Inpatient Outcomes of Patients Undergoing Robot-Assisted versus Laparoscopic Radical Cystectomy for Bladder Cancer: A National Inpatient Sample Database Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Ethics Statement
2.3. Study Population
2.4. Outcomes
2.5. Covariates
2.6. Statistical Analysis
3. Results
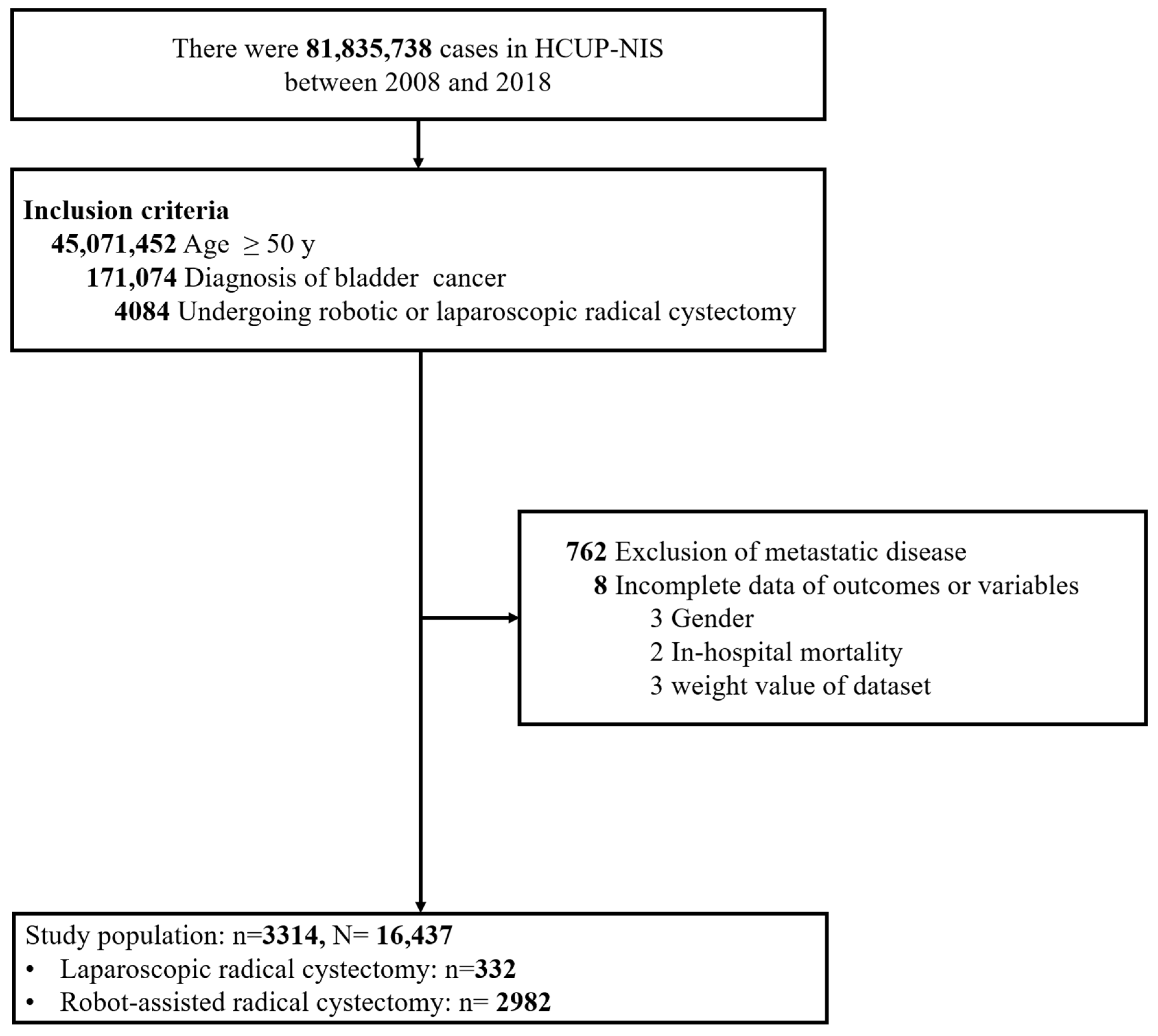
3.1. Study Population Selection
3.2. Characteristics of the Study Population
3.3. Risk of in-Hospital Mortality and Prolonged LOS between Robot-Assisted versus Pure Laparoscopic Cystectomy
3.4. Postoperative Complications of Robot-Assisted vs. Pure Laparoscopic Cystectomy
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dobruch, J.; Oszczudłowski, M. Bladder Cancer: Current Challenges and Future Directions. Medicina 2021, 57, 749. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F.; Bsc, M.F.B.; Me, J.F.; Soerjomataram, M.I.; et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of bladder cancer. Med. Sci. 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Moschini, M.; Simone, G.; Stenzl, A.; Gill, I.S.; Catto, J. Critical review of outcomes from radical cystectomy: Can complications from radical cystectomy be reduced by surgical volume and robotic surgery? Eur. Urol. Focus 2016, 2, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Novara, G.; De Marco, V.; Aragona, M.; Boscolo-Berto, R.; Cavalleri, S.; Artibani, W.; Ficarra, V. Complications and mortality after radical cystectomy for bladder transitional cell cancer. J. Urol. 2009, 182, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.S.; Khetrapal, P.; Tan, W.P.; Rodney, S.; Chau, M.; Kelly, J.D. Robotic assisted radical cystectomy with extracorporeal urinary diversion does not show a benefit over open radical cystectomy: A systematic review and meta-analysis of randomised controlled trials. PLoS ONE 2016, 11, e0166221. [Google Scholar] [CrossRef] [PubMed]
- Ishii, H.; Rai, B.P.; Stolzenburg, J.U.; Bose, P.; Chlosta, P.L.; Somani, B.K.; Nabi, G.; Qazi, H.A.R.; Rajbabu, K.; Kynaston, H.; et al. Robotic or open radical cystectomy, which is safer? A systematic review and meta-analysis of comparative studies. J. Endourol. 2014, 28, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Mastroianni, R.; Ferriero, M.; Tuderti, G.; Anceschi, U.; Bove, A.M.; Brassetti, A.; Misuraca, L.; Zampa, A.; Torregiani, G.; Ghiani, E.; et al. Open radical cystectomy versus robot-assisted radical cystectomy with intracorporeal urinary diversion: Early outcomes of a single-center randomized controlled trial. J. Urol. 2022, 207, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Lisiński, J.; Kienitz, J.; Tousty, P.; Kaczmarek, K.; Lemiński, A.; Słojewski, M. Comparison of laparoscopic and open radical cystectomy for muscle-invasive bladder cancer. Int. J. Environ. Res. Public Health 2022, 19, 15995. [Google Scholar] [PubMed]
