Postprocedural Contrast-Associated Acute Kidney Injury and Prognosis of Patients Undergoing Recanalization of Chronic Total Occlusions
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patient Population
2.2. Data and Statistical Analyses
3. Results
3.1. Baseline Patient and Lesion Characteristics
3.2. Procedural Characteristics and Outcomes
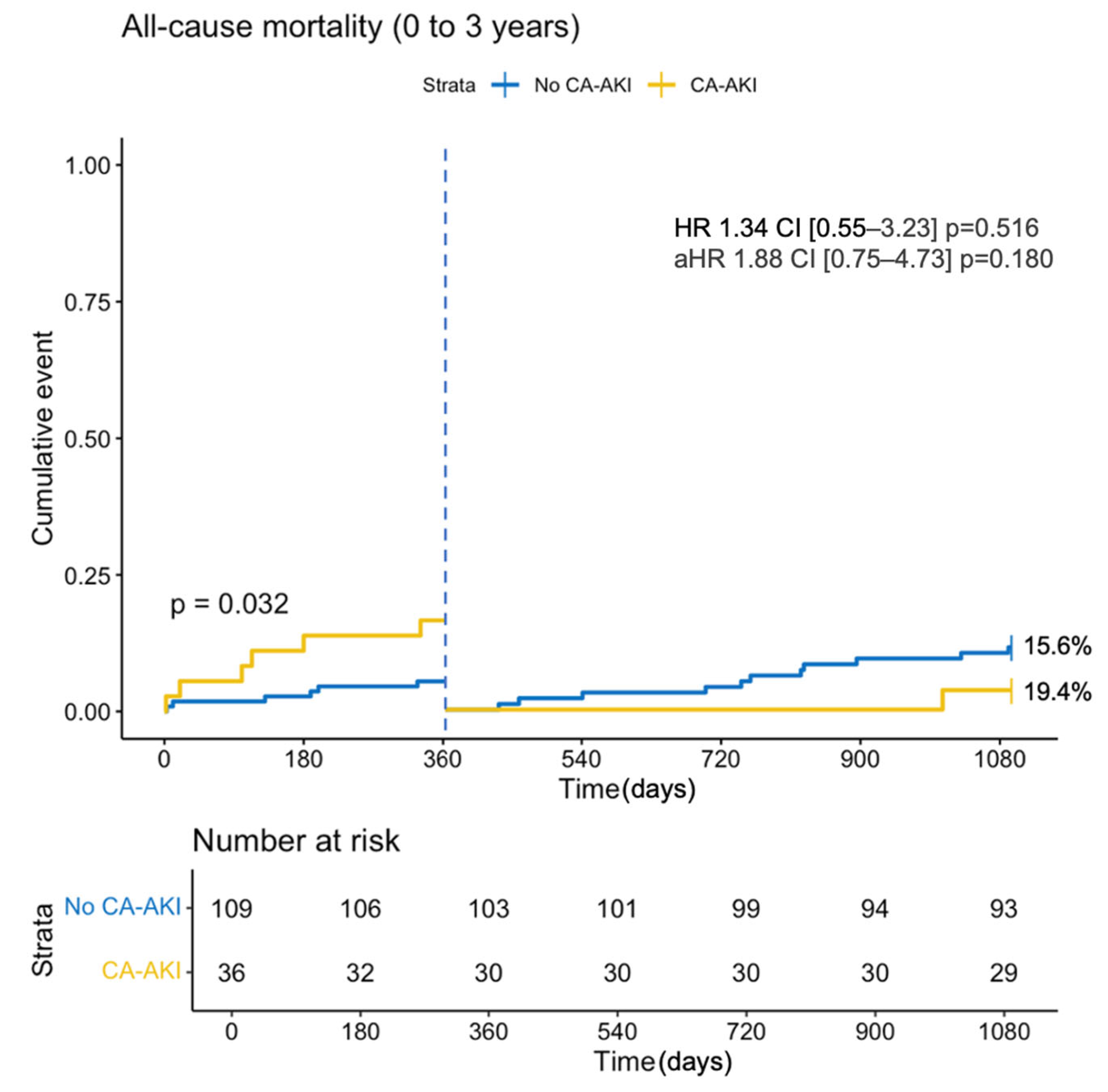
3.3. All-Cause Mortality
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mandurino-Mirizzi, A.; Munafò, A.; Crimi, G. Contrast-Associated Acute Kidney Injury. J. Clin. Med. 2022, 11, 2167. [Google Scholar] [CrossRef] [PubMed]
- Solomon, R.; Dauerman, H.L. Contrast-induced acute kidney injury. Circulation 2010, 122, 2451–2455. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Gurm, H.S.; Bhatt, D.L.; Chew, D.P.; Ellis, S.G. Renal failure after percutaneous coronary intervention is associated with high mortality. Catheter. Cardiovasc. Interv. 2005, 64, 442–448. [Google Scholar] [CrossRef]
- Brilakis, E.S.; Mashayekhi, K.; Tsuchikane, E.; Rafeh, N.A.; Alaswad, K.; Araya, M.; Avran, A.; Azzalini, L.; Babunashvili, A.M.; Bayani, B.; et al. Guiding Principles for Chronic Total Occlusion Percutaneous Coronary Intervention: A Global Expert Consensus Document. Circulation 2019, 140, 420–433. [Google Scholar] [CrossRef] [PubMed]
- Sapontis, J.; Hirai, T.; Patterson, C.; Gans, B.; Yeh, R.W.; Lombardi, W.; Karmpaliotis, D.; Moses, J.; Nicholson, W.J.; Pershad, A.; et al. Intermediate procedural and health status outcomes and the clinical care pathways after chronic total occlusion angioplasty: A report from the OPEN-CTO (outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures) study. Catheter. Cardiovasc. Interv. 2021, 98, 626–635. [Google Scholar] [CrossRef]
- Mehran, R.; Aymong, E.D.; Nikolsky, E.; Lasic, Z.; Iakovou, I.; Fahy, M.; Mintz, G.S.; Lansky, A.J.; Moses, J.W.; Stone, G.W.; et al. simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: Development and initial validation. J. Am. Coll. Cardiol. 2004, 44, 1393–1399. [Google Scholar] [CrossRef]
- Azzalini, L.; Vilca, L.M.; Lombardo, F.; Poletti, E.; Laricchia, A.; Beneduce, A.; Maccagni, D.; Demir, O.M.; Slavich, M.; Giannini, F.; et al. Incidence of contrast-induced acute kidney injury in a large cohort of all-comers undergoing percutaneous coronary intervention: Comparison of five contrast media. Int. J. Cardiol. 2018, 273, 69–73. [Google Scholar] [CrossRef]
- Werner, G.S.; Lorenz, S.; Yaginuma, K.; Koch, M.; Tischer, K.; Werner, J.; Keuser, T.; Moehlis, H.; Riegel, W. A prospective study on the incidence of contrast-associated acute kidney injury after recanalization of chronic total coronary occlusions with contemporary interventional techniques. Int. J. Cardiol. 2021, 337, 38–43. [Google Scholar] [CrossRef]
