The Prevalence and Diagnostic Patterns of Oral and Maxillofacial Lesions: A Seven-Year, Retrospective, Single-Center Cone Beam Computed Tomography and Histopathology Study in Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethical Approval and Patient Confidentiality
2.3. Inclusion and Exclusion Criteria
2.4. Diagnostic Imaging and Pathological Confirmation
2.5. Reliability Assessment
2.6. Data Extraction
2.7. Statistical Analysis
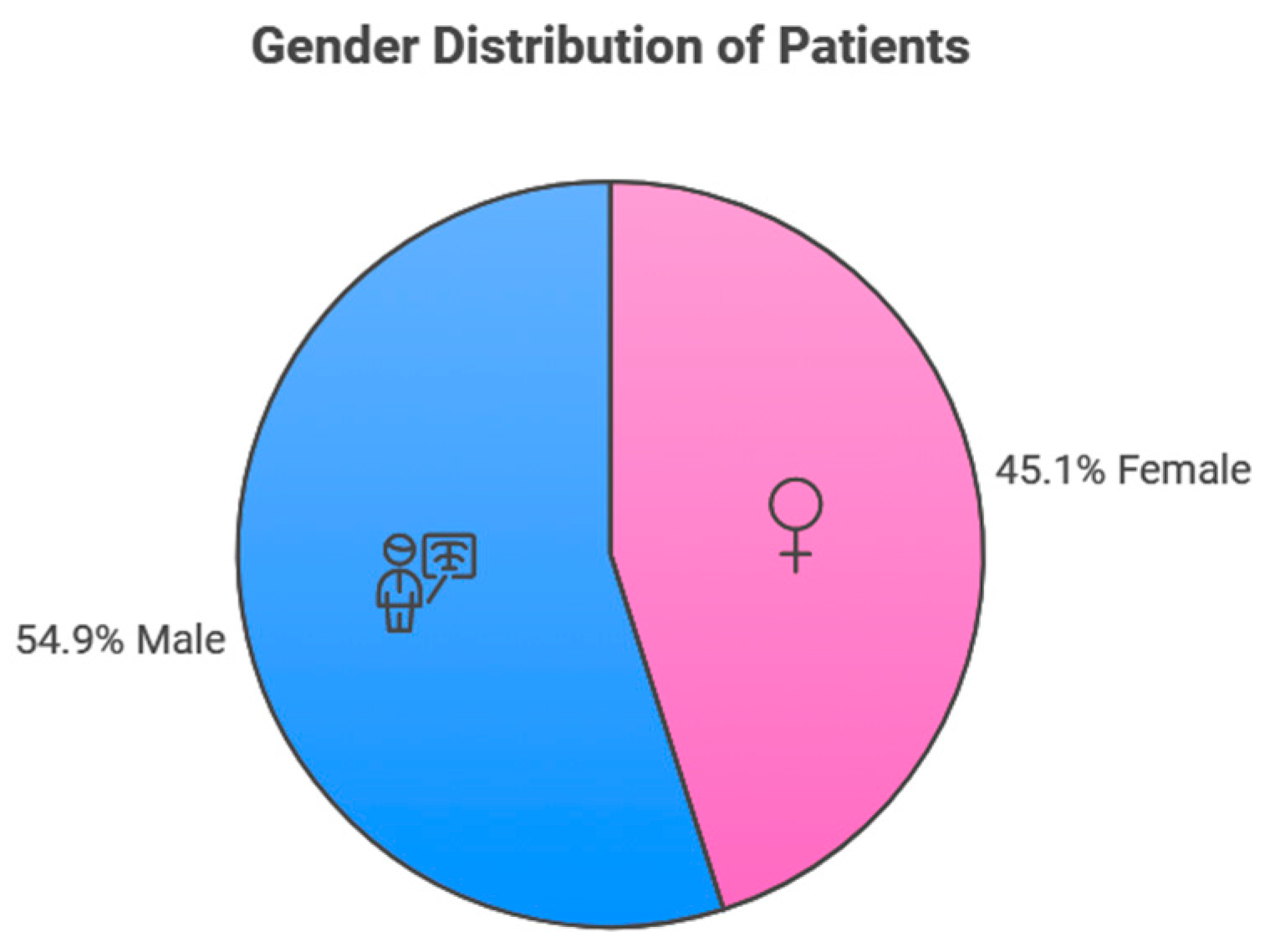
3. Results
3.1. Participants’ Lesion Sites
3.2. Benign and Malignant Odontogenic Tumors
3.3. Odontogenic Cysts
3.4. Other Lesions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lauritano, D.; Moreo, G.; Carinci, F.; Borgia, R.; Lucchese, A.; Contaldo, M.; Della Vella, F.; Bernardelli, P.; Moreo, G.; Petruzzi, M. Aging and oral care: An observational study of characteristics and prevalence of oral diseases in an Italian cohort. Int. J. Environ. Res. Public Health 2019, 16, 3763. [Google Scholar] [CrossRef] [PubMed]
- Shahzad, A.; Kiyani, A.; Paiker, S. Prevalence of oral anomalies and pathologies in the Pakistani population—A cross sectional study. J. Pakistan Dent. Assoc. 2018, 27, 13–17. [Google Scholar] [CrossRef]
- Monteiro, L.S.; Albuquerque, R.; Paiva, A.; de la Peña-Moral, J.; Amaral, J.B.; Lopes, C.A. A comparative analysis of oral and maxillofacial pathology over a 16-year period, in the north of Portugal. Int. Dent. J. 2017, 67, 38–45. [Google Scholar] [CrossRef]
- Shabir, H.; Irshad, M.; Durrani, S.H.; Sarfaraz, A.; Arbab, K.N.; Khattak, M.T. First comprehensive report on distribution of histologically confirmed oral and maxillofacial pathologies; A nine-year retrospective study. J. Pak. Med. Assoc. 2022, 72, 685–690. [Google Scholar] [CrossRef]
- Singh, H.P.; Thippeswamy, S.H.; Gandhi, P.; Salgotra, V.; Choudhary, S.; Agarwal, R. A retrospective study to evaluate biopsies of oral and maxillofacial lesions. J. Pharm. Bioallied Sci. 2021, 13, S116–S119. [Google Scholar] [CrossRef]
- Oivio, U.-M.; Pesonen, P.; Ylipalosaari, M.; Kullaa, A.; Salo, T. Prevalence of oral mucosal normal variations and lesions in a middle-aged population: A Northern Finland Birth Cohort 1966 study. BMC Oral Health 2020, 20, 357. [Google Scholar] [CrossRef] [PubMed]
- Izgi, E.; Mollaoglu, N.; Simsek, M.B. Prevalence of odontogenic cysts and tumors on Turkish sample according to latest classification of World Health Organization: A 10-year retrospective study. Niger. J. Clin. Pract. 2021, 24, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Ruslin, M.; van Trikt, K.N.; Yusuf, A.-S.-H.; Tajrin, A.; Fauzi, A.; Rasul, M.-I.; Boffano, P.; Forouzanfar, T. Epidemiology, treatment, and recurrence of odontogenic and non-odontogenic cysts in South Sulawesi, Indonesia: A 6-year retrospective study. J. Clin. Exp. Dent. 2022, 14, e247–e253. [Google Scholar] [CrossRef] [PubMed]
