Sacubitril/Valsartan and Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Effects on the Arrhythmic Burden
Abstract
1. Introduction
2. Materials and Methods
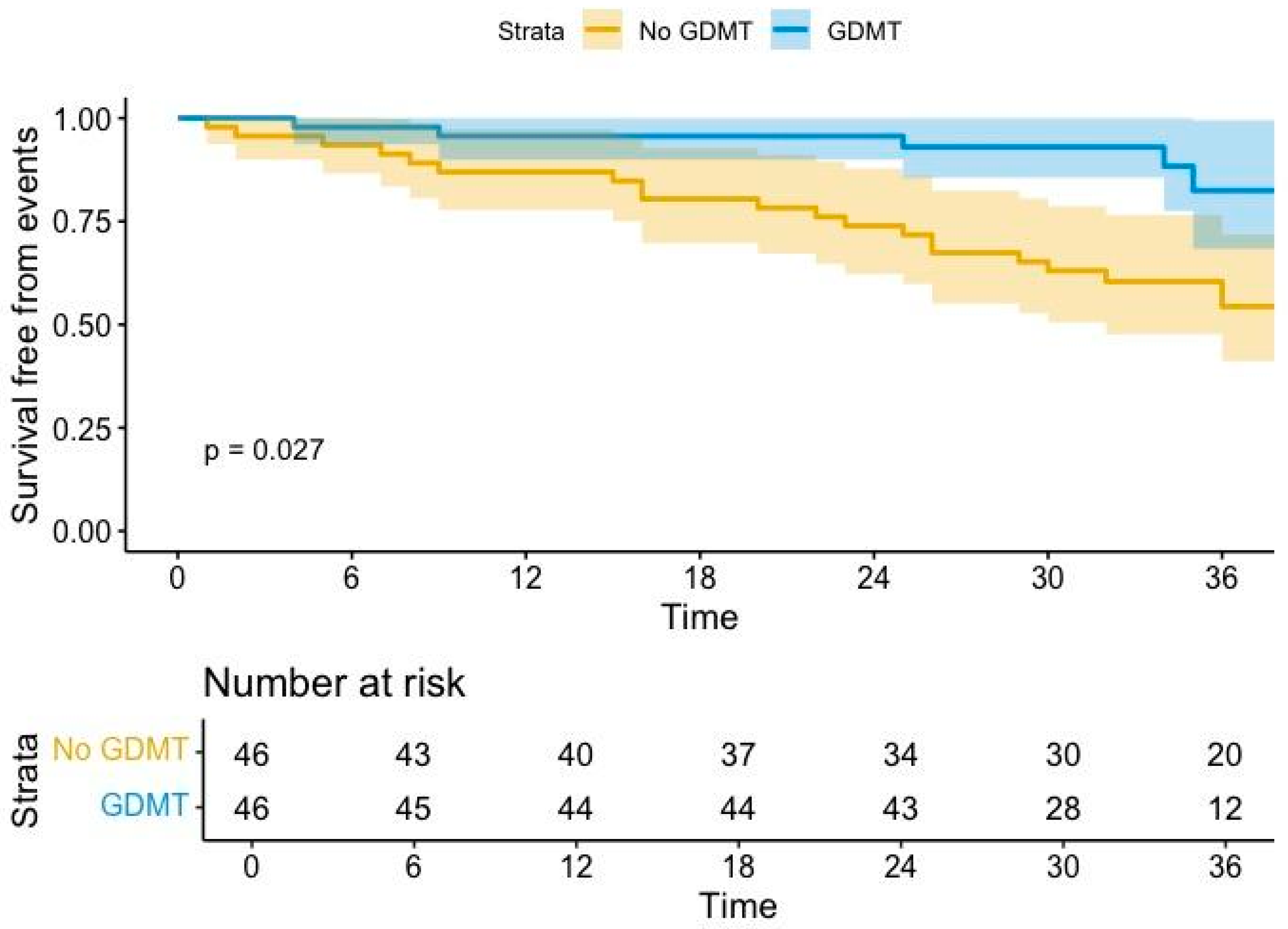
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Broberg, C.S.; van Dissel, A.; Minnier, J.; Aboulhosn, J.; Kauling, R.M.; Ginde, S.; Krieger, E.V.; Rodriguez, F., 3rd; Gupta, T.; Shah, S.; et al. Long-Term Outcomes After Atrial Switch Operation for Transposition of the Great Arteries. J. Am. Coll. Cardiol. 2022, 80, 951–963. [Google Scholar] [CrossRef] [PubMed]
- van Dissel, A.C.; Opotowsky, A.R.; Burchill, L.J.; Aboulhosn, J.; Grewal, J.; Lubert, A.M.; Antonova, P.; Shah, S.; Cotts, T.; John, A.S.; et al. End-stage heart failure in congenitally corrected transposition of the great arteries: A multicentre study. Eur. Heart J. 2023, 44, 3278–3291. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ladouceur, M.; Van De Bruaene, A.; Kauling, R.; Budts, W.; Roos-Hesselink, J.; Albert, S.V.; Perez, I.S.; Sarubbi, B.; Fusco, F.; Gallego, P.; et al. A new score for life-threatening ventricular arrhythmias and sudden cardiac death in adults with transposition of the great arteries and a systemic right ventricle. Eur. Heart J. 2022, 43, 2685–2694. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Scognamiglio, G.; Merola, A.; Iannuzzi, A.; Palma, M.; Grimaldi, N.; Sarubbi, B. Safety and Efficacy of Sacubitril/Valsartan in Patients with a Failing Systemic Right Ventricle: A Prospective Single-Center Study. Circ. Heart Fail. 2023, 16, e009848. [Google Scholar] [CrossRef]
- Fusco, F.; Scognamiglio, G.; Abbate, M.; Merola, A.; Grimaldi, N.; Ciriello, G.D.; Sarubbi, B. Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Results From the DAPA-SERVE Trial. JACC Heart Fail. 2024, 12, 789–791. [Google Scholar] [CrossRef] [PubMed]
- Martens, P.; Nuyens, D.; Rivero-Ayerza, M.; Van Herendael, H.; Vercammen, J.; Ceyssens, W.; Luwel, E.; Dupont, M.; Mullens, W. Sacubitril/valsartan reduces ventricular arrhythmias in parallel with left ventricular reverse remodeling in heart failure with reduced ejection fraction. Clin. Res. Cardiol. 2019, 108, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Benedikt, M.; Oulhaj, A.; Rohrer, U.; Manninger, M.; Tripolt, N.J.; Pferschy, P.N.; Aziz, F.; Wallner, M.; Kolesnik, E.; Gwechenberger, M.; et al. Ertugliflozin to Reduce Arrhythmic Burden in Patients with ICDs/CRT-Ds. NEJM Evid. 2024, 3, EVIDoa2400147. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.; Bernard, M.L.; Elise Hiltbold, A.; Khatib, S.; Polin, G.M.; Rogers, P.A.; Dominic, P.; Morin, D.P. Sacubitril/valsartan: An antiarrhythmic drug? J. Cardiovasc. Electrophysiol. 2022, 33, 2375–2381. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Falguera, D.; Aranyó, J.; Teis, A.; Ferrer-Curriu, G.; Monguió-Tortajada, M.; Fadeuilhe, E.; Rodríguez-Leor, O.; Díaz-Güemes, I.; Roura, S.; Villuendas, R.; et al. Antiarrhythmic and Anti-Inflammatory Effects of Sacubitril/Valsartan on Post-Myocardial Infarction Scar. Circ. Arrhythmia Electrophysiol. 2024, 17, e012517. [Google Scholar] [CrossRef] [PubMed]
