Femoral–Obturator–Sciatic (FOS) Nerve Block as an Anesthetic Triad for Arthroscopic ACL Reconstruction: Is This the Magic Trick We Were Missing?
Abstract
1. Introduction
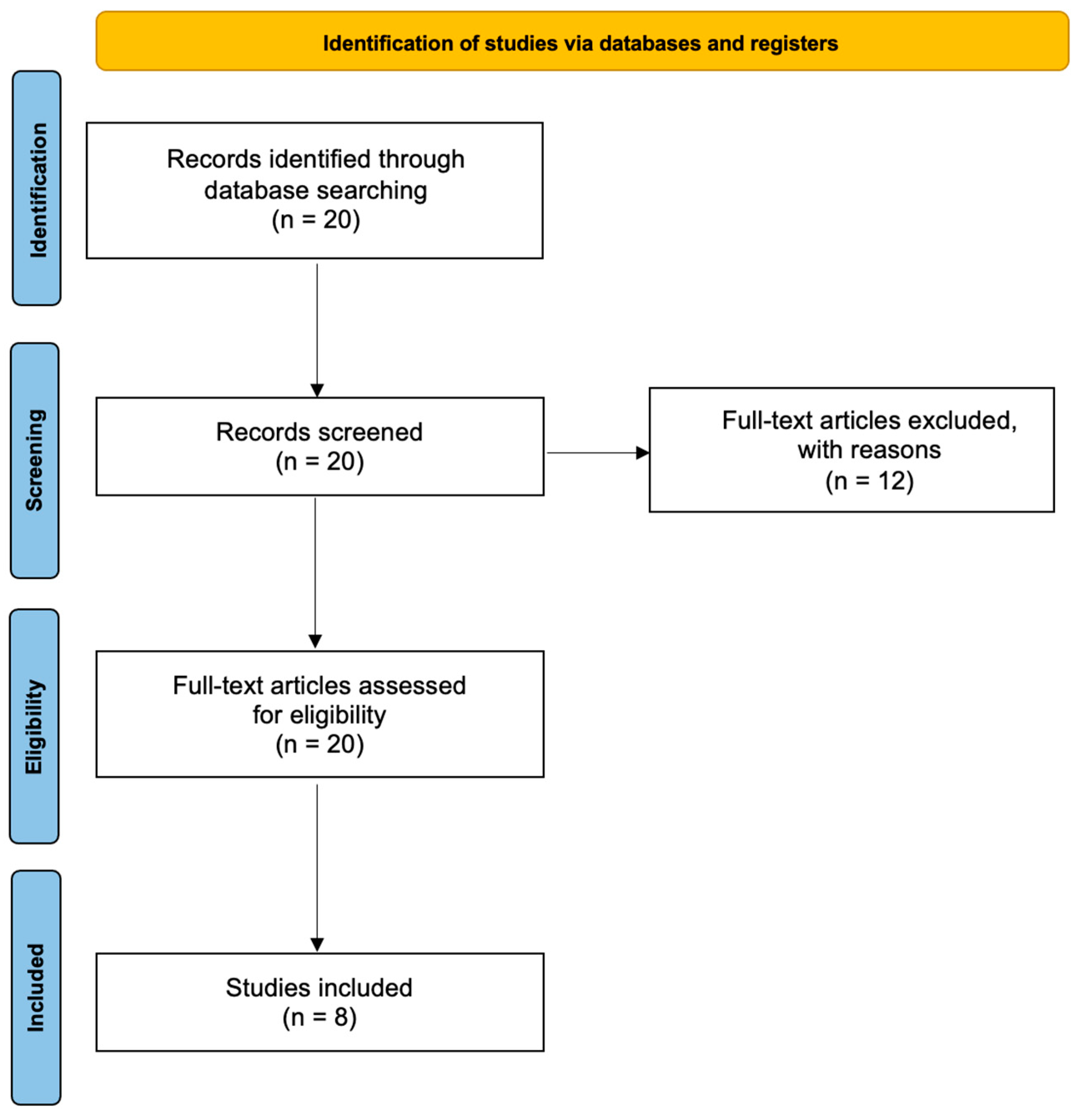
2. Materials and Methods
2.1. Data Sources/Search Strategy
- Obturator nerve block;
- Anterior cruciate ligament;
- Anesthesia.