- Hewlett, S.A.; Blankson, P.K.; Aheto, J.M.K.; Anto, F.; Danso-Appiah, T.; Sackeyfio, J.; Koram, K.; Amoah, A.G.B. Assessment of oral health status in a Ghanaian population: Rationale, methods, and population characteristics. BMC Oral Health 2022, 22, 67. [Google Scholar] [CrossRef] [PubMed]
- Mao, W.-Y.; Lei, J.; Lim, L.Z.; Gao, Y.; Tyndall, D.A.; Fu, K. Comparison of radiographical characteristics and diagnostic accuracy of intraosseous jaw lesions on panoramic radiographs and CBCT. Dentomaxillofac. Radiol. 2021, 50, 20200165. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Zhou, Z.; Shen, X.; Wang, Y.; Shi, L.; Wang, Y.; Hu, Y.; Sun, H.; Liu, W. Prevalence and distribution of oral mucosal lesions: A cross-sectional study in Shanghai, China. J. Oral Pathol. Med. 2015, 44, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Amadori, F.; Bardellini, E.; Conti, G.; Majorana, A. Oral mucosal lesions in teenagers: A cross-sectional study. Ital. J. Pediatr. 2017, 43, 50. [Google Scholar] [CrossRef]
- Kaur, H.; Gosavi, S.; Hazarey, V.K.; Gupta, V.; Bhadauria, U.S.; Kherde, P. Impact of changing classification systems on prevalence and frequency distribution of odontogenic tumors in tertiary care center of Nagpur. Braz. J. Otorhinolaryngol. 2022, 88, S3–S13. [Google Scholar] [CrossRef]
- Sudarsan, R.; Abilasha, R. Prevalence of odontogenic tumours in association with age and gender—An institutional study. J. Popul. Ther. 2020, 29, e222–e231. [Google Scholar] [CrossRef]
- Speight, P.M.; Takata, T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: Odontogenic and maxillofacial bone tumours. Virchows Arch. 2018, 472, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Slootweg, P.J.; El-Naggar, A.K. World Health Organization 4th edition of head and neck tumor classification: Insight into the consequential modifications. Virchows Arch. 2018, 472, 311–313. [Google Scholar] [CrossRef]
- Villasis-Sarmiento, L.; Portilla-Robertson, J.; Melendez-Ocampo, A.; Gaitan-Cepeda, L.-A.; Leyva-Huerta, E.-R. Prevalence and distribution of odontogenic cysts in a Mexican sample. A 753 cases study. J. Clin. Exp. Dent. 2017, 9, e531–e538. [Google Scholar] [CrossRef] [PubMed]
- Garg, R.K.; O’Connor, M.K.; Sterling, D.A.; Jacob, L.; Hammoudeh, J.A.; Andrews, B.T. Pediatric odontogenic and maxillofacial bone pathology: A global analysis. J. Craniofac. Surg. 2021, 33, 870–874. [Google Scholar] [CrossRef] [PubMed]
- Goodson, A.M.; Sarwar, M.S.; Rehman, U.; Brennan, P.A. Classifications and Lists in Oral and Maxillofacial Surgery, 1st ed.; CRC Press: Boca Raton, FL, USA, 2024. [Google Scholar] [CrossRef]
- Kebede, B.; Tare, D.; Bogale, B.; Alemseged, F. Odontogenic tumors in Ethiopia: Eight years retrospective study. BMC Oral Health 2017, 17, 54. [Google Scholar] [CrossRef] [PubMed]