- Azzalini, L.; Ojeda, S.; Demir, O.M.; Dens, J.; Tanabe, M.; La Manna, A.; Benincasa, S.; Bellini, B.; Poletti, E.; Maccagni, D.; et al. Recanalization of Chronic Total Occlusions in Patients with vs. Without Chronic Kidney Disease: The Impact of Contrast-Induced Acute Kidney Injury. Can. J. Cardiol. 2018, 34, 1275–1282. [Google Scholar] [CrossRef]
- Tajti, P.; Ayoub, M.; Ahres, A.; Rahimi, F.; Behnes, M.; Buettner, H.-J.; Neumann, F.-J.; Westermann, D.; Mashayekhi, K. Procedural outcomes of chronic total occlusion percutaneous coronary interventions in patients with acute kidney injury. Cardiol. J. 2024, 31, 84. [Google Scholar] [CrossRef]
- Lv, Q.; Li, D.; Wang, Y.; Yu, P.; Zhao, L.; Chen, S.; Wang, M.; Fu, G.; Zhang, W. Admission electrolyte and osmotic pressure levels are associated with the incidence of contrast-associated acute kidney injury. Sci. Rep. 2022, 12, 4714. [Google Scholar] [CrossRef] [PubMed]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron. Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Rasouli, M. Basic concepts and practical equations on osmolality: Biochemical approach. Clin. Biochem. 2016, 49, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.T.; Patel, U.D.; Chang, T.I.; Kennedy, K.F.; Masoudi, F.A.; Matheny, M.E.; Kosiborod, M.; Amin, A.P.; Messenger, J.C.; Rumsfeld, J.S.; et al. Contemporary Incidence, Predictors, and Outcomes of Acute Kidney Injury in Patients Undergoing Percutaneous Coronary Interventions: Insights from the NCDR Cath-PCI Registry. JACC Cardiovasc. Interv. 2014, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.A.; Manolis, T.A.; Melita, H.; Mikhailidis, D.P.; Manolis, A.S. Low serum albumin: A neglected predictor in patients with cardiovascular disease. Eur. J. Intern. Med. 2022, 102, 24–39. [Google Scholar] [CrossRef]
- Wang, Y.; Sun, W.J.; Ji, Z.S.; Liu, C.B.; Wang, R. Serum albumin and the risk of contrast-induced acute kidney injury after percutaneous coronary intervention. Rev. Cardiovasc. Med. 2020, 21, 139–145. [Google Scholar] [CrossRef]
- Mankerious, N.; Hemetsberger, R.; Traboulsi, H.; Toelg, R.; Abdel-Wahab, M.; Richardt, G.; Allali, A. Predictors of In-Hospital Adverse Outcomes after Rotational Atherectomy: Impact of the Target Vessel SYNTAX Score. Cardiovasc. Revasc. Med. 2020, 21, 754–759. [Google Scholar] [CrossRef]
- Mankerious, N.; Hemetsberger, R.; Samy, M.; Elbasha, K.; Kandil, N.; Elawady, M.; Toelg, R.; Abdel-Wahab, M.; Richardt, G.; Allali, A. The Target Vessel SYNTAX Score: A Novel Pre-Procedural Predictor for Contrast-Induced Acute Kidney Injury After Rotational Atherectomy. Cardiovasc. Revasc. Med. 2023, 47, 18–24. [Google Scholar] [CrossRef]