- Curtain, J.P.; Jackson, A.M.; Shen, L.; Jhund, P.S.; Docherty, K.F.; Petrie, M.C.; Castagno, D.; Desai, A.S.; Rohde, L.E.; Lefkowitz, M.P.; et al. Effect of sacubitril/valsartan on investigator-reported ventricular arrhythmias in PARADIGM-HF. Eur. J. Heart Fail. 2022, 24, 551–561. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, X.; Liu, H.; Wang, L.; Zhang, L.; Xu, Q. Role of sacubitril-valsartan in the prevention of atrial fibrillation occurrence in patients with heart failure: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2022, 17, e0263131. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frommeyer, G.; Uphoff, J.; Wolfes, J.; Eckardt, L.; Ellermann, C. Dapagliflozin but not empagliflozin prevents atrial fibrillation in an experimental whole-heart model. Eur. Heart J. 2022, 43, ehac544.505. [Google Scholar] [CrossRef]
- Paasche, A.; Wiedmann, F.; Kraft, M.; Seibertz, F.; Herlt, V.; Blochberger, P.L.; Jávorszky, N.; Beck, M.; Weirauch, L.; Seeger, T.; et al. Acute antiarrhythmic effects of SGLT2 inhibitors-dapagliflozin lowers the excitability of atrial cardiomyocytes. Basic Res. Cardiol. 2024, 119, 93–112. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duan, H.Y.; Barajas-Martinez, H.; Antzelevitch, C.; Hu, D. The potential anti-arrhythmic effect of SGLT2 inhibitors. Cardiovasc. Diabetol. 2024, 23, 252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kolesnik, E.; Scherr, D.; Rohrer, U.; Benedikt, M.; Manninger, M.; Sourij, H.; von Lewinski, D. SGLT2 Inhibitors and Their Antiarrhythmic Properties. Int. J. Mol. Sci. 2022, 23, 1678. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zelniker, T.A.; Bonaca, M.P.; Furtado, R.H.M.; Mosenzon, O.; Kuder, J.F.; Murphy, S.A.; Bhatt, D.L.; Leiter, L.A.; McGuire, D.K.; Wilding, J.P.H.; et al. Effect of Dapagliflozin on Atrial Fibrillation in Patients with Type 2 Diabetes Mellitus: Insights From the DECLARE-TIMI 58 Trial. Circulation 2020, 141, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Noh, H.J.; Cha, S.J.; Kim, C.H.; Choi, S.W.; Lee, C.H.; Hwang, J.K. Efficacy of dapagliflozin in improving arrhythmia-related outcomes after ablation for atrial fibrillation: A retrospective single-center study. Clin. Res. Cardiol. 2024; epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mariani, M.V.; Manzi, G.; Pierucci, N.; Laviola, D.; Piro, A.; D’Amato, A.; Filomena, D.; Matteucci, A.; Severino, P.; Miraldi, F.; et al. SGLT2i effect on atrial fibrillation: A network meta-analysis of randomized controlled trials. J. Cardiovasc. Electrophysiol. 2024, 35, 1754–1765. [Google Scholar] [CrossRef] [PubMed]
