Cesarean Uterine Lacerations and Prematurity in the Following Delivery: A Retrospective Longitudinal Follow-Up Cohort Study
Abstract
1. Introduction
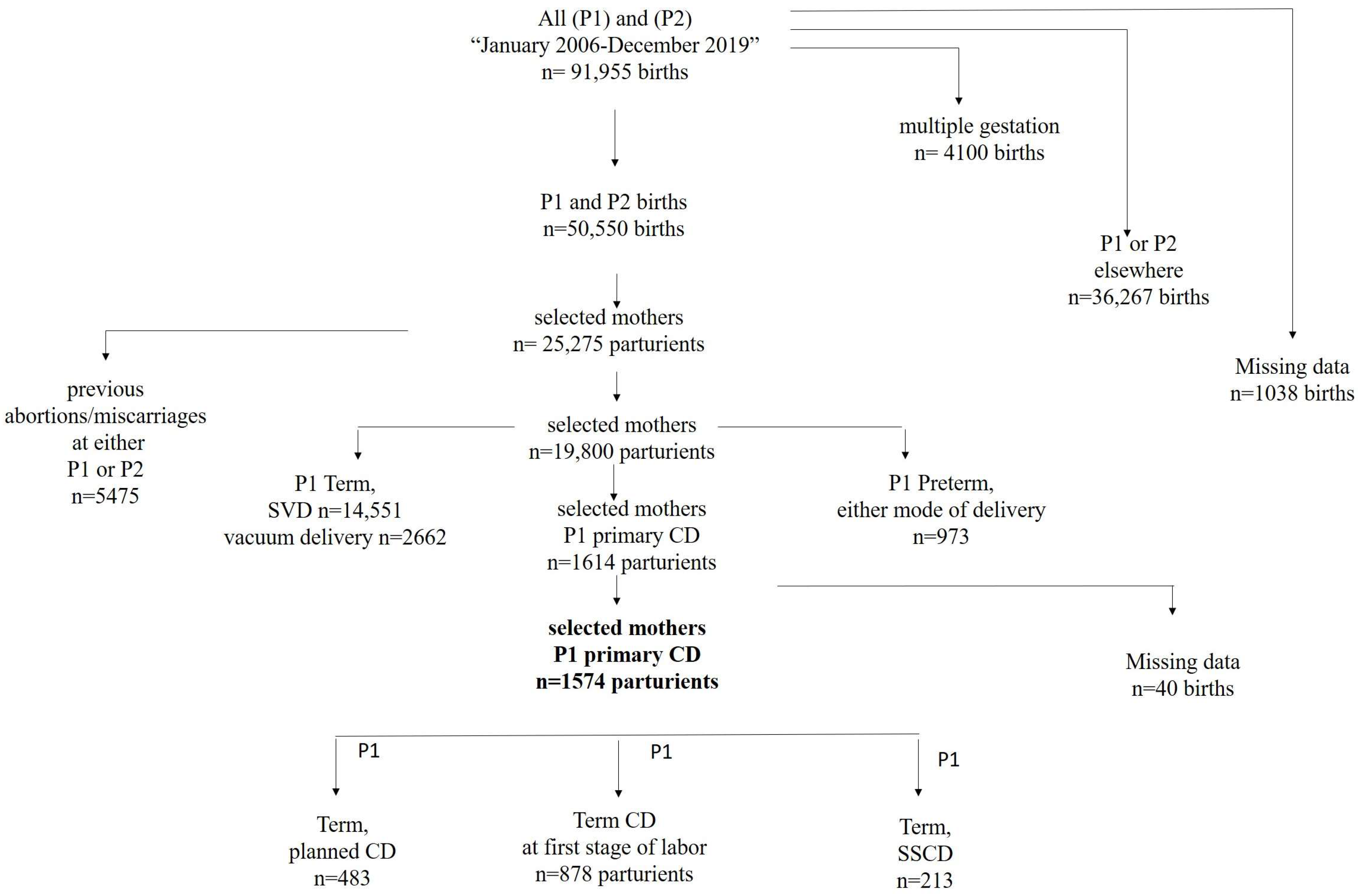
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar] [CrossRef]
- Romero, R.; Espinoza, J.; Kusanovic, J.P.; Gotsch, F.; Hassan, S.; Erez, O.; Chaiworapongsa, T.; Mazor, M. The preterm parturition syndrome. BJOG 2006, 113 (Suppl. S3), 17–42, Erratum in BJOG 2008, 115, 674–675. [Google Scholar] [CrossRef]
- Wood, S.L.; Tang, S.; Crawford, S. Cesarean Delivery in the Second Stage of Labor and the Risk of Subsequent Premature Birth. Am. J. Obstet. Gynecol. 2017, 217, 63.e1–63.e10. [Google Scholar] [CrossRef]
- Levine, L.D.; Sammel, M.D.; Hirshberg, A.; Elovitz, M.A.; Srinivas, S.K. Does stage of labor at time of cesarean delivery affect risk of subsequent preterm birth? Am. J. Obstet. Gynecol. 2015, 212, 360.e1–360.e7. [Google Scholar] [CrossRef]
- Watson, H.A.; Carter, J.; David, A.L.; Seed, P.T.; Shennan, A.H. Full dilation cesarean section: A risk factor for recurrent second-trimester loss and preterm birth. Acta Obstet. Gynecol. Scand. 2017, 96, 1100–1105. [Google Scholar] [CrossRef]
- Visser, L.; Slaager, C.; Kazemier, B.; Rietveld, A.; Oudijk, M.; de Groot, C.; Mol, B.; de Boer, M. Risk of preterm birth after prior term cesarean. BJOG 2020, 127, 610–617. [Google Scholar] [CrossRef]
- Cong, A.; de Vries, B.; Ludlow, J. Does previous caesarean section at full dilatation increase the likelihood of subsequent spontaneous preterm birth? Aust. N. Z. J. Obstet. Gynaecol. 2018, 58, 267–273. [Google Scholar] [CrossRef]
- Berghella, V.; Gimovsky, A.C.; Levine, L.D.; Vink, J. Cesarean in the Second Stage: A Possible Risk Factor for Subsequent Spontaneous Preterm Birth. Am. J. Obstet. Gynecol. 2017, 217, 1–3. [Google Scholar] [CrossRef]
- Alexander, J.M.; Leveno, K.J.; Rouse, D.J.; Landon, M.B.; Gilbert, S.; Spong, C.Y.; Varner, M.W.; Moawad, A.H.; Caritis, S.N.; Harper, M.; et al. Comparison of Maternal and infant outcomes from primary cesarean delivery during the second compared with first stage of labor. Obstet. Gynecol. 2007, 109, 917–921. [Google Scholar] [CrossRef]
- Glazewska-Hallin, A.; Story, L.; Suff, N.; Shennan, A. Late-stage Cesarean section causes recurrent early preterm birth: How to tackle this problem? Ultrasound Obstet. Gynecol. 2019, 54, 293–296. [Google Scholar] [CrossRef]