- Andreis, A.; Budano, C.; Levis, M.; Garrone, P.; Usmiani, T.; D’ascenzo, F.; De Filippo, O.; D’amico, M.; Bergamasco, L.; Biancone, L.; et al. Contrast-induced kidney injury: How does it affect long-term cardiac mortality? J. Cardiovasc. Med. 2017, 18, 908–915. [Google Scholar] [CrossRef]
- Leoncini, M.; Toso, A.; Maioli, M.; Tropeano, F.; Villani, S.; Bellandi, F. Early high-dose rosuvastatin for contrast-induced nephropathy prevention in acute coronary syndrome: Results from the PRATO-ACS Study (Protective Effect of Rosuvastatin and Antiplatelet Therapy On contrast-induced acute kidney injury and myocardial damage in patients with Acute Coronary Syndrome). J. Am. Coll. Cardiol. 2014, 63, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.F.; Brilakis, E.S.; Wendel, C.S.; Thai, H. Comparison of procedural complications and in-hospital clinical outcomes between patients with successful and failed percutaneous intervention of coronary chronic total occlusions: A Meta-Analysis of Observational Studies. Catheter. Cardiovasc. Interv. 2015, 85, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Megaly, M.; Khalil, M.; Basir, M.B.; McEntegart, M.B.; Spratt, J.C.; Yamane, M.; Tsuchikane, E.; Xu, B.; Alaswad, K.; Brilakis, E.S. Outcomes of successful vs. failed contemporary chronic total occlusion percutaneous coronary intervention. Cardiovasc. Interv. Ther. 2022, 37, 483–489. [Google Scholar] [CrossRef]
- Goel, P.K.; Khanna, R.; Pandey, C.M.; Ashfaq, F. Long-term outcomes post chronic total occlusion intervention—Implications of completeness of revascularization. J. Interv. Cardiol. 2018, 31, 293–301. [Google Scholar] [CrossRef]
- Maioli, M.; Toso, A.; Leoncini, M.; Gallopin, M.; Musilli, N.; Bellandi, F. Persistent renal damage after contrast-induced acute kidney injury: Incidence, evolution, risk factors, and prognosis. Circulation 2012, 125, 3099–3107. [Google Scholar] [CrossRef]
- Hamzaraj, K.; Kammerlander, A.; Gyöngyösi, M.; Frey, B.; Distelmaier, K.; Graf, S. Patient Selection and Clinical Indication for Chronic Total Occlusion Revascularization-A Workflow Focusing on Non-Invasive Cardiac Imaging. Life 2022, 13, 4. [Google Scholar] [CrossRef]
- Canton, L.; Suma, N.; Amicone, S.; Impellizzeri, A.; Bodega, F.; Marinelli, V.; Ciarlantini, M.; Casuso, M.; Bavuso, L.; Belà, R.; et al. Clinical impact of multimodality assessment of myocardial viability. Echocardiography 2024, 41, e15854. [Google Scholar] [CrossRef]

| Total n = 145 | No CA-AKI n = 109 | CA-AKI n = 36 | p Value | |
|---|---|---|---|---|
| Male sex | 109 (75.2%) | 84 (77.1%) | 25 (69.4%) | 0.487 |
| Age (y) | 67.3 (11.5) | 67.3 (11.2) | 67.3 (12.4) | 0.996 |
| BMI | 26.9 [24.7;31.1] | 26.8 [24.5;30.8] | 28.5 [25.2;32.8] | 0.217 |