2.2. Study Inclusion and Exclusion Criteria
- Population: The population of interest was adult patients undergoing arthroscopic ACL reconstruction under PNBs as the sole anesthetic technique;
- Intervention: The investigated intervention was the performance of three separate PNBs, i.e., (i) femoral (F), (ii) obturator (O), and (iii) sciatic (S), abbreviated as the FOS intervention;
- Comparison: The comparison was not specified;
- Outcome: The effectiveness, the adequacy (measured by incomplete analgesia and failure of the anesthetic technique) and the safety (measured by the appearance of complications) of performing three separate PNBs (femoral, obturator, and sciatic; FOS) as an exclusive method for anesthesia, in patients undergoing ACL reconstruction;
- Study selection: All cases, case series, observational or interventional studies (randomized or quasi-randomized clinical trials) were included. Reviews, narrative or systematic, meta-analyses, and qualitative research were excluded. In addition, only articles in the English language were included.
2.3. Data Extraction
3. Results
3.1. Number of Patient Groups in Included Studies
3.2. Peripheral Nerve Block Technique
3.3. Local Anesthetic Mixture and Dosage
3.4. Incomplete Analgesia and Failure of Anesthetic Technique
| Study ID | Type of Study | Number of Patients | PNB Technique | PNB1 | PNB2 | Evaluation Method for ONB | Incomplete SNB | Conversion to GA | Need for Supplementary Analgesic | Neurovascular Complications | Evaluation of Postoperative Pain Control | Patient or Physician Satisfaction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Helayel [18], 2007 Brazil | Prospective | 22 | Dual | N/A | FOS | Sensory: Diminished sensitivity or loss of pinprick sensation over the anterior, medial, lateral, and posterior aspects of the thigh and knee Motion: Sphygmomanometer | N/A | No | 3 patients (14%) | No | No | N/A |
| Sakura [14], 2010 Japan | Prospective | 21 | Dual | F-LFC-S | F-LFC-O-S | Manual evaluation of ON function | 1 in 21 (4.8%) | No | 6 patients (28.5%) | No | Yes | N/A |
| Tharwat [19], 2011 Egypt | Prospective | 24 | NS | PLP-S | FOS | N/A | N/A | 2 patients (8.333%) | 3 patients (12.5%) | No | Yes | N/A |
| Taha [17], 2012 United Arab Emirates | Prospective | 60 | US | N/A | FOS | Hip abduction 40–60°, | 3 patients (5%) | No | N/A | No | No | N/A |
| Simeoforidou [20], 2013 Greece | Prospective | 57 | Dual | N/A | FOS | Leg elevation. Lifted upwards and laterally, it could not be adducted to the midline. | 8 patients (14%) | 1 patient (1.75%) | 6 patients (10.5%) | No | Yes, morphine 8.6 ± 5.8 mg | |
| Aissaoui [21], 2013 Morocco | Prospective | 20 | NS | F-PS | F-O-PS | Adductor strength by sphygmomantometer | 0 | No | 5 patients (25%) | No | No | N/A |
| Bareka [22], 2018 Greece | Prospective | 58 | Dual | PLP-S | FOS | Leg elevation. Lifted upwards and laterally, it could not be adducted to the midline. | 5 patient (8.6%) | 1 patient (1.72%) | 11 patients (19.29%) | No | Yes, less morphine consumption than PLP | Patient, refers as good |
| Goyal [23], 2022 India | Prospective | 53 | NS | Spinal | FOS | N/A | N/A | 7 patients (11%) | 2 patients (3%) | No | Yes, less VAS scores and less need for postoperative analgesia | N/A |
| Study ID | LA in FNB | LA in ONB | LA in SNB |
|---|---|---|---|
| Helayel [18], 2007 Brazil | 30 mL ropivacaine 0.5% | 8 mL ropivacaine 0.5% | 15 mL ropivacaine 0.5% |