- Huang, H.; Yan, B.; Hao, H.; Shang, M.; He, Q.; Liu, L.; Xi, Z. Laparoscopic versus open radical cystectomy in 607 patients with bladder cancer: Comparative survival analysis. Int. J. Urol. 2021, 28, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Tang, K.; Li, H.; Xia, D.; Hu, Z.; Zhuang, Q.; Liu, J.; Xu, H.; Ye, Z. Laparoscopic versus open radical cystectomy in bladder cancer: A systematic review and meta-analysis of comparative studies. PLoS ONE 2014, 9, e95667. [Google Scholar] [CrossRef] [PubMed]
- HCUP-US NIS Overview. 2019. Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp (accessed on 9 November 2023).
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Yang, L.; Deng, Y.Q.; Yan, S.Y.; Gu, J.M.; Li, B.H.; Zi, H.; Ming, D.; Zeng, X.; Wang, Y. The causal association between smoking, alcohol consumption and risk of bladder cancer: A univariable and multivariable Mendelian randomization study. Int. J. Cancer 2022, 151, 2136–2143. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, Y.; Lian, C. Cigarette smoking and risk of bladder cancer: A dose-response meta-analysis. Int. Urol. Nephrol. 2022, 54, 1169–1185. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, J.; Thurairaja, R.; Nair, R. Bladder Cancer. Surgery 2019, 37, 529–537. [Google Scholar] [CrossRef]
- Mori, K.; Mostafaei, H.; Abufaraj, M.; Yang, L.; Egawa, S.; Shariat, S.F. Smoking and bladder cancer: Review of recent literature. Curr. Opin. Urol. 2020, 30, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wei, Z.; Bie, M.; Peng, X.; Chen, C. Robot-assisted versus laparoscopic-assisted surgery for colorectal cancer: A meta-analysis. Surg. Endosc. 2016, 30, 5601–5614. [Google Scholar] [CrossRef]
- Hayn, M.H.; Hellenthal, N.J.; Seixas-Mikelus, S.A.; Mansour, A.M.; Stegemann, A.; Hussain, A.; Guru, K.A. Is patient outcome compromised during the initial experience with robot-assisted radical cystectomy? Results of 164 consecutive cases. BRJ Int. 2011, 108, 882–887. [Google Scholar] [CrossRef]
- Challacombe, B.J.; Bochner, B.H.; Dasgupta, P.; Gill, I.; Guru, K.; Herr, H.; Mottrie, A.; Pruthi, R.; Redorta, J.P.; Wiklund, P. The role of laparoscopic and robotic cystectomy in the management of muscle-invasive bladder cancer with special emphasis on cancer control and complications. Eur. Urol. 2011, 60, 767–775. [Google Scholar] [CrossRef]
- Von Deimling, M.; Furrer, M.; Mertens, L.S.; Mari, A.; van Ginkel, N.; Bacchiani, M.; Maas, M.; Pichler, R.; Li, R.; Moschini, M.; et al. Impact of the extent of lymph node dissection on survival outcomes in clinically lymph node-positive bladder cancer. In BJU International; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2023. [Google Scholar]