| Diabetes | 48 (33.1%) | 35 (32.1%) | 13 (36.1%) | 0.812 |
| Dyslipidemia | 107 (73.8%) | 83 (76.1%) | 24 (66.7%) | 0.367 |
| Hypertension | 111 (76.6%) | 85 (78.0%) | 26 (72.2%) | 0.631 |
| Current smoker | 38 (26.2%) | 27 (24.8%) | 11 (30.6%) | 0.641 |
| Prior MI | 62 (42.8%) | 48 (44.0%) | 14 (38.9%) | 0.729 |
| Prior PCI | 81 (55.9%) | 65 (59.6%) | 16 (44.4%) | 0.162 |
| Prior CABG | 20 (13.8%) | 13 (11.9%) | 7 (19.4%) | 0.272 |
| PAD | 31 (21.4%) | 23 (21.1%) | 8 (22.2%) | 1.000 |
| TIA/Stroke | 5 (3.45%) | 4 (3.67%) | 1 (2.78%) | 1.000 |
| History of Heart Failure | 27 (18.6%) | 19 (17.4%) | 8 (22.2%) | 0.694 |
| Chronic pulmonary disease § | 20 (13.8%) | 15 (13.8%) | 5 (13.9%) | 1.000 |
| Chronic kidney disease * | 54 (37.2%) | 38 (34.9%) | 16 (44.4%) | 0.405 |
| Dialysis | 1 (0.93%) | 1 (1.16%) | 0 (0.00%) | 1.000 |
| Baseline creatinine (mg/dL) | 1.04 [0.87;1.31] | 1.02 [0.87;1.31] | 1.09 [0.87;1.33] | 0.589 |
| GFR (mL/min/1.73 m2) | 71.0 [53.1;87.6] | 71.5 [55.0;87.5] | 65.6 [50.9;90.9] | 0.640 |
| Fasting glucose | ||||
| 100–125 mg/dL | 59 (40.7%) | 47 (43.1%) | 12 (33.3%) | 0.042 |
| ≥126 mg/dL | 56 (38.6%) | 36 (33.0%) | 20 (55.6%) |
| Total n = 145 | No CA-AKI n = 109 | CA-AKI n = 36 | p Value | |
|---|---|---|---|---|
| Number of diseased vessels | 0.008 | |||
| 1 | 21 (14.5%) | 12 (11.0%) | 9 (25.0%) | |
| 2 | 53 (36.6%) | 47 (43.1%) | 6 (16.7%) | |
| 3 | 71 (49.0%) | 50 (45.9%) | 21 (58.3%) | |
| Multivessel disease | 124 (85.5%) | 97 (89.0%) | 27 (75.0%) | 0.073 |
| CTO vessel | 0.186 | |||
| LAD | 37 (25.5%) | 25 (22.9%) | 12 (33.3%) | |
| CX | 25 (17.2%) | 22 (20.2%) | 3 (8.33%) | |
| RCA | 83 (57.2%) | 62 (56.9%) | 21 (58.3%) | |
| J-CTO score | 2 [1;3] | 2 [1;3] | 2 [1;3] | 0.574 |
| In-stent CTO | 13 (8.97%) | 10 (9.17%) | 3 (8.33%) | 1.000 |
| CTO involving a bifurcation Lesion | 29 (20.0%) | 25 (22.9%) | 4 (11.1%) | 0.194 |
| Calcification (moderate–severe) | 42 (29.0%) | 31 (28.4%) | 11 (30.6%) | 0.976 |
| Length > 20 mm | 91 (62.8%) | 67 (61.5%) | 24 (66.7%) | 0.718 |
| Proximal cap ambiguity | 52 (35.9%) | 42 (38.5%) | 10 (27.8%) | 0.334 |
| Absence of interventional collaterals | 14 (9.66%) | 10 (9.17%) | 4 (11.1%) | 0.749 |
| Moderate–severe tortuosity | 17 (11.7%) | 12 (11.0%) | 5 (13.9%) | 0.765 |
| Circumflex CTO | 28 (19.3%) | 22 (20.2%) | 6 (16.7%) | 0.826 |
| Ostial CTO | 20 (13.8%) | 14 (12.8%) | 6 (16.7%) | 0.582 |
| Aorto-ostial CTO | 5 (3.45%) | 3 (2.75%) | 2 (5.56%) | 0.598 |
| Total n = 145 | No CA-AKI n = 109 | CA-AKI n = 36 | p Value | |
|---|---|---|---|---|
| Use of radial access | 0.183 | |||
| Biradial | 46 (31.7%) | 39 (35.8%) | 7 (19.4%) | |
| Radial and femoral | 29 (20.0%) | 20 (18.3%) | 9 (25.0%) | |