- Winters, R.; Garip, M.; Meeus, J.; Coropciuc, R.; Politis, C. Safety and efficacy of adjunctive therapy in the treatment of odontogenic keratocyst: A systematic review. Br. J. Oral Maxillofac. Surg. 2023, 61, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Alhindi, N.A.; Sindi, A.M.; Binmadi, N.O.; Elias, W.Y. A retrospective study of oral and maxillofacial pathology lesions diagnosed at the Faculty of Dentistry, King Abdulaziz University. Clin. Cosmet. Investig. Dent. 2019, 11, 45–52. [Google Scholar] [CrossRef] [PubMed]
- AlSheddi, M.A.; AlSenani, M.A.; Aldosari, A. Odontogenic tumors: Analysis of 188 cases from Saudi Arabia. Ann. Saudi Med. 2015, 35, 146–150. [Google Scholar] [CrossRef]
- Jaeger, F.; de Noronha, M.S.; Silva, M.L.; Amaral, M.B.; Grossmann, S.M.; Horta, M.C.; de Souza, P.E.; de Aguiar, M.C.; Mesquita, R.A. Prevalence profile of odontogenic cysts and tumors on Brazilian sample after the reclassification of odontogenic keratocyst. J. Craniomaxillofac. Surg. 2017, 45, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Kambalimath, D.H.; Kambalimath, H.V.; Agrawal, S.M.; Singh, M.; Jain, N.; Anurag, B.; Michael, P. Prevalence and distribution of odontogenic cyst in Indian population: A 10 year retrospective study. J. Maxillofac. Oral Surg. 2014, 13, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Del Corso, G.; Righi, A.; Bombardi, M.; Rossi, B.; Dallera, V.; Pelliccioni, G.A.; Marchetti, C.; Foschini, M.P. Jaw cysts diagnosed in an Italian population over a 20-year period. Int. J. Surg. Pathol. 2014, 22, 699–706. [Google Scholar] [CrossRef]
- Ismail, S.; Saw, C.L. A clinicopathologic study of 173 odontogenic tumours in Northern Peninsular Malaysia (2007–2014). Malays. J. Pathol. 2018, 40, 129–135. [Google Scholar] [PubMed]
- Tamiolakis, P.; Thermos, G.; Tosios, K.I.; Sklavounou-Andrikopoulou, A. Demographic and clinical characteristics of 5294 jaw cysts: A retrospective study of 38 years. Head Neck Pathol. 2019, 13, 587–596. [Google Scholar] [CrossRef]
- Al Sheddi, M.A. Odontogenic cysts. A clinicopathological study. Saudi Med. J. 2012, 33, 304–308. [Google Scholar] [PubMed]
- Güler, N.; Şençift, K.; Demirkol, Ö. Conservative management of keratocystic odontogenic tumors of jaws. Sci. World J. 2012, 2012, 680397. [Google Scholar] [CrossRef]
- Jeong, Y.; Kang, B.-H.; Park, M.-J.; Choi, S.-J.; Park, H.-J.; Oh, H.K.; Kook, M. A retrospective study of cysts in the maxillofacial area. Oral Biol. Res. 2019, 43, 210–216. [Google Scholar] [CrossRef]
- Anwer, T.; Charan, D.D.; Batra, D.N.; Bajoria, D.A.A.; Ritu, D.P. Evaluation of prevalence of odontogenic tumours and cysts at maxillofacial area. Webology 2022, 19, 3163–3169. Available online: https://api.semanticscholar.org/CorpusID:251244574 (accessed on 31 October 2024).