| Sakura [14], 2010 Japan | 15 mL ropivacaine 0.5% | 5 + 5 mL ropivacaine 0.5% | 20 mL mepivacaine 1.5% + epinephrine 1:400,000 |
| Tharwat [19], 2011 Egypt | 20–30 mL bupivacaine 0.25% + lidocaine 1% | 20–30 mL bupivacaine 0.25% + lidocaine 1% | 20–30 mL bupivacaine 0.25% + lidocaine 1% |
| Taha [17], 2012 United Arab Emirates | 10 mL ropivacaine 0.33% + 0.67% lidocaine + epinephrine | 15 mL ropivacaine 0.33% + 0.67% lidocaine + epinephrine | 20 mL ropivacaine 0.33% + 0.67% lidocaine + epinephrine |
| Simeoforidou [20], 2013 Greece | 25 mL ropivacaine 0.5% | 10 mL ropivacaine 0.5% | 10 mL ropivacaine 0.5% |
| Aissaoui [21], 2013 Morocco | 15 mL bupivacaine 0.25% + lidocaine 1% | 6 mL bupivacaine 0.25% + lidocaine 1% | 25 mL bupivacaine 0.25% + lidocaine 1% |
| Bareka [22], 2018 Greece | 25 mL ropivacaine 0.5% | 10 mL ropivacaine 0.5% | 10 mL ropivacaine 0.5% |
| Goyal [23], 2022 India | 15 mL ropivacaine 0.25% + lidocaine 1% + epinephrine | 8–10 mL ropivacaine 0.25% + lidocaine 1% + epinephrine | 15–20 mL ropivacaine 0.25% + lidocaine 1% + epinephrine |
3.5. Complications
3.6. Postoperative Pain Control
3.7. Patient Satisfaction
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frobell, R.B.; Lohmander, L.S.; Roos, H.P. Acute rotational trauma to the knee: Poor agreement between clinical assessment and magnetic resonance imaging findings. Scand. J. Med. Sci. Sport. 2007, 17, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Parkkari, J.; Pasanen, K.; Mattila, V.M.; Kannus, P.; Rimpela, A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: A population- based cohort study of 46,500 people with a 9 year follow-up. Br. J. Sport. Med. 2008, 42, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, S.M.; Marshall, S.W.; Hume, P.A.; Bunt, L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J. Sci. Med. Sport 2009, 12, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Nordenvall, R.; Bahmanyar, S.; Adami, J.; Stenros, C.; Wredmark, T.; Fellander-Tsai, L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: Incidence, treatment, and sex differences. Am. J. Sport. Med. 2012, 40, 1808–1813. [Google Scholar] [CrossRef] [PubMed]
- Jansson, H.; Narvy, S.J.; Mehran, N. Perioperative pain management strategies for anterior Cruciate ligament reconstruction. JBJS Rev. 2018, 6, e3. [Google Scholar] [CrossRef] [PubMed]
- Mall, N.A.; Chalmers, P.N.; Moric, M.; Tanaka, M.J.; Cole, B.J.; Bach, B.R.; Paletta, G.A. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am. J. Sport. Med. 2014, 42, 2363–2370. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.L.; Kremers, H.M.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am. J. Sport. Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef]
- Herzog, M.M.; Marshall, S.W.; Lund, J.L.; Pate, V.; Mack, C.D.; Spang, J.T. Trends in Incidence of ACL Reconstruction and Concomitant Procedures among Commercially Insured Individuals in the United States, 2002–2014. Sport. Health 2018, 10, 523–531. [Google Scholar] [CrossRef]
- Chunduri, A.; Aggarwal, A.K. Multimodal Pain Management in Orthopedic Surgery. J. Clin. Med. 2022, 11, 6386. [Google Scholar] [CrossRef]
- Andrés-Cano, P.; Godino, M.; Vides, M.; Guerado, E. Postoperative complications of anterior cruciate ligament reconstruction after ambulatory surgery. Rev. Española Cirugía Ortopédica Traumatol. 2015, 59, 157–164. [Google Scholar] [CrossRef]