| CTO final strategy | 0.881 | |||
| Antegrade | 120 (82.8%) | 91 (83.5%) | 29 (80.6%) | |
| Retrograde | 25 (17.2%) | 18 (16.5%) | 7 (19.4%) | |
| Rotational atherectomy | 9 (6.21%) | 6 (5.50%) | 3 (8.33%) | 0.690 |
| Number of stents | 2 [1;3] | 2 [1;3] | 2 [1;2] | 0.759 |
| Maximal stent size (mm) | 3.27 (0.56) | 3.24 (0.58) | 3.36 (0.48) | 0.271 |
| Total stent length (mm) | 54.5 [32.2;80.0] | 56.0 [33.0;81.2] | 50.5 [30.5;75.5] | 0.395 |
| Mehran risk score | 11.3 (5.52) | 11.2 (5.42) | 11.6 (5.85) | 0.674 |
| Total procedural time (min) | 170 [135;210] | 165 [127;205] | 180 [153;211] | 0.103 |
| Contrast volume (mL) | 250 [178;330] | 240 [170;330] | 280 [214;338] | 0.173 |
| Total DAP (µGy·m2) | 14,147 [7815;24,528] | 13,326 [7292;22,090] | 22,087 [9313;29,823] | 0.041 |
| Periprocedural hydration | 62 (42.8%) | 47 (43.1%) | 15 (41.7%) | 1.000 |
| Periprocedural catecholamines | 20 (13.8%) | 15 (13.8%) | 5 (13.9%) | 1.000 |
| Fluoroscopy duration (min) | 46.3 [28.0;65.4] | 43.0 [26.1;59.5] | 52.1 [35.6;73.1] | 0.138 |
| Technical success | 115 (79.3%) | 86 (78.9%) | 29 (80.6%) | 1.000 |
| Procedural success | 105 (72.4%) | 80 (73.4%) | 25 (69.4%) | 0.807 |
| In-hospital MACCE | 6 (4.14%) | 3 (2.75%) | 3 (8.33%) | 0.162 |
| Post max creatinine (mg/dL) | 1.16 [0.88;1.63] | 1.02 [0.84;1.30] | 1.73 [1.45;2.45] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamzaraj, K.; Demirel, C.; Gyöngyösi, M.; Bartko, P.E.; Hengstenberg, C.; Frey, B.; Hemetsberger, R. Postprocedural Contrast-Associated Acute Kidney Injury and Prognosis of Patients Undergoing Recanalization of Chronic Total Occlusions. J. Clin. Med. 2024, 13, 7676. https://doi.org/10.3390/jcm13247676
Hamzaraj K, Demirel C, Gyöngyösi M, Bartko PE, Hengstenberg C, Frey B, Hemetsberger R. Postprocedural Contrast-Associated Acute Kidney Injury and Prognosis of Patients Undergoing Recanalization of Chronic Total Occlusions. Journal of Clinical Medicine. 2024; 13(24):7676. https://doi.org/10.3390/jcm13247676
Chicago/Turabian StyleHamzaraj, Kevin, Caglayan Demirel, Mariann Gyöngyösi, Philipp E. Bartko, Christian Hengstenberg, Bernhard Frey, and Rayyan Hemetsberger. 2024. "Postprocedural Contrast-Associated Acute Kidney Injury and Prognosis of Patients Undergoing Recanalization of Chronic Total Occlusions" Journal of Clinical Medicine 13, no. 24: 7676. https://doi.org/10.3390/jcm13247676
APA StyleHamzaraj, K., Demirel, C., Gyöngyösi, M., Bartko, P. E., Hengstenberg, C., Frey, B., & Hemetsberger, R. (2024). Postprocedural Contrast-Associated Acute Kidney Injury and Prognosis of Patients Undergoing Recanalization of Chronic Total Occlusions. Journal of Clinical Medicine, 13(24), 7676. https://doi.org/10.3390/jcm13247676