- Almazyad, A.; Alamro, M.; Almadan, N.; Almutairi, M.; Alquwayz, T.S. Frequency and demographic analysis of odontogenic tumors in three tertiary institutions: An 11-year retrospective study. Diagnostics 2024, 14, 910. [Google Scholar] [CrossRef]
- Alshehri, B.M. Trends in the incidence of oral cancer in Saudi Arabia from 1994 to 2015. World J. Surg. Oncol. 2020, 18, 217. [Google Scholar] [CrossRef] [PubMed]
- Saleh, S.M.; Idris, A.M.; Vani, N.V.; Tubaigy, F.M.; Alharbi, F.A.; Sharwani, A.A.; Mikhail, N.T.; Warnakulasuriya, S. Retrospective analysis of biopsied oral and maxillofacial lesions in South-Western Saudi Arabia. Saudi Med. J. 2017, 38, 405–412. [Google Scholar] [CrossRef]
- Kumararama, S.S.; Patel, S.D.; Parekh, N.H.; Bhate, P.; Kukreja, B.J.; Hazra, T.; Kumar, A.; Badiyani, B.K. Investigate how frequently dental professionals conduct oral cancer screenings during routine dental check-ups and the methods they use. J. Pharm. Bioallied Sci. 2014, 16, S783–S785. [Google Scholar] [CrossRef]
- Silva, L.P.; Leite, R.B.; Sobral, A.P.V.; Arruda, J.A.; Oliveira, L.V.; Noronha, M.S.; Kato, C.O.; Mesquita, R.A.; Schuch, L.F.; Gomes, A.P.N.; et al. Oral and maxillofacial lesions diagnosed in older people of a Brazilian population: A multicentric study. J. Am. Geriatr. Soc. 2017, 65, 1586–1590. [Google Scholar] [CrossRef] [PubMed]
- Shetty, P.; Prince, J.; Poojary, D.; Poorna, P.; Suresh, P.K. Diagnostic conundrum in an ambiguous posterior mandibular osseous lesion: Case report and radiological review. Int. J. Surg. Case Rep. 2023, 106, 108288. [Google Scholar] [CrossRef]
- Pick, E.; Schäfer, T.; Husain, A.A.H.; Rupp, N.J.; Hingsammer, L.; Valdec, S. Clinical, radiological, and pathological diagnosis of fibro-osseous lesions of the oral and maxillofacial region: A retrospective study. Diagnostics 2022, 12, 238. [Google Scholar] [CrossRef]
- Mohammad, D.N.; Ibraheem, B.F.; Garib, B.T.; Hamied, M.A.S. Histopathological records of oral and maxillofacial lesions among pediatric and adolescent patients in Sulaimani Governorate. Children 2022, 9, 156. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Clear CBCT and a histopathologically confirmed diagnosis | Diagnosed outside KAUFD (n = 38, 17.75%) |
| Male or female | CBCT was conducted for another purpose (n = 132, 61.68%) |
| Age > 18 years | No CBCT reading and radiographic report (n = 16, 7.47) No histopathology results (n = 8, 3.73%) Treatment completed outside KAUFD (n = 20, 9.34%) |
| WHO Classification of Head and Neck Tumors: Odontogenic and Maxillofacial Bone Tumors. | ||
|---|---|---|
| Benign Odontogenic Tumors | ||
Epithelial odontogenic tumors
| Mixed epithelial and mesenchymal odontogenic tumors
| Mesenchymal odontogenic tumors
|
| Malignant odontogenic tumors | ||
Odontogenic carcinomas
| Odontogenic carcinosarcoma | Odontogenic sarcoma |
| Odontogenic cysts | ||
Odontogenic cysts of inflammatory origin
| Odontogenic and non-odontogenic developmental cysts
