. Rep. 2024; (Submitted). [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Mazzone, E.; Fassone, G.; Picardi, A.; Sagoni, E.; Ramieri, L.; Lega, I.; Camaioni, D.; Abeni, D.; Pasquini, P. Il Patient Health Questionnaire (PHQ) per lo screening dei disturbi psichiatrici: Uno studio di validazione nei confronti della Intervista Clinica Strutturata per il DSM-IV asse I (SCID-I). J. Psychopathol. 2003, 9, 235–242. [Google Scholar]
- Prunas, A.; Sarno, I.; Preti, E.; Madeddu, F.; Perugini, M. Psychometric properties of the Italian version of the SCL-90-R: A study on a large community sample. Eur. Psychiatry 2012, 27, 591–597. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1998, 240, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Zou, K.H.; Liu, A.; Bandos, A.I.; Ohno-Machado, L.; Rockette, H.E. Statistical Evaluation of Diagnostic Performance: Topics in ROC Analysis; Chapman & Hall/CRC Biostatistics Series; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Pastore, M.; Calcagni, A. Measuring Distribution Similarities Between Samples: A Distribution-Free Overlapping Index. Front. Psychol. 2019, 10, 1089. [Google Scholar] [CrossRef] [PubMed]
- Huberty, C.J.; Lowman, L.L. Group overlap as a basis for effect size. Educ. Psychol. Meas. 2000, 60, 543–563. [Google Scholar] [CrossRef]
- Meuldijk, D.; Giltay, E.J.; Carlier, I.V.; van Vliet, I.M.; van Hemert, A.M.; Zitman, F.G. A Validation Study of the Web Screening Questionnaire (WSQ) Compared With the Mini-International Neuropsychiatric Interview-Plus (MINI-Plus). JMIR Ment. Health 2017, 4, e35. [Google Scholar] [CrossRef]
- Bertuzzi, V.; Semonella, M.; Andersson, G.; Manzoni, G.M.; Castelnuovo, G.; Molinari, E.; Pietrabissa, G. Study protocol for a randomized controlled trial evaluating the effectiveness of an internet-based self-help intervention to cope with psychological distress due to COVID-19 in the Italian general population: The RinasciMENTE project. Trials 2022, 23, 801. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Marchesi, G.; Semonella, M.; Andersson, G.; Castelnuovo, G. The RinasciMENTE 2.0 Project: A Study Protocol for A Randomized Controlled Trial Evaluating the Efficacy of An Internet-Based Self-Help Program for Managing Psychological Distress Within the Broader Italian Population. In Proceedings of the EAI PervasiveHealth 2023—17th EAI International Conference on Pervasive Computing Technologies for Healthcare, Malmö, Sweden, 27–29 November 2023. [Google Scholar]
| n | % | |
|---|---|---|
| Civil status (n, %) | ||
| Single | 246 | 19.2% |
| In a relationship | 421 | 32.8% |
| Married | 508 | 39.6% |
| Separated | 41 | 3.2% |
| Divorced | 50 | 3.9% |
| Widowed | 16 | 1.2% |
| Education (n, %) | ||
| Middle school degree | 74 | 5.8% |
| Professional qualification | 70 | 5.58% |
| High school degree | 491 | 38.38% |
| Bachelor degree | 167 | 13.08% |
| Master degree | 367 | 28.68% |
| Ph.D. | 113 | 8.88% |
| Job status (n, %) | ||
| Student | 148 | 11.5% |
| Employee worker | 657 | 51.2% |
| Freelance worker | 227 | 17.7% |
| Unemployed | 45 | 3.5% |
| Housewife | 72 | 5.6% |