- Helman, S.; Mahajna, M.; Ehrlich, Z.; Ratner, M.; Grisaru-Granovsky, S.; Reichman, O. Risk of Preterm Birth among Secundiparas with a Previous Cesarean due to a Failed Vacuum Delivery. J. Clin. Med. 2023, 12, 7358. [Google Scholar] [CrossRef] [PubMed]
- Reichman, O.; Gal, M.; Nezer, M.; Shen, O.; Calderon-Margalit, R.; Farkash, R.; Samueloff, A. Delivering Elsewhere between the First and Second Deliveries Is a Risk Marker for Obstetric Complications in the Second Delivery. Arch. Gynecol. Obstet. 2016, 294, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.J.; Liebling, R.E.; Verity, L.; Swingler, R.; Patel, R. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: A cohort study. Lancet 2001, 358, 1203–1207. [Google Scholar] [CrossRef]
- Lurie, S.; Raz, N.; Boaz, M.; Sadan, O.; Golan, A. Comparison of maternal outcomes from primary cesarean section during the second compared with first stage of labor by indication for the operation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 182, 43–47. [Google Scholar] [CrossRef]
- Ewington, L.J.; Quenby, S. Full Dilatation Caesarean Section and the Risk of Preterm Delivery in a Subsequent Pregnancy: A Historical Cohort Study. J. Clin. Med. 2020, 9, 3998. [Google Scholar] [CrossRef]
- Vink, J.Y.; Qin, S.; Brock, C.O.; Zork, N.M.; Feltovich, H.M.; Chen, X.; Urie, P.; Myers, K.M.; Hall, T.J.; Wapner, R.; et al. A new paradigm for the role of smooth muscle cells in the human cervix. Am. J. Obstet. Gynecol. 2016, 215, 478.e1–478.e11. [Google Scholar] [CrossRef]
- Williams, C.; Fong, R.; Murray, S.M.; Stock, S.J. Caesarean birth and risk of subsequent preterm birth: A retrospective cohort study. BJOG 2021, 128, 1020–1028. [Google Scholar] [CrossRef]
- Offringa, Y.; Paret, L.; Vayssiere, C.; Parant, O.; Loussert, L.; Guerby, P. Second stage cesarean section and the risk of preterm birth in subsequent pregnancies. Int. J. Gynaecol. Obstet. 2022, 159, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.D.; Srinivas, S.K. Length of second stage of labor and preterm birth in a subsequent pregnancy. Am. J. Obstet. Gynecol. 2016, 214, 535.e1–535.e4. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Kirby, A.; Gibbs, E.; Gidaszewski, B.; Khajehei, M.; Chua, S.C. Risk of preterm birth in the subsequent pregnancy following caesarean section at full cervical dilatation compared with mid-cavity instrumental delivery. Aust. N. Z. J. Obstet. Gynaecol. 