- Koufakis, T.; Giannakoulas, G.; Zebekakis, P.; Kotsa, K. The effect of dapagliflozin on ventricular arrhythmias, cardiac arrest, or sudden death in people with heart failure: A tick in another box for sodium-glucose cotransporter 2 inhibitors. Expert. OpinPharmacother. 2022, 23, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Curtain, J.P.; Docherty, K.F.; Jhund, P.S.; Petrie, M.C.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; et al. Effect of dapagliflozin on ventricular arrhythmias, resuscitated cardiac arrest, or sudden death in DAPA-HF. Eur. Heart J. 2021, 42, 3727–3738. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fujiki, S.; Iijima, K.; Nakagawa, Y.; Takahashi, K.; Okabe, M.; Kusano, K.; Owada, S.; Kondo, Y.; Tsujita, K.; Shimizu, W.; et al. Effect of empagliflozin on ventricular arrhythmias in patients with type 2 diabetes treated with an implantable cardioverter-defibrillator: The EMPA-ICD trial. Cardiovasc. Diabetol. 2024, 23, 224. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hernández-Madrid, A.; Paul, T.; Abrams, D.; Aziz, P.F.; Blom, N.A.; Chen, J.; Chessa, M.; Combes, N.; Dagres, N.; Diller, G.; et al. Arrhythmias in congenital heart disease: A position paper of the European Heart Rhythm Association (EHRA), Association for European Paediatric and Congenital Cardiology (AEPC), and the European Society of Cardiology (ESC) Working Group on Grown-up Congenital heart disease, endorsed by HRS, PACES, APHRS, and SOLAECE. Europace 2018, 20, 1719–1753. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef] [PubMed]
- Brida, M.; Diller, G.P.; Gatzoulis, M.A. Systemic Right Ventricle in Adults with Congenital Heart Disease: Anatomic and Phenotypic Spectrum and Current Approach to Management. Circulation 2018, 137, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, 1494–1563, Erratum in J. Am. Coll. Cardiol. 2019, 73, 2361. [Google Scholar] [CrossRef] [PubMed]
- Ladouceur, M.; Segura de la Cal, T.; Gaye, B.; Valentin, E.; Ly, R.; Iserin, L.; Legendre, A.; Mousseaux, E.; Li, W.; Rafiq, I.; et al. Effect of medical treatment on heart failure incidence in patients with a systemic right ventricle. Heart 2021, 107, 1384–1389. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Rodriguez-Monserrate, C.P.; Gauvreau, K.; Dellborg, M.; Fusco, F.; Gupta, T.; Kay, J.; Kutty, S.; Kauling, R.M.; Nicolarsen, J.; et al. Propensity Score Analysis of Possible Medication Effects on Outcomes in Patients with Systemic Right Ventricles. JACC Adv. 2025, 4, 101443. [Google Scholar] [CrossRef]