- Baverel, L.; Cucurulo, T.; Lutz, C.; Colombet; Cournapeau, J.; Dalmay, F.; Lefevre, N.; Letartre, R.; Potel, J.F.; Roussignol, X.; et al. Anesthesia and analgesia methods for outpatient anterior cruciate ligament reconstruction. Orthop. Traumatol. Surg. Res. 2016, 102, s251–s255. [Google Scholar] [CrossRef]
- McNamee, D.A.; Parks, L.; Milligan, K.R. Post-operative analgesia following total knee replacement: An evaluation of the addition of an obturator nerve block to combined femoral and sciatic nerve block. Acta Anaesthesiol. Scand. 2002, 46, 95–99. [Google Scholar] [CrossRef]
- Macalouet, D.; Trueck, S.; Meuret, P.; Heck, M.; Vial, F.; Ouologuem, S.; Capdevila, X.; Virion, J.M.; Bouaziz, H. Postoperative analgesia after total knee replacement: The effect of an obturator nerve block added to the femoral 3-in-1 nerve block. Anesth. Analg. 2004, 99, 251–254. [Google Scholar] [CrossRef]
- Sakura, S.; Hara, K.; Ota, J.; Tadenuma, S. Ultrasound-guided peripheral nerve blocks for anterior cruciate ligament reconstruction: Effect of obturator nerve block during and after surgery. J. Anesth. 2010, 24, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Anagnostopoulou, S.; Kostopanagiotou, G.; Paraskeuopoulos, T.; Chantzi, C.; Lolis, E.; Saranteas, T. Anatomic variations of the obturator nerve in the inguinal region: Implications in conventional and ultrasound regional anesthesia techniques. Reg. Anesth. Pain Med. 2009, 34, 33–39. [Google Scholar] [CrossRef]
- Bendtsen, T.F.; Moriggl, B.; Chan, V.; Borglum, J. The optimal analgesic block for total knee arthroplasty. Reg. Anesth. Pain Med. 2016, 41, 711–7199. [Google Scholar] [CrossRef]
- Taha, A.M. Ultrasound-guided obturator nerve block: A proximal interfascial technique. Anesth. Analg. 2012, 114, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Helayel, P.E.; da Conceição, D.B.; Pavei, P.; Knaesel, J.A.; de Oliveira Filho, G.R. Ultrasound-guided obturator nerve block: A preliminary report of a case series. Reg. Anesth. Pain Med. 2007, 32, 221–226. [Google Scholar] [CrossRef]
- Tharwat, A.I. Combined posterior lumbar plexus-sciatic nerve block versus combined femoral-obturator-sciatic nerve block for ACL reconstruction. Local Reg. Anesth. 2011, 4, 1–6. [Google Scholar] [CrossRef][Green Version]
- Aissaoui, Y.; Serghini, I.; Qamous, Y.; Seddiki, R.; Zoubir, M.; Boughalem, M. The parasacral sciatic nerve block does not induce anesthesia of the obturator nerve. J. Anesth. 2013, 27, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Simeoforidou, M.; Bareka, M.; Basdekis, G.; Tsiaka, K.; Chantzi, E.; Vretzakis, G. Peripheral nerve blockade as an exclusive approach to obturator nerve block in anterior cruciate ligament reconstructive surgery. Korean J. Anesthesiol. 2013, 65, 410–417. [Google Scholar] [CrossRef]
- Bareka, M.; Hantes, M.; Arnaoutoglou, E.; Vretzakis, G. Superior perioperative analgesia with combined femoral–obturator–sciatic nerve block in comparison with posterior lumbar plexus and sciatic nerve block for ACL reconstructive surgery. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 478–484. [Google Scholar] [CrossRef]
- Goyal, T.; Paul, S.; Choudhury, A.K.; Das, L.; Schuh, A.; Govil, N. Combined femoral-obturator-sciatic nerve block has superior postoperative pain score and earlier ambulation as compared to spinal anaesthesia for arthroscopic anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3480–3487. [Google Scholar] [CrossRef]