2020, 60, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.Z.; Ho, N.; Tanaka, K.; Lehner, C.; Sekar, R.; Amoako, A.A. Does the length of second stage of labour or second stage caesarean section in nulliparous women increase the risk of preterm birth in subsequent pregnancies? J. Perinat. Med. 2020, 49, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Cornthwaite, K.; Bahl, R.; Winter, C.; Wright, A.; Kingdom, J.; Walker, K.F.; Tydeman, G.; Briley, A.; Schmidt-Hansen, M.; Draycott, T.; et al. Management of Impacted Fetal Head at Caesarean Birth: Scientific Impact Paper No. 73. BJOG 2023, 130, e40–e64. [Google Scholar] [CrossRef] [PubMed]
| P1 Term Planned CD N = 483 | P1 Term First-Stage CD N = 878 | P1 Term SSCD N = 213 | p-Value | ||
|---|---|---|---|---|---|
| P1 first delivery | |||||
| P1 maternal age, years, mean ± std | 26.4 ± 5.4 | 25.8 ± 4.6 | 25.8 ± 4.6 | 0.002 | |
| P1 macrosomia (>4000 g), N | 46 (9.5%) | 47 (5.4%) | 23 (10.9%) | 0.002 | |
| P1 female gender | 249 (51.6%) | 372 (42.2%) | 79 (37.1%) | <0.001 | |
| P1 Apgar at 5 min ≤ 7 | 6 (1.2%) | 27 (3.1%) | 5 (2.3%) | 0.108 | |
| P1 NICU | 13 (2.7%) | 7 (4.4%) | 18 (8.5%) | 0.004 | |
| P1 unintended uterine extension | 5 (1.0%) | 56 (6.4%) | 50 (23.5%) | <0.001 | |
| P2 second delivery | |||||
| Onset of labor | Spontaneous | 265 (54.9%) | 521 (59.3%) | 156 (73.2%) | |
| Induction | 30 (6.2%) | 76 (8.7%) | 9 (4.2%) | <0.001 | |
| CD—no trial of labor | 188 (38.9%) | 281(32.0%) | 48 (22.5%) | ||
| Mode of delivery | Spontaneous | 189 (39.1%) | 319 (36.3%) | 84 (39.4%) | |
| Vacuum extraction | 39 (8.1%) | 99 (11.3%) | 37 (17.4%) | 0.009 | |
| CD | 255 (52.8%) | 458 (52.2%) | 92 (43.2%) | ||
| Preterm birth prior to 37 weeks of gestation | 28 (5.7%) | 36 (4.1%) | 10 (4.7%) | 0.367 | |
| OR (95% CI) | p | |
|---|---|---|
| Factors at P1 | ||
| SSCD versus planned CD | 0.800 (0.383; 1.679) | 0.556 |
| Low-segment uterine incisional extension | 1.402 (0.628; 3.132) | 0.409 |
| Duration of the second stage | 1.000 (0.997; 1.004) | 0.815 |
| Breech presentation | 1.048 (0.608; 1.807) | 0.865 |
| Duration of cesarean operation | 1.000 (0.996; 1.004) | 0.862 |
| Birthweight of newborn | 1.000 (0.999; 1.000) | 0.061 |