- Bada, M.; De Concilio, B.; Crocetto, F.; Creta, M.; Silvestri, T.; Di Mauro, M.; Celia, A. Laparoscopic radical cystectomy with extracorporeal urinary diversion: An Italian single-center experience with 10-year outcomes. Minerva Urol. Nefrol. 2020, 72, 641–643. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total | Laparoscopic Radical Cystectomy | Robot-Assisted Radical Cystectomy | p-Value |
|---|---|---|---|---|
| (n = 3314) | (n = 332) | (n = 2982) | ||
| In-hospital mortality | 54 (1.6) | 11 (3.3) | 43 (1.4) | 0.004 |
| Prolonged LOS a,b | 855 (26.2) | 105 (32.7) | 750 (25.5) | 0.004 |
| Complication (any) | 834 (25.0) | 84 (25.1) | 750 (25.0) | 0.955 |
| Bleeding | 598 (17.9) | 53 (15.9) | 545 (18.1) | 0.279 |
| Pneumonia | 65 (1.9) | 12 (3.6) | 53 (1.8) | 0.009 |
| Infection | 240 (7.2) | 29 (8.5) | 211 (7.1) | 0.315 |
| Wound complications | 122 (3.7) | 23 (6.8) | 99 (3.3) | <0.001 |
| Sepsis | 217 (6.6) | 39 (11.7) | 178 (6.0) | <0.001 |
| Age | 69.5 ± 0.2 | 70.6 ± 0.4 | 69.4 ± 0.2 | 0.023 |
| 50–59 | 485 (14.6) | 43 (12.9) | 442 (14.8) | 0.018 |
| 60–69 | 1146 (34.6) | 96 (28.9) | 1050 (35.2) | |
| 70–79 | 1201 (36.3) | 142 (42.8) | 1059 (35.6) | |
| 80+ | 482 (14.5) | 51 (15.3) | 431 (14.4) | |
| Gender | 0.015 | |||
| Male | 2704 (81.6) | 255 (76.8) | 2449 (82.1) | |
| Female | 610 (18.4) | 77 (23.2) | 533 (17.9) | |
| Race | 0.078 | |||
| White | 2626 (85.9) | 267 (86.4) | 2359 (85.9) | |
| Black | 166 (5.5) | 23 (7.6) | 143 (5.2) | |
| Hispanic | 106 (3.5) | 10 (3.2) | 96 (3.5) | |
| Others | 156 (5.2) | 9 (2.9) | 147 (5.4) | |
| Missing | 260 | 23 | 237 | |
| Household income | 0.018 | |||
| Quartile 1 | 606 (18.5) | 62 (18.6) | 544 (18.5) | |
| Quartile 2 | 870 (26.6) | 104 (31.8) | 766 (26.0) | |
| Quartile 3 | 923 (28.3) | 96 (29.3) | 827 (28.2) | |
| Quartile 4 | 869 (26.6) | 67 (20.3) | 802 (27.3) | |
| Missing | 46 | 3 | 43 | |
| Insurance status | 0.021 | |||
| Medicare/Medicaid | 2238 (67.6) | 246 (74.1) | 1992 (66.8) | |
| Private including HMO | 975 (29.4) | 77 (23.2) | 898 (30.1) | |
| Self-pay/no-charge/other | 101 (3.0) | 9 (2.7) | 92 (3.1) | |
| CCI | 0.017 | |||
| 0–1 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 2–3 | 2355 (71.0) | 223 (67.0) | 2132 (71.5) | |
| 4–5 | 712 (21.5) | 73 (22.1) | 639 (21.4) | |
| 6+ | 247 (7.5) | 36 (10.8) | 211 (7.1) | |
| Hospital bed size | 0.012 | |||
| Large | 2192 (66.1) | 210 (63.2) | 1982 (66.4) | |
| Medium | 673 (20.5) | 88 (26.6) | 585 (19.8) | |
| Small | 447 (13.4) | 34 (10.2) | 413 (13.8) | |
| Missing | 2 | 0 | 2 | |
| Hospital location/teaching status | <0.001 | |||