| Retired | 56 | 4.4% |
| Other | 77 | 6.0% |
| Diagnosed mental health disorder (n, %) | ||
| None | 693 | 54.1% |
| Anxiety | 416 | 32.4% |
| Obsessive-compulsive disorder | 30 | 2.3% |
| Depression | 157 | 12.2% |
| EDs | 107 | 8.3% |
| Sexual Disorders | 19 | 1.5% |
| Post-traumatic stress disorder (PTSD) | 82 | 6.4% |
| Substance-use related disorders (SRAD) | 8 | 0.6% |
| Specific phobia | 11 | 0.9% |
| Personality disorders | 16 | 1.2% |
| Psychosis | 5 | 0.4% |
| Other | 21 | 1.6% |
| Mental health consultation (n, %) | ||
| None | 682 | 53.2% |
| Psychiatrist | 140 | 29.6% |
| Psychologist | 380 | 29.6% |
| Psychotherapist | 236 | 18.4% |
| Other professional | 20 | 1.6% |
| Psychiatric drug (n, %) | ||
| Yes | 105 | 8.2% |
| No | 1177 | 91.8% |
| χ2 | AUC | ACC | SPE | SEN | NPV | PPV | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PHQ9 Diagnosis | ||||||||||
| Depressive disorder | No | Yes | ||||||||
| WSQ-depression | No | 1029 | 144 | 240.68 * | 0.891 | 0.863 | 0.877 | 0.716 | 0.971 | 0.351 |
| Yes | 31 | 78 | [0.862, 0.919] | [0.843, 0.882] | [0.858, 0.895] | [0.624, 0.798] | [0.962, 0.979] | [0.306, 0.397] | ||
| GAD7 Diagnosis | ||||||||||
| Generalized anxiety disorder | No | Yes | ||||||||
| WSQ-anxiety | No | 1043 | 45 | 154.32 * | 0.840 | 0.861 | 0.959 | 0.314 | 0.887 | 0.575 |
| Yes | 133 | 61 | [0.814, 0.867] | [0.847, 0.875] | [0.946, 0.970] | [0.253, 0.376] | [0.878, 0.896] | [0.490, 0.663] | ||
| SCL-90-R INT SENS | ||||||||||
| Social phobia | No | Yes | ||||||||
| WSQ-Social Phobia | No | 898 | 128 | 197.83 * | 0.799 | 0.805 | 0.875 | 0.523 | 0.880 | 0.511 |
| Yes | 122 | 134 | [0.769, 0.830] | [0.785, 0.824] | [0.855, 0.895] | [0.465, 0.586] | [0.867, 0.895] | [0.464, 0.562] | ||
| Panic Diagnosis | ||||||||||
| Panic disorder | No | Yes | ||||||||
| WSQ-Panic | No | 1020 | 28 | 184.13 * | 0.799 | 0.848 | 0.973 | 0.286 | 0.859 | 0.705 |
| Yes | 167 | 67 | [0.770, 0.827] | [0.839, 0.858] | [0.964, 0.981] | [0.251, 0.315] | [0.854, 0.864] | [0.558, 0.852] | ||
| Panic Diagnosis | ||||||||||
| Panic with agoraphobia | No | Yes | ||||||||
| WSQ-Panic and Agoraph. | No | 1143 | 66 | 112.88 * | 0.832 | 0.914 | 0.945 | 0.397 | 0.963 | 0.305 |
| Yes | 44 | 29 | [0.787, 0.877] | [0.902, 0.928] | [0.939, 0.967] | [0.302, 0.492] | [0.957, 0.969] | [0.227, 0.383] | ||
| Panic Diagnosis | ||||||||||
| Agoraphobia | No | Yes | ||||||||
| WSQ-Agoraphobia | No | 1064 | 59 | 58.865 * | 0.746 | 0.858 | 0.947 | 0.226 | 0.896 | 0.379 |
| Yes | 123 | 36 | [0.706, 0.786] | [0.845, 0.871] | [0.934, 0.960] | [0.163, 0.289] | [0.888, 0.904] | [0.287, 0.471] | ||
| SCL-90-R PHOB ANX | ||||||||||
| Specific phobia | No | Yes | ||||||||
| WSQ-Specific Phobia | No | 1106 | 27 | 154.19 * | 0.811 | 0.894 | 0.976 | 0.268 | 0.910 | 0.597 |
| Yes | 109 | 40 | [0.772, 0.851] | [0.882, 0.906] | [0.967, 0.984] | [0.201, 0.342] | [0.903, 0.918] | [0.487, 0.707] | ||
| SCL-90-R OCD | ||||||||||
| Obsessive-compulsive disorder | No | Yes | ||||||||
| WSQ-OCD | No | 771 | 149 | 134.09 * | 0.732 | 0.736 | 0.838 | 0.475 | 0.802 | 0.536 |