| Blood transfusion | 2.493 (0.735; 8.453) | 0.143 |
| Factors at P2 | ||
| Maternal age | 1.066 (1.023; 1.110) | 0.002 |
| Interpregnancy interval of less than one year | 0.846 (0.492; 1.456) | 0.546 |
| Timing of CD at First Delivery (P1) | Status of Extensions in CD at P1 | Preterm Delivery P2 | p-Value |
|---|---|---|---|
| Planned CD | No extension (n = 478) | 28 (5.9%) | 0.741 |
| With extension (n = 5) | 0 | ||
| First-stage CD | No extension (n = 822) | 33 (4%) | 0.407 |
| With extension (n = 56) | 3 (5.4%) | ||
| SSCD | No extension (n = 163) | 6 (3.7%) | 0.185 |
| With extension (n = 50) | 4 (8%) |
| P2 Preterm Birth | p-Value | |||||
|---|---|---|---|---|---|---|
| ≤31.6 Weeks n = 6 | 32–34 Weeks n = 13 | 35–36 Weeks n = 55 | ≥37.0 Weeks n = 1500 | |||
| P1 cesarean delivery n (%) | Incisional extensions 111 (7%) | 2 (1.8%) | 2 (1.8%) | 3 (2.7%) | 104 (93.7%) | 0.047 |
| No extensions 1463 (93%) | 4 (0.3%) | 11 (0.8%) | 52 (3.6%) | 1396 (95.4%) | ||
| P1 Term Planned CD N = 483 | P1 Term First-Stage CD N= 878 | P1 Term SSCD N = 213 | P1 Term Total N = 1574 | p-Value | |
|---|---|---|---|---|---|
| Fetal distress * | 40 (8.3%) | 385 (43.8%) | 54 (25.4%) | 479 (30.4%) | <0.001 |
| Intrapartum fever/chorioamnionitis | 2 (0.4%) | 63 (7.2%) | 16 (7.5%) | 81 (5.1%) | <0.001 |
| Malformed uterus | 20 (4.1%) | 23 (2.6%) | 0 | 43 (2.7%) | 0.008 |
| Gestational hypertension ** | 4 (0.8%) | 43 (4.9%) | 7 (3.3%) | 54 (3.4%) | <0.001 |
| Failed vacuum | 0 | 0 | 58 (27.2%) | 58 (3.7%) | <0.001 |
| Arrest of dilatation | 1 (0.2%) | 85 (9.7%) | 8 (3.8%) | 94 (6%) | <0.001 |
| Premature rupture of membranes | 45 (9.5%) | 154 (17.6%) | 28 (13.3%) | 227 (14.6%) | <0.001 |
| Breech presentation | 198 (41.8%) | 51 (5.8%) | 2 (1%) | 251 (16.1%) | <0.001 |
| No Extension n = 1463 | Low-Segment Uterine Incision Extensions n = 111 | p-Value | |
|---|---|---|---|
| Fetal distress * | 435 (29.7%) | 44 (39.6%) | 0.020 |
| Intrapartum fever/chorioamnionitis | 65 (4.4%) | 16 (14.4%) | <0.001 |
| Malformed uterus | 40 (2.7%) | 3 (2.7%) | 0.640 |
| Pregnancy-induced hypertension ** | 50 (3.4%) | 4 (3.6%) | 0.537 |
| Failed vacuum | 45 (3.1%) | 13 (11.7%) | <0.001 |
| Arrest of dilatation | 88 (6.1%) | 6 (5.5%) | 0.498 |
| Premature rupture of membranes | 211 (14.6%) | 16 (4.5%) | 0.563 |