| Urban teaching | 2901 (87.6) | 274 (82.6) | 2627 (88.2) | |
| Urban nonteaching | 365 (11.0) | 49 (14.9) | 316 (10.6) | |
| Rural | 46 (1.3) | 9 (2.6) | 37 (1.2) | |
| Missing | 2 | 0 | 2 | |
| Year admission | <0.001 | |||
| 2005–2010 | 410 (12.2) | 42 (12.5) | 368 (12.1) | |
| 2011–2014 | 1165 (34.9) | 42 (12.3) | 1123 (37.5) | |
| 2015–2018 | 1739 (52.9) | 248 (75.2) | 1491 (50.4) |
| Outcomes | Robot-Assisted vs. Pure Laparoscopic | |||
|---|---|---|---|---|
| Univariate | Multivariate | |||
| OR (95% CI) | p Value | aOR (95% CI) | p Value | |
| In-hospital mortality | 0.43 (0.23, 0.78) | 0.006 | 0.50 (0.28, 0.90) | 0.020 |
| Prolonged LOS a,b | 0.68 (0.53, 0.86) | 0.001 | 0.63 (0.49, 0.80) | <0.001 |
| Outcomes | Robot-Assisted vs. Pure Laparoscopic | |||
|---|---|---|---|---|
| Univariable | Multivariable | |||
| OR (95% CI) | p Value | aOR (95% CI) | p Value | |
| Complications (any) | 0.99 (0.78, 1.27) | 0.955 | 0.69 (0.54, 0.88) | 0.003 |
| Bleeding | 1.17 (0.88, 1.57) | 0.280 | 0.73 (0.54, 0.99) | 0.045 |
| Pneumonia | 0.48 (0.27, 0.84) | 0.011 | 0.49 (0.28, 0.86) | 0.013 |
| Infection | 0.81 (0.54, 1.22) | 0.316 | 0.55 (0.36, 0.85) | 0.007 |
| Wound complications | 0.47 (0.30, 0.72) | <0.001 | 0.33 (0.20, 0.54) | <0.001 |
| Sepsis | 0.48 (0.34, 0.67) | <0.001 | 0.49 (0.34, 0.69) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, L.-W.; Li, Y.-R.; Wu, C.-M.; Chuang, K.-T.; Li, W.-C.; Liu, C.-Y.; Chang, Y.-H. Inpatient Outcomes of Patients Undergoing Robot-Assisted versus Laparoscopic Radical Cystectomy for Bladder Cancer: A National Inpatient Sample Database Study. J. Clin. Med. 2024, 13, 772. https://doi.org/10.3390/jcm13030772
Fan L-W, Li Y-R, Wu C-M, Chuang K-T, Li W-C, Liu C-Y, Chang Y-H. Inpatient Outcomes of Patients Undergoing Robot-Assisted versus Laparoscopic Radical Cystectomy for Bladder Cancer: A National Inpatient Sample Database Study. Journal of Clinical Medicine. 2024; 13(3):772. https://doi.org/10.3390/jcm13030772
Chicago/Turabian StyleFan, Le-Wei, Yun-Ren Li, Cheng-Mu Wu, Kai-Ti Chuang, Wei-Chang Li, Chung-Yi Liu, and Ying-Hsu Chang. 2024. "Inpatient Outcomes of Patients Undergoing Robot-Assisted versus Laparoscopic Radical Cystectomy for Bladder Cancer: A National Inpatient Sample Database Study" Journal of Clinical Medicine 13, no. 3: 772. https://doi.org/10.3390/jcm13030772
APA StyleFan, L.-W., Li, Y.-R., Wu, C.-M., Chuang, K.-T., Li, W.-C., Liu, C.-Y., & Chang, Y.-H. (2024). Inpatient Outcomes of Patients Undergoing Robot-Assisted versus Laparoscopic Radical Cystectomy for Bladder Cancer: A National Inpatient Sample Database Study. Journal of Clinical Medicine, 13(3), 772. https://doi.org/10.3390/jcm13030772