- Murthy, V.H. Ending the opioid epidemic—A call to action. N. Engl. J. Med. 2016, 375, 2413–2415. [Google Scholar] [CrossRef]
- Teulieres, M.; Berard, E.; Marot, V.; Reina, N.; Ferre, F.; Minville, V.; Cavaignac, E. A quadruple peripheral nerve block outside the OR for anterior cruciate ligament reconstruction reduces the OR occupancy time. Knee Surg. Sport. Traumatol. Arthrosc. 2023, 31, 2917–2926. [Google Scholar] [CrossRef] [PubMed]
- Kuvadia, M.; Cummis, C.E.; Liguori, G.; Wu, C.L. “Green-gional” anesthesia: The non-pulluting benefits of regional anesthesia to decrease greenhouse gases and attenuate climate change. Reg. Anesth. Pain Med. 2020, 45, 744–745. [Google Scholar] [CrossRef] [PubMed]
- Sinha, S.K.; Abrams, J.H.; Houle, T.T.; Weller, R.S. Ultrasound-guided obturator nerve block an interfascial injection approach without nerve stimulation. Reg. Anesth. Pain Med. 2009, 34, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Soong, J.; Schafhalter-Zoppoth, I.; Gray, A.T. Sonographic Imaging of the Obturator Nerve for Regional Block. Reg. Anesth. Pain Med. 2007, 32, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, Y.; Sato, Y.; Kitayama, M.; Shibata, Y.; Komatsu, T.; Hirota, K. Obturator nerve block using ultrasound guidance. Anesth. Analg. 2007, 105, 888–889. [Google Scholar] [CrossRef] [PubMed]
- Akkaya, T.; Ozturk, E.; Comert, A.; Ates, Y.; Gumus, H.; Ozturk, H.; Tekdemir, I.; Elhan, A. Ultrasound-guided obturator nerve block: A sonoanatomic study of a new methodologic approach. Anesth. Analg. 2009, 108, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Onishi, T.; Furutani, K.; Baba, H. A new ultrasound-guided pubic approach for proximal obturator nerve block: Clinical study and cadaver evaluation. Anaesthesia 2016, 71, 291–297. [Google Scholar] [CrossRef][Green Version]
- Lin, J.A.; Nakamoto, T.; Yeh, S.D. Ultrasound standard for obturator nerve block: The modified Taha’s approach. Br. J. Anaesth. 2015, 114, 337–338. [Google Scholar] [CrossRef] [PubMed]
- Wassef, M.R. Interadductor approach to obturator nerve blockade for spastic con-ditions of adductor thigh muscles. Reg. Anesth. 1993, 18, 13–17. [Google Scholar]
- Lang, S.A.; Yip, R.W.; Chang, P.C.; Gerard, M.A. The femoral 3-in-1 block revisited. J. Clin. Anesth. 1993, 5, 292–296. [Google Scholar] [CrossRef]
- Tran, D.Q.; Salinas, F.V.; Benzon, H.T.; Neal, J.M. Lower extremity regional anesthesia: Essentials of our current understanding. Reg. Anesth. Pain Med. 2019, 44, 143–180. [Google Scholar] [CrossRef]
- Auroy, Y.; Benhamou, D.; Bargues, L.; Ecoffey, C.; Falissard, B.; Mercier, F.; Bouaziz, H.; Samii, K. Major complications of regional anesthesia in France the SOS regional anesthesia hotline service. Anesthesiology 2002, 97, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, B.D.; Szűcs, S. Peripheral nerve block and local anaesthetic dose, how much is enough? Anaesthesia 2014, 69, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Nestor, C.C.; Ng, C.; Sepulveda, P.; Irwin, M.G. Pharmacological and clinical implications of local anaesthetic mixtures: A narrative review. Anaesthesia 2022, 77, 339–350. [Google Scholar] [CrossRef]