| Breech presentation | 246 (17.0%) | 5 (4.5%) | <0.001 |
| Reference First Author [# Ref] | SSCD Number | SSCD Low-Segment Uterine Incisional Extensions n (%) | Association between SSCD and PTB (OR) | PTB Subsequent to Uterine Incisional Extensions (OR/Prevalence) |
|---|---|---|---|---|
| Wood, S.L., et al. [3] | 8607 | - | 1.57 (1.43; 1.73) * | - |
| Levine, L.D., et al. [4] | 37 | - | 2.40 (0.77–7.43) * | 13.5% # |
| 5.80 (1.08–30.80) ** | ||||
| Watson, H.A., et al. [5] | 29 | - | 3.06 (1.22–7.71) * | - |
| Cong, A., et al. [7] | 533 | - | 1.50 (0.97–2.20) ** | - |
| Helman, S., et al. [11] | 221 | - | 3.8% vs. 3.4% * | - |
| Murphy, D.J., et al. [14] | 209 | 50 (24%) | ||
| Lurie, S., et al. [15] | 76 | 13 (17.1%) | - | |
| Ewington, L.J., et al. [16] | 329 | 55 (16.8%) ^^ | 1.86 (0.91–3.83) ** | 1.34 (0.54–3.29) |
| Williams, C., et al. [18] | 483 | - | 3.29 (2.02–5.13) * | - |
| Offringa, Y., et al. [19] | 143 | - | 2.50 (1.30–4.90) * | - |
| Levine, L.D., et al. [20] | 37 | not documented | 2.08 (0.32–13.78) * | 20.0% ^ |
| Reichman, O., et al. [Current study] | 213 | 50 (23.5%) | 0.800 (0.38; 1.68) *** | 1.402 (0.628; 3.132) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reichman, O.; Hirsch, A.; Fridman, S.; Grisaru-Granovsky, S.; Helman, S. Cesarean Uterine Lacerations and Prematurity in the Following Delivery: A Retrospective Longitudinal Follow-Up Cohort Study. J. Clin. Med. 2024, 13, 749. https://doi.org/10.3390/jcm13030749
Reichman O, Hirsch A, Fridman S, Grisaru-Granovsky S, Helman S. Cesarean Uterine Lacerations and Prematurity in the Following Delivery: A Retrospective Longitudinal Follow-Up Cohort Study. Journal of Clinical Medicine. 2024; 13(3):749. https://doi.org/10.3390/jcm13030749
Chicago/Turabian StyleReichman, Orna, Ayala Hirsch, Shira Fridman, Sorina Grisaru-Granovsky, and Sarit Helman. 2024. "Cesarean Uterine Lacerations and Prematurity in the Following Delivery: A Retrospective Longitudinal Follow-Up Cohort Study" Journal of Clinical Medicine 13, no. 3: 749. https://doi.org/10.3390/jcm13030749
APA StyleReichman, O., Hirsch, A., Fridman, S., Grisaru-Granovsky, S., & Helman, S. (2024). Cesarean Uterine Lacerations and Prematurity in the Following Delivery: A Retrospective Longitudinal Follow-Up Cohort Study. Journal of Clinical Medicine, 13(3), 749. https://doi.org/10.3390/jcm13030749