- Kharbanda, R.K.; Moore, J.P.; Lloyd, M.S.; Galotti, R.; Bogers, A.J.J.C.; Taverne, Y.J.H.J.; Madhavan, M.; McLeod, C.J.; Dubin, A.M.; Mah, D.Y.; et al. Cardiac Resynchronization Therapy for Adult Patients with a Failing Systemic Right Ventricle: A Multicenter Study. J. Am. Heart Assoc. 2022, 11, e025121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thompson, S.E.; Hudsmith, L.E.; Bowater, S.E.; Clift, P.; Marshall, H.; Leyva, F.; Arif, S. Cardiac resynchronization therapy in adults with structural congenital heart disease and chronic heart failure. Pacing Clin. Electrophysiol. 2023, 46, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Barracano, R.; Brida, M.; Guarguagli, S.; Palmieri, R.; Diller, G.P.; Gatzoulis, M.A.; Wong, T. Implantable cardiac electronic device therapy for patients with a systemic right ventricle. Heart 2020, 106, 1052–1058. [Google Scholar] [CrossRef] [PubMed]
- Nederend, M.; Kiès, P.; Regeer, M.V.; Vliegen, H.W.; Mertens, B.J.; Robbers-Visser, D.; Bouma, B.J.; Tops, L.F.; Schalij, M.J.; Jongbloed, M.R.M.; et al. Tolerability and beneficial effects of sacubitril/valsartan on systemic right ventricular failure. Heart 2023, 109, 1525–1532. [Google Scholar] [CrossRef] [PubMed]
- Neijenhuis, R.M.L.; Nederend, M.; Jongbloed, M.R.M.; Kiès, P.; Rotmans, J.I.; Vliegen, H.W.; Jukema, J.W.; Egorova, A.D. The potential of sodium-glucose cotransporter 2 inhibitors for the treatment of systemic right ventricular failure in adults with congenital heart disease. Front. Cardiovasc. Med. 2023, 10, 1093201. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Age (Years) | 38.2 ± 10.7 | |
| Sex | 27 (58%) males | |
| d-TGA | 30 (65%) | |
| ccTGA | 16 (35%) | |
| Additional defects | 11 (23%) VSD + PS | |
| 2 (4%) PS | ||
| 3 (6%) VSD | ||
| 1 (2%) MAPCAs | ||
| PM/ICD/ILR/CRT | 16 (34%)/8 (17%)/2 (4%)/1 (2%) | |
| Baseline | 3-year follow-up | |
| Permanent atrial fibrillation | 3 (6%) | 3 (6%) |
| Heart rate (bpm) | 66 ± 11 | 64 ± 12 |
| Systolic BP (mmHg) | 119 ± 12 | 117 ± 12 |
| Diastolic BP (mmHg) | 69 ± 11 | 68 ± 7 |
| 6MWT (mt) | 430 [340–480] | 480 [365–540] |
| Oxygen saturation (%) | 96 ± 3.4 | 96.5 ± 2.1 |
| NYHA class | I 4 pts (8%) | I 17 pts (%) |
| II 39 pts (84%) | II 28 pts (%) | |
| III 3 pts (6%) | III 1 pts (%) | |
| Medications for HF | ||
| ACEi | 35 pts (76%) | 0 |
| ARBs | 11 pts (23%) | 0 |
| ARNI | 0 | 46 pts (100%) |
| SGLT2i | 0 | 23 pts (50%) |
| MRA | 6 pts (13%) | 8 pts (17%) |
| Diuretics | 10 pts (21%) | 6 pts (13%) |
| Pre | Post | |
|---|---|---|
| Bisoprolol | 17 pts (36%)
| 22 pts (47%)
|
| Carvedilol | 6 pts (13%)
| 6 pts (13%)
|
| Metoprolol | 1 pt (2%) 50 mg/daily | 2 pts (4%) 100 mg/daily |
| Sotalol | 3 pts (6%)
| 2 pts (4%)
|
| Amiodarone | 4 pts (8%) 200 mg/daily | 4 pts (8%) 200 mg/daily |