| Yes | 190 | 172 | [0.702, 0.762] | [0.713, 0.757] | [0.815, 0.861] | [0.420, 0.528] | [0.785, 0.819] | [0.490, 0.581] | ||
| PTSQ-SF Diagnosis | ||||||||||
| Post-traumatic stress disorder | No | Yes | ||||||||
| WSQ-PTSD | No | 961 | 123 | 134.54 * | 0.810 | 0.819 | 0.887 | 0.449 | 0.898 | 0.420 |
| Yes | 109 | 89 | [0.781, 0.838] | [0.800, 0.839] | [0.868, 0.905] | [0.384, 0.520] | [0.887, 0.910] | [0.367, 0.477] | ||
| Alcohol Diagnosis | ||||||||||
| Alcohol abuse/dependence | No | Yes | ||||||||
| WSQ-Alcohol | No | 1138 | 119 | 106.14 * | 0.841 | 0.902 | 0.905 | 0.760 | 0.995 | 0.138 |
| Yes | 6 | 19 | [0.752, 0.931] | [0.884, 0.920] | [0.886, 0.924] | [0.560, 0.920] | [0.990, 0.998] | [0.108, 0.168] | ||
| Diagnosis on WSQ | Statistics | |||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| M (SD) | M (SD) | t | p-value | g | 1 − η | |
| Depression (range 0–27) | 5.278 (3.986) | 13.505 (5.870) | −14.328 | <0.001 | 1.97 | 0.591 |
| Anxiety (range 0–21) | 4.210 (2.777) | 8.170 (2.755) | −18.317 | <0.001 | 1.43 | 0.471 |
| Social Phobia (range 0–4) | 0.442 (0.520) | 1.237 (0.847) | −14.367 | <0.001 | 1.33 | 0.435 |
| Panic (range 0–11) | 2.407 (2.932) | 5.889 (2.847) | −16.509 | <0.001 | 1.19 | 0.384 |
| Panic with Agoraphobia (range 0–11) | 2.806 (3.080) | 6.973 (2.764) | −12.425 | <0.001 | 1.36 | 0.468 |
| Agoraphobia (range 0–11) | 2.674 (3.036) | 5.648 (3.214) | −11.474 | <0.001 | 0.97 | 0.324 |
| Specific phobia (range 0–4) | 0.106 (0.240) | 0.382 (0.558) | −10.895 | <0.001 | 1.61 | 0.615 |
| Obsessive-compulsive (range 0–4) | 0.531 (0.580) | 1.122 (0.819) | −12.537 | <0.001 | 0.90 | 0.330 |
| Post-Traumatic Stress (range 6–36) | 9.758 (4.132) | 15.980 (6.184) | −13.612 | <0.001 | 1.38 | 0.365 |
| Alcohol abuse (range 0–5) | 0.146 (0.494) | 1.520 (1.295) | −5.296 | <0.001 | 2.64 | 0.732 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pietrabissa, G.; Semonella, M.; Marchesi, G.; Mannarini, S.; Castelnuovo, G.; Andersson, G.; Rossi, A.A. Validation of the Italian Version of the Web Screening Questionnaire for Common Mental Disorders. J. Clin. Med. 2024, 13, 1170. https://doi.org/10.3390/jcm13041170
Pietrabissa G, Semonella M, Marchesi G, Mannarini S, Castelnuovo G, Andersson G, Rossi AA. Validation of the Italian Version of the Web Screening Questionnaire for Common Mental Disorders. Journal of Clinical Medicine. 2024; 13(4):1170. https://doi.org/10.3390/jcm13041170
Chicago/Turabian StylePietrabissa, Giada, Michelle Semonella, Gloria Marchesi, Stefania Mannarini, Gianluca Castelnuovo, Gerhard Andersson, and Alessandro Alberto Rossi. 2024. "Validation of the Italian Version of the Web Screening Questionnaire for Common Mental Disorders" Journal of Clinical Medicine 13, no. 4: 1170. https://doi.org/10.3390/jcm13041170
APA StylePietrabissa, G., Semonella, M., Marchesi, G., Mannarini, S., Castelnuovo, G., Andersson, G., & Rossi, A. A. (2024). Validation of the Italian Version of the Web Screening Questionnaire for Common Mental Disorders. Journal of Clinical Medicine, 13(4), 1170. https://doi.org/10.3390/jcm13041170