- Barry, G.S.; Bailey, J.G.; Sardinha, J.; Brousseau, P.; Uppal, V. Factors associated with rebound pain after peripheral nerve block for ambulatory surgery. Br. J. Anaesth. 2021, 126, 862–871. [Google Scholar] [CrossRef]
- Dada, O.; Gonzalez Zacarias, A.; Ongaigui, C.; Echeverria-Villalobos, M.; Kushelev, M.; Bergese, S.D.; Moran, K. Does Rebound Pain after Peripheral Nerve Block for Orthopedic Surgery Impact Postoperative Analgesia and Opioid Consumption? A Narrative Review. Int. J. Environ. Res. Public Health 2019, 16, 3257. [Google Scholar] [CrossRef]
- Stone, A.; Lirk, P.; Vlassakov, K. Rebound Pain after Peripheral Nerve Blockade-Bad Timing or Rude Awakening? Anesthesiol. Clin. 2022, 40, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, Y.; Sakura, S.; Abe, S.; Uchimura, E.; Saito, Y. Effects of the addition of dexamethasone on postoperative analgesia after anterior cruciate ligament reconstruction surgery under quadruple nerve blocks. BMC Anesthesiol. 2021, 21, 218. [Google Scholar] [CrossRef] [PubMed]
| Frame | P (Patients, participants, population) | I (Intervention) | C (Comparator/reference test) | O (Outcome) | Study design | Time | |
| Adult patients undergoing arthroscopic ACL reconstruction under PNBs as the sole anesthetic technique | The performance of 3 separate PBNs: (i) the femoral (F); (ii) the obturator (O); (iii) the sciatic (S); abbreviated as the FOS intervention | Not specified | The effectiveness and the adequacy of performing three separate PBNs (femoral, obturator, sciatic; FOS) as an exclusive method for anesthesia in patients undergoing ACL reconstruction | English language | Search period: 1964–October 2023 | Last search: (October 2023) | |
| Inclusion criteria | Cases, case series, observational or interventional studies (randomized or quasi-randomized clinical trials) | ||||||
| Exclusion criteria | Reviews, narrative or systematic, meta-analyses, and qualitative research | ||||||
| Sources | Databases (Medline, Embase, Cochrane, Web of Science, Google Scholar, and medRxiv) Reference list | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bareka, M.; Ntalouka, M.P.; Angelis, F.; Mermiri, M.; Tsiaka, A.; Hantes, M.; Arnaoutoglou, E. Femoral–Obturator–Sciatic (FOS) Nerve Block as an Anesthetic Triad for Arthroscopic ACL Reconstruction: Is This the Magic Trick We Were Missing? J. Clin. Med. 2024, 13, 1054. https://doi.org/10.3390/jcm13041054
Bareka M, Ntalouka MP, Angelis F, Mermiri M, Tsiaka A, Hantes M, Arnaoutoglou E. Femoral–Obturator–Sciatic (FOS) Nerve Block as an Anesthetic Triad for Arthroscopic ACL Reconstruction: Is This the Magic Trick We Were Missing? Journal of Clinical Medicine. 2024; 13(4):1054. https://doi.org/10.3390/jcm13041054
Chicago/Turabian StyleBareka, Metaxia, Maria P. Ntalouka, Fragkiskos Angelis, Maria Mermiri, Aikaterini Tsiaka, Michael Hantes, and Eleni Arnaoutoglou. 2024. "Femoral–Obturator–Sciatic (FOS) Nerve Block as an Anesthetic Triad for Arthroscopic ACL Reconstruction: Is This the Magic Trick We Were Missing?" Journal of Clinical Medicine 13, no. 4: 1054. https://doi.org/10.3390/jcm13041054
APA StyleBareka, M., Ntalouka, M. P., Angelis, F., Mermiri, M., Tsiaka, A., Hantes, M., & Arnaoutoglou, E. (2024). Femoral–Obturator–Sciatic (FOS) Nerve Block as an Anesthetic Triad for Arthroscopic ACL Reconstruction: Is This the Magic Trick We Were Missing? Journal of Clinical Medicine, 13(4), 1054. https://doi.org/10.3390/jcm13041054