| Flecainide | 2 pts (4%) 100 mg/daily | 2 pts (4%) 100 mg/daily |
| Arrhythmic Burden | Before GDMT 32 Episodes | After GDMT 15 Episodes |
|---|---|---|
| Atrial arrhythmia episodes | 20 episodes
| 8 episodes
|
| Ventricular arrhythmia episodes | 12 episodes
| 7 episodes
|
| Before GDMT | Arrhythmic Events 20 Patients | No Arrhythmic Events 26 Patients | p-Value |
|---|---|---|---|
| Anatomy (d-TGA) | 11 (55%) | 19 (73%) | 0.2 |
| Age (years) | 43.1 ± 11 | 32.5 ± 7 | 0.04 |
| Sex (male) | 12 (60%) | 14 (53%) | 0.6 |
| NT-proBNP (pg/mL) | 459 [307–955] | 162 [106–273] | 0.02 |
| CIED recipients | 9 (45%) | 11 (42%) | 0.8 |
| FAC (%) | 28.2 ± 4.7 | 29.9 ± 6.4 | 0.9 |
| RV GLS (%) | −12.8 ± 2.3 | −13.3 ± 3.8 | 0.7 |
TR severity
| 14 (70%) 6 (30%) | 23 (88%) 3 (12%) | 0.1 |
| Last follow-up | Arrhythmic events 13 patients | No arrhythmic events 33 patients | p-value |
| Anatomy (d-TGA) | 9 (69%) | 21 (63%) | 0.7 |
| Age (years) | 36.6 ± 9 | 37.3 ± 10 | 0.8 |
| Sex (male) | 6 (46%) | 21 (63%) | 0.3 |
| NT-proBNP (pg/mL) | 279 [183–447] | 154 [105–278] | 0.03 |
| CIED recipients | 8 (62%) | 12 (36%) | 0.1 |
| FAC (%) | 33.1 ± 8.7 | 32.7 ± 2.1 | 0.9 |
| RV GLS (%) | −14.4 ± 2.6 | −15.3 ± 2.8 | 0.3 |
TR severity
| 9 (69%) 4 (31%) | 26 (78%) 7 (22%) | 0.5 |
| History of arrhythmic events at baseline | 4 (31%) | 16 (48%) | 0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciriello, G.D.; Altobelli, I.; Fusco, F.; Colonna, D.; Correra, A.; Papaccioli, G.; Romeo, E.; Scognamiglio, G.; Sarubbi, B. Sacubitril/Valsartan and Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Effects on the Arrhythmic Burden. J. Clin. Med. 2024, 13, 7659. https://doi.org/10.3390/jcm13247659
Ciriello GD, Altobelli I, Fusco F, Colonna D, Correra A, Papaccioli G, Romeo E, Scognamiglio G, Sarubbi B. Sacubitril/Valsartan and Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Effects on the Arrhythmic Burden. Journal of Clinical Medicine. 2024; 13(24):7659. https://doi.org/10.3390/jcm13247659
Chicago/Turabian StyleCiriello, Giovanni Domenico, Ippolita Altobelli, Flavia Fusco, Diego Colonna, Anna Correra, Giovanni Papaccioli, Emanuele Romeo, Giancarlo Scognamiglio, and Berardo Sarubbi. 2024. "Sacubitril/Valsartan and Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Effects on the Arrhythmic Burden" Journal of Clinical Medicine 13, no. 24: 7659. https://doi.org/10.3390/jcm13247659
APA StyleCiriello, G. D., Altobelli, I., Fusco, F., Colonna, D., Correra, A., Papaccioli, G., Romeo, E., Scognamiglio, G., & Sarubbi, B. (2024). Sacubitril/Valsartan and Dapagliflozin in Patients with a Failing Systemic Right Ventricle: Effects on the Arrhythmic Burden. Journal of Clinical Medicine, 13(24), 7659. https://doi.org/10.3390/jcm13247659