| |
| Lesion Type | Number | Percentage |
|---|---|---|
| Benign odontogenic tumor | 24 | 10.12% |
| Malignant odontogenic tumor | 7 | 2.95% |
| Odontogenic cyst | 155 | 65.40% |
| Other | 51 | 21.51% |
| Total | 237 | 100.00% |
| Lesion Classification | Type | n (%) |
|---|---|---|
| Benign odontogenic tumors | Odontoma | 12 (50%) |
| Ameloblastoma | 8 (33.3%) | |
| Ossifying fibroma | 2 (8.3%) | |
| Cemento-ossifying fibroma | 1 (4.2%) | |
| Odontogenic myxoma | 1 (4.2%) | |
| Malignant odontogenic tumors | Multiple myeloma | 3 (42.9%) |
| Squamous cell carcinoma | 2 (28.8%) | |
| Chondroblastic osteosarcoma | 1 (14.3%) | |
| Spindle cell neoplasm | 1 (14.3%) | |
| Odontogenic cysts | Radicular cyst | 51 (32.9%) |
| Keratocycst | 36 (23.2%) | |
| Odontogenic cyst | 32 (20.6%) | |
| Dentigerous cyst | 17 (11%) | |
| Glandular odontogenic cyst | 6 (3.9%) | |
| Simple bone cyst | 5 (3.2%) | |
| Periapical cyst | 4 (2.5%) | |
| Nasopalatine dust cyst | 3 (1.9%) | |
| Lateral periodontal cyst | 1 (0.6%) | |
| Other lesions | Periapical granuloma | 19 (37.2%) |
| Cemento-osseous dysplasia | 12 (23.5) | |
| Fibrous dysplasia | 6 (11.8%) | |
| Osteomyelitis | 4 (7.8) | |
| Medication-related osteonecrosis of the jaw | 2 (3.9%) | |
| Sialolith | 2 (3.95) | |
| Central giant cell lesion | 1 (2%) | |
| Sialoadenitis | 1 (2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzahrani, S.; Wazzan, T.; Almaghrabi, A.; Alkhudran, A.; Aljereb, H.; Elsayed, S.; Alolayan, A.B. The Prevalence and Diagnostic Patterns of Oral and Maxillofacial Lesions: A Seven-Year, Retrospective, Single-Center Cone Beam Computed Tomography and Histopathology Study in Saudi Arabia. J. Clin. Med. 2024, 13, 7774. https://doi.org/10.3390/jcm13247774
Alzahrani S, Wazzan T, Almaghrabi A, Alkhudran A, Aljereb H, Elsayed S, Alolayan AB. The Prevalence and Diagnostic Patterns of Oral and Maxillofacial Lesions: A Seven-Year, Retrospective, Single-Center Cone Beam Computed Tomography and Histopathology Study in Saudi Arabia. Journal of Clinical Medicine. 2024; 13(24):7774. https://doi.org/10.3390/jcm13247774
Chicago/Turabian StyleAlzahrani, Shadi, Tagreed Wazzan, Abdulaziz Almaghrabi, Abdulaziz Alkhudran, Hamzah Aljereb, Shadia Elsayed, and Albraa B. Alolayan. 2024. "The Prevalence and Diagnostic Patterns of Oral and Maxillofacial Lesions: A Seven-Year, Retrospective, Single-Center Cone Beam Computed Tomography and Histopathology Study in Saudi Arabia" Journal of Clinical Medicine 13, no. 24: 7774. https://doi.org/10.3390/jcm13247774
APA StyleAlzahrani, S., Wazzan, T., Almaghrabi, A., Alkhudran, A., Aljereb, H., Elsayed, S., & Alolayan, A. B. (2024). The Prevalence and Diagnostic Patterns of Oral and Maxillofacial Lesions: A Seven-Year, Retrospective, Single-Center Cone Beam Computed Tomography and Histopathology Study in Saudi Arabia. Journal of Clinical Medicine, 13(24), 7774. https://doi.org/10.3390/jcm13247774